Gut-Brain Axis: How Digestion Shapes Mood, Behavior, and Mental Wellness
Microbial messages can boost emotional balance and clarity through targeted nutrition.
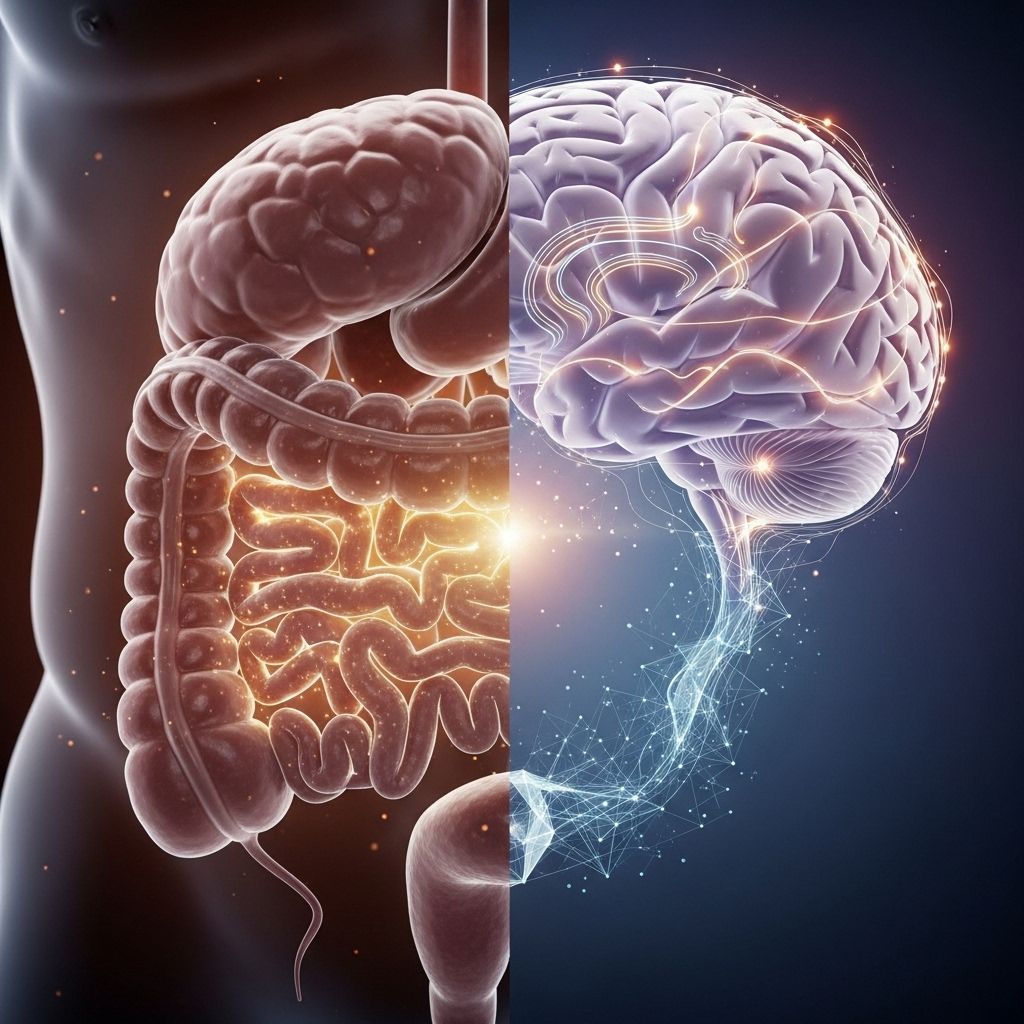
Gut-Brain Axis: Digestion and Mood Connection
Your digestive system does far more than break down food. The relationship between your gut and your brain—a complex, bidirectional communication system known as the gut-brain axis—plays a crucial role in regulating mood, emotions, cognition, and even mental health disorders. Unraveling this relationship reveals new opportunities for improving both digestive and psychological well-being.
Table of Contents
- Introduction: What Is the Gut-Brain Axis?
- Core Components of the Gut-Brain Axis
- How Digestion Influences Mood and Mental Health
- Scientific Evidence Linking Digestion & Mood
- Digestive Disorders and Psychological Symptoms
- How to Support the Gut-Brain AxisStress can have a profound impact on your digestive health, leading to various complications. To delve deeper into how stress affects your gut and to uncover methods for enhancing your well-being, don't miss our comprehensive guide on the impact of stress on digestion and the vagus nerve. This resource reveals vital connections and practical strategies to support both your mental and digestive health.
