Gut Health and Autoimmune Disease Management: Unraveling Their Complex Interactions for Optimal Wellness
Uncover novel ways your microbiome impacts immune balance and disease progression.
In recent years, scientists and clinicians have radically reshaped our understanding of autoimmune disease by highlighting a fundamental connection: the critical role of gut health. This article provides a thorough exploration of the interplay between the gut microbiome and autoimmune disorders, synthesizing current research, mechanisms, and strategies for improving outcomes through targeted interventions.
Table of Contents
- Introduction
- The Gut Microbiome: Foundation of Health
- How Gut Health Influences Autoimmune Disease Mechanisms
- Key Autoimmune Conditions and Their Gut Connection
- Risk Factors and Contributors: What Disrupts Gut Health?
- Diagnosis and Management: Integrative Approaches
- Evidence and Practical Tips for Gut Health Optimization
- Frequently Asked Questions (FAQs)
- References
Introduction
Autoimmune diseases—where the body’s immune system erroneously attacks its own tissues—represent a diverse group of disorders impacting millions worldwide. Traditional management approaches have focused heavily on immune suppression, but a growing body of evidence suggests that the gut might hold the key to both understanding and treating these complex conditions.
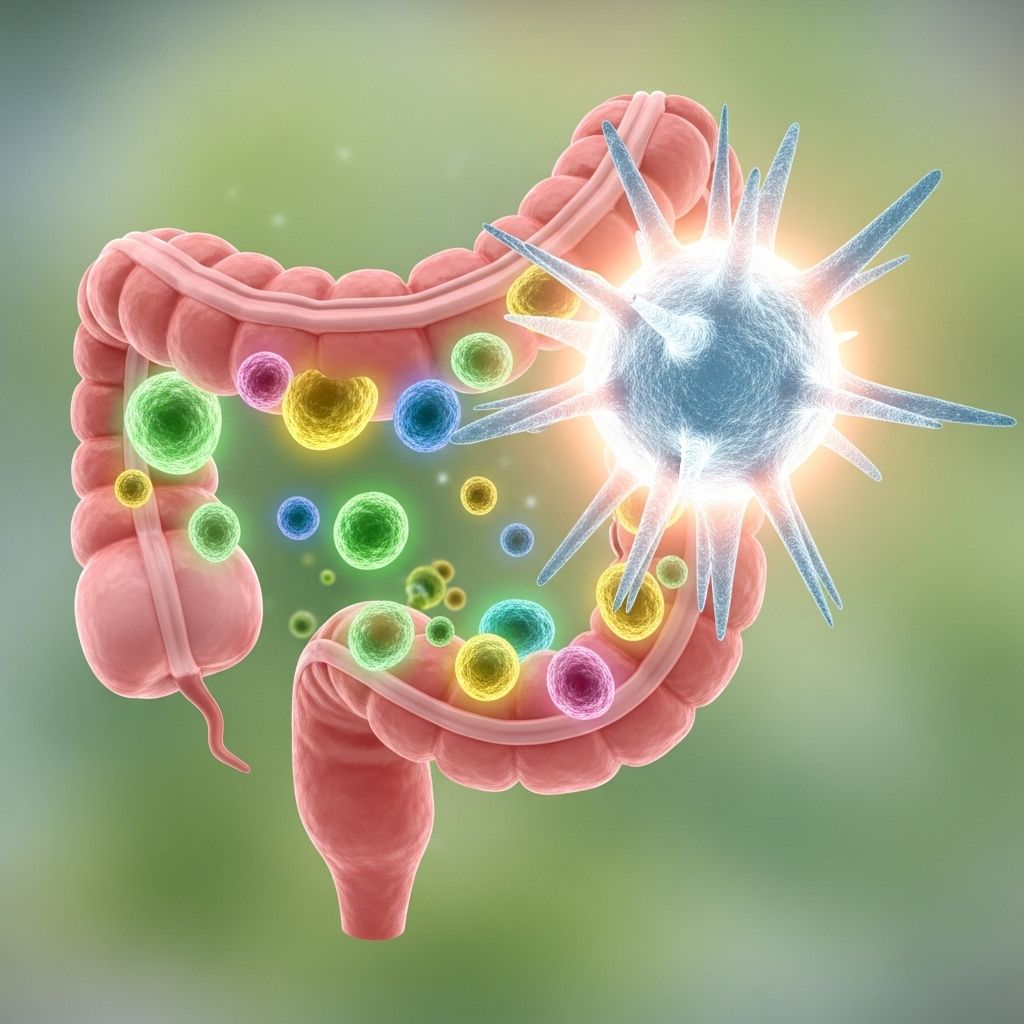
The gut harbors trillions of microorganisms encompassed by the term gut microbiome. Disturbance in the balance of this ecosystem, known as dysbiosis, can lead to chronic inflammation and immune dysfunction, hallmarks of autoimmune conditions. By analyzing the links, mechanisms, and holistic management strategies, individuals and healthcare providers can take proactive steps for improved long-term health outcomes.
The Gut Microbiome: Foundation of Health
The gut microbiome is a dynamic community of bacteria, viruses, fungi, and other microorganisms residing primarily in the intestines. These microbes play essential roles in:
- Digesting food and producing essential vitamins
- Regulating immune system activity
- Maintaining the integrity of the intestinal barrier
- Protecting against harmful pathogens
- Modulating systemic inflammation
Research emphasizes that this ecosystem is integral to immune homeostasis. Beneficial commensal bacteria help create a selective barrier in the gut lining, while disruptions can promote “leaky gut“—a phenomenon where harmful substances pass into the blood, potentially triggering immune reactions.
Table: Key Features of a Healthy vs. Dysbiotic Gut
| Healthy Gut | Dysbiotic Gut |
|---|---|
|
|
How Gut Health Influences Autoimmune Disease Mechanisms
The relationship between the gut and the immune system is bidirectional and intricate. The gut microbiota educates and calibrates the immune response. When microbial diversity is compromised, or harmful bacteria proliferate, it can set the stage for inappropriate immune activation against the body’s tissues.
Main mechanisms linking gut health to autoimmunity include:
- Dysbiosis: Disruption of the normal balance of gut microorganisms. Frequently observed in autoimmune patients and associated with immune system misfiring.
- Increased Intestinal Permeability (Leaky Gut): Damage to the gut barrier allows antigens and toxins to enter the bloodstream, activating systemic immune responses.
- Molecular Mimicry: Certain gut bacteria possess molecular structures similar to host proteins, leading the immune system to produce autoantibodies (e.g. Ro60 in SLE).
- Altered Immune Cell Activation: Changes in the microbiota can regulate immune cell types (e.g., T and B cells), producing abnormal cytokines and autoantibodies.
- Metabolite Influence: Microbial metabolites, such as short-chain fatty acids (SCFAs), modulate immune function and inflammation.
Key Autoimmune Conditions and Their Gut Connection
Numerous autoimmune diseases demonstrate unique links to gut health, either as contributing factors or as results of disease processes.
Inflammatory Bowel Disease (IBD): Crohn’s Disease & Ulcerative Colitis
IBD epitomizes the gut-autoimmune connection—an impaired gut barrier, chronic intestinal inflammation, and pronounced microbial imbalance occur. Crohn’s disease flare-ups, for instance, have been associated with blooms of Ruminococcus gnavus, a bacterium that, while normally present, can exacerbate inflammation when imbalanced.
Celiac Disease
Celiac disease arises when gluten ingestion prompts autoimmune destruction of the small intestine lining, leading to both digestive and systemic symptoms. This condition also increases intestinal permeability and inflammation, establishing a strong link between gut dysfunction and systemic autoimmune activity.
Rheumatoid Arthritis
Emerging research indicates specific gut bacteria can trigger autoimmune responses against joint tissues, often years before clinical symptoms arise. As people age, changes in the microbiome may increase susceptibility to rheumatoid arthritis. This research provides the potential for earlier diagnosis and targeted treatments.
Systemic Lupus Erythematosus (SLE)
Individuals with SLE show decreased gut microbial diversity and elevated levels of specific bacteria (Ruminococcus gnavus) that correlate with disease activity. Molecular mimicry between gut bacteria and host proteins (such as the Ro60 epitope) can provoke pathogenic autoantibodies.
Other Autoimmune Diseases
- Multiple Sclerosis (MS): Gut microbial balance influences neuroinflammation and disease progression.
- Type 1 Diabetes: Early-life dysbiosis may disrupt immune tolerance, increasing disease risk.
- Skin Disorders (Psoriasis, Dermatitis): Gut-mediated immune activation can trigger cutaneous autoimmunity.
Risk Factors and Contributors: What Disrupts Gut Health?
The delicate microbiome ecosystem can become imbalanced due to various environmental, dietary, and lifestyle factors, setting the stage for autoimmune dysfunction.
- Poor Diet: Diets low in fiber, high in processed foods, sugar, or unhealthy fats diminish beneficial bacteria and promote inflammation.
- Antibiotic Overuse: Broad-spectrum antibiotics indiscriminately eradicate both harmful and beneficial bacteria, often leading to dysbiosis.
- Chronic Stress: Stress hormones affect gut lining integrity and microbial diversity.
- Environmental Toxins: Exposure to pollutants, additives, and xenobiotics can impact gut flora and barrier function.
- Genetics: Genetic predispositions can make individuals more susceptible to gut-related immune dysfunction.
- Infections: Both acute and chronic infections can alter the microbiome and promote autoimmune reactivity.
Table: Modifiable vs. Non-Modifiable Gut Health Risk Factors
| Modifiable Factors | Non-Modifiable Factors |
|---|---|
|
|
Diagnosis and Management: Integrative Approaches
Managing autoimmune diseases through the lens of gut health involves both targeted diagnosis and multifaceted therapeutic strategies.