- Emerging Research & Future Directions
- Frequently Asked Questions (FAQs)
Introduction: What Is the Gut-Brain Axis?
The gut-brain axis is a term for the sophisticated, two-way communication network connecting your digestive tract and your central nervous system. This network includes neural, hormonal, immune, and metabolic signals. The gut-brain axis enables the brain to affect gut function and allows gut health to influence mood and mental processes. In recent years, research has shown that this axis plays a vital role not just in digestion but also in emotional regulation, stress response, and even the risk of psychological disorders.
Core Components of the Gut-Brain Axis
To understand how digestion and mood are linked, it is essential to explore the key pillars of the gut-brain axis:
Nervous System Links
- Central Nervous System (CNS): The brain and spinal cord, overseeing thought, memory, and emotional regulation.
- Enteric Nervous System (ENS): Sometimes called the “second brain,” consisting of a network of neurons governing the digestive tract. The ENS communicates directly with the CNS, often through the vagus nerve, a major conduit of information.
- Bidirectional Communication: The brain can impact gut motility, secretion, and immune activity, while gut-derived signals affect emotional state and cognition.
Endocrine and Immune Interactions
- Endocrine (Hormonal) Signaling: Hormones produced in the gut (like ghrelin and peptide YY) and in the stress-response system (cortisol, via the HPA axis) travel between gut and brain, influencing appetite, energy, and emotional responses.
- Immune System: The gut houses a significant proportion of the body’s immune cells. Cytokines and other immune mediators originating from the gut can cross into the brain and alter neural functioning, affecting mood and behavior—especially when inflammation is present.
Gut Microbiota: The Microbial Players
- Microbiota: Trillions of bacteria, viruses, fungi, and other microbes reside in our digestive tracts, collectively known as the gut microbiota.
- Functions: These microbes are vital for digestion, nutrient absorption, immune regulation, and—most importantly—sending chemical messages that influence the brain.
How Digestion Influences Mood and Mental Health
Through multiple, overlapping systems, the processes of digestion and the state of the gut can have profound effects on how we feel every day.
Neurotransmitters Made in the Gut
- Serotonin: About 90% of the body’s serotonin (a “feel-good” neurotransmitter crucial for mood, sleep, and appetite) is produced in the gut, not the brain. Its production is influenced directly by the gut’s microbiota and the nutrients we consume.
- Dopamine, GABA, and Others: Gut microbes also help produce or modulate neurotransmitters like dopamine (linked to motivation) and gamma-aminobutyric acid (GABA, which calms neural activity).
Microbial Metabolites and Their Effects
- Short-Chain Fatty Acids (SCFAs): These are byproducts produced when gut bacteria digest fiber. SCFAs, such as butyrate, regulate inflammation, reinforce the blood-brain barrier, and affect brain function—potentially reducing anxiety and depressive symptoms.
- Tryptophan Metabolites: Gut microbes break down the amino acid tryptophan (a serotonin precursor), influencing the balance of serotonin and other mood-related chemicals.
Inflammation, Stress, and Mood
- Immune Mediators: Imbalances in gut bacteria (dysbiosis) can prompt the immune system to release pro-inflammatory molecules, which can travel to the brain and effect mood regulation, potentially increasing the risk of depression or anxiety.
- HPA Axis Modulation: The gut-brain axis can activate or mitigate the hypothalamic-pituitary-adrenal (HPA) stress response system, altering levels of stress hormones like cortisol. Chronic stress, in turn, can disrupt both gut and psychological health.
Scientific Evidence Linking Digestion & Mood
A growing body of animal and human research supports direct links between digestive health and mood:
- Mood and GI Disorders: People with chronic digestive conditions like irritable bowel syndrome (IBS) often experience higher rates of anxiety and depression. Conversely, those with mood disorders report more gut complaints.
- Microbiota and Behavior: Animal studies show that both removing and altering gut bacteria can impact anxiety, sociability, and depressive-like behaviors.
- Probiotics and Mood: Several clinical trials reveal that supplementing with live beneficial bacteria (probiotics) can reduce feelings of stress, depressive symptoms, and negative mood states in some people.