Diagnosis
- Gut Microbiome Analysis: Advanced genetic sequencing and analysis of stool samples can reveal microbial patterns linked to disease states.
- Intestinal Permeability Testing: Functional tests can assess the integrity of the gut lining.
- Comprehensive Blood Panels: Sensitive biomarkers can indicate immune activity, inflammation, and nutrient absorption deficiencies.
Management Approaches
- Dietary Interventions
- Increase intake of fiber-rich foods, prebiotics, and probiotics to foster microbial diversity.
- Eliminate trigger foods (e.g., gluten for celiac disease, processed foods, artificial sweeteners).
- Consider specialized diets (e.g., Mediterranean, anti-inflammatory, elimination diets) based on individual needs.
- Probiotic/Prebiotic Supplementation
- Use targeted probiotic strains supported by research for the specific autoimmune disorder.
- Support probiotics with prebiotic foods (e.g., chicory, onions, garlic).
- Stress Reduction and Mind-Body Practices
- Meditation, yoga, and mindfulness-based stress reduction can support gut integrity.
- Medication Management
- Work with healthcare providers to optimize therapies, minimize gut-disrupting side effects, and monitor responses.
- Lifestyle and Environmental Modification
- Reduce exposure to toxins, maintain regular physical activity, get restorative sleep.
Role of Emerging Therapies
- Fecal microbiota transplantation (FMT) for severe gut dysbiosis
- Personalized, precision medicine using microbiome and genetic analysis
- Biologics targeting both immune and inflammatory pathways
Evidence and Practical Tips for Gut Health Optimization
Current research from the Mayo Clinic, Frontiers in Immunology, and other experts emphasizes:
- Microbiome-targeted interventions can improve disease symptoms and overall wellness.
- Restoring microbiome balance may reduce inflammation and improve immune system tolerance.
- Diet is a cornerstone; regular consumption of whole fruits, vegetables, fermented foods (yogurt, kefir, kimchi), and avoidance of processed items is recommended.
- Avoid long-term or unnecessary antibiotic use unless medically mandated.
- Manage stress through structured programs; chronic stress disrupts gut health demonstrably.
- Monitor autoimmune symptoms closely and respond rapidly to flares—early intervention can prevent long-term complications.
Tips for Supporting a Healthy Gut-Immune Axis
- Eat a wider variety of foods, especially those high in soluble and insoluble fibers.
- Include daily fermented products for live cultures.
- Experiment with elimination diets (under medical guidance) to identify immune triggers.
- Stay hydrated to support cellular and microbial function.
- Pursue gentle movement like walking, yoga, or tai chi to support immune regulation.
Frequently Asked Questions (FAQs)
Q: Can improving gut health cure autoimmune disease?
No current evidence suggests that gut restoration alone can cure autoimmune diseases, but it can significantly improve symptoms, reduce flares, and enhance quality of life.
Q: Are probiotics effective for autoimmune conditions?
Probiotics may benefit some patients, but effectiveness varies depending on the strain and the individual’s clinical profile. Always consult a healthcare provider.
Q: Does “leaky gut” really contribute to autoimmunity?
Research supports that increased intestinal permeability can activate unnecessary immune responses and contribute to autoimmune processes.
Q: How is the gut microbiome tested?
Stool sample analysis using genetic sequencing provides insight into microbial composition, diversity, and potential pathogenic species.
Q: Can diet changes help manage autoimmune disease?
Yes. Anti-inflammatory diets high in plant-based fiber, fermented foods, and low in processed ingredients support microbiome balance and lower inflammation.
References
- BGAPC: Understanding How Digestive Health Impacts Autoimmune Diseases
- Mayo Clinic: Link Between Gut Bacteria and Rheumatoid Arthritis
- PMC: The Dynamic Interplay between the Gut Microbiota and Autoimmune Disease
- Frontiers in Immunology: Emerging Role of Gut Microbiota in Autoimmune Diseases
- Autoimmune Institute: The Relationship Between Autoimmune Disease and Gut Microbiome
References
- https://bgapc.com/the-gut-autoimmune-connection/
- https://individualizedmedicineblog.mayoclinic.org/2023/09/18/mayo-clinic-researchers-identify-link-between-gut-bacteria-and-pre-clinical-autoimmunity-and-aging-in-rheumatoid-arthritis/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6854958/
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1365554/full
- https://www.autoimmuneinstitute.org/articles/the-relationship-between-autoimmune-disease-and-the-gut-microbiome
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4036413/
- https://www.sydney.edu.au/news-opinion/news/2024/09/06/how-the-bugs-in-your-gut-affect-your-immune-system.html
- https://news.yale.edu/2025/02/05/study-reveals-how-gut-bacteria-might-trigger-autoimmune-diseases-lupus
- https://www.lupusresearch.org/researchers-discover-how-gut-bacteria-can-trigger-autoimmunity/
Read full bio of Sneha Tete