Digestive Disorders and Psychological Symptoms
The relationship between digestive disorders and psychological symptoms is particularly strong, suggesting a feedback loop:
| Digestive Disorder | Common Psychological Symptoms | Possible Gut-Brain Axis Role |
|---|---|---|
| Irritable Bowel Syndrome (IBS) | Anxiety, depression, heightened stress, sleep disturbances | Dysbiosis, altered serotonin and stress hormone signaling |
| Inflammatory Bowel Disease (IBD) | Mood fluctuations, fatigue, cognitive fog | Intestinal inflammation, increased cytokine production, barrier dysfunction |
| Functional GI Disorders (e.g., functional dyspepsia) | Somatic symptom disorder, stress sensitivity | Heightened gut sensitivity, ENS and CNS miscommunication |
In each case, disruptions in gut health can trigger or aggravate emotional challenges, while psychological distress can worsen digestive symptoms—a key example of the gut-brain axis in action.
How to Support the Gut-Brain Axis
Understanding this crucial connection highlights actionable steps for improved mood and digestion:
Diet and Nutrition
- Fiber-rich foods: Promote microbial diversity and the production of beneficial SCFAs.
- Fermented foods: Such as yogurt, kefir, kimchi, sauerkraut, and miso, supply live cultures that support a balanced microbiome.
- Limit ultra-processed foods: These can disrupt the gut barrier, promote inflammation, and favor harmful bacteria.
Probiotics and Prebiotics
- Probiotics: Live microorganisms that, when administered in adequate amounts, confer a health benefit by restoring balance in the gut microbiota. Evidence shows certain probiotic strains can reduce negative mood states and stress reactivity.
- Prebiotics: Fibers and compounds (like inulin, fructooligosaccharides) that fuel the growth of beneficial gut bacteria, indirectly impacting mood and well-being.
Lifestyle and Stress Management
- Regular physical activity: Enhances gut motility, supports the microbiome, and lowers inflammation.
- Stress reduction practices: Mindfulness, meditation, yoga, and deep breathing can all calm the gut-brain axis and alleviate both digestive and psychological distress.
- Sleep hygiene: Adequate, regular sleep supports overall gut and brain function.
Emerging Research & Future Directions
Scientists continue to probe the gut-brain axis, revealing its relevance in neurodevelopmental, neurodegenerative, and psychiatric disorders. Future areas of focus include:
- Personalized gut-microbiota interventions: Future therapies may use customized probiotic or prebiotic regimens based on an individual’s unique microbiome profile.
- Fecal microbiota transplantation (FMT): Studies are assessing whether transplanting microbiota from a healthy donor can treat not only gut disorders but also affect mood and behavior.
- Early-life influences: How maternal diet, antibiotic exposure, and early nutrition affect the developing gut-brain axis and later mental health risk.
- Non-invasive diagnostics: Using stool or blood markers as indicators of mental health risk and therapy response.
Frequently Asked Questions (FAQs)
Q: Can anxiety or depression cause digestive symptoms?
Yes. Psychological stress and mood disorders like anxiety and depression can disrupt gut motility, increase sensitivity to pain, and alter the gut microbiota, leading to symptoms such as nausea, diarrhea, constipation, and abdominal discomfort.
Q: Is it possible for improving my gut health to improve my mood?
For many people, yes. Diets rich in fiber and fermented foods, stress management techniques, and targeted probiotic supplements have shown promise in supporting both digestive and emotional well-being. However, individual responses may vary.
Q: What types of probiotic strains are linked to improved mental health?
Certain strains of Lactobacillus and Bifidobacterium have been the most studied for their potential to reduce symptoms of anxiety and depression. It is best to consult a healthcare provider for specific recommendations.
Q: How quickly can dietary or lifestyle changes affect the gut-brain axis?
Improvements can start within days to weeks, especially with dietary changes and probiotic supplementation, but lasting benefits depend on ongoing supportive habits.
Q: Are children’s brain development and behavior affected by the gut-brain axis?
Emerging evidence suggests that the composition of gut microbiota in early life can impact neurological development and potentially influence risk for behavioral and mood disorders later in life.
Understanding the gut-brain axis represents a transformative shift in health. By nurturing our digestive system, we foster not just physical but also emotional and mental resilience—an approach essential for sustaining overall wellness in the modern world.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6469458/
- https://paloaltou.edu/resources/business-of-practice-blog/the-microbiota-gut-brain-axis
- https://www.nature.com/articles/s44184-025-00123-z
- https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection
- https://med.stanford.edu/news/insights/2025/03/gut-brain-connection-long-covid-anxiety-parkinsons.html
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5641835/
Read full bio of medha deb












