Gum Health and Respiratory Infection Risk: Understanding The Crucial Connection
Oral inflammation can send harmful bacteria into your lungs, compromising immune defenses.
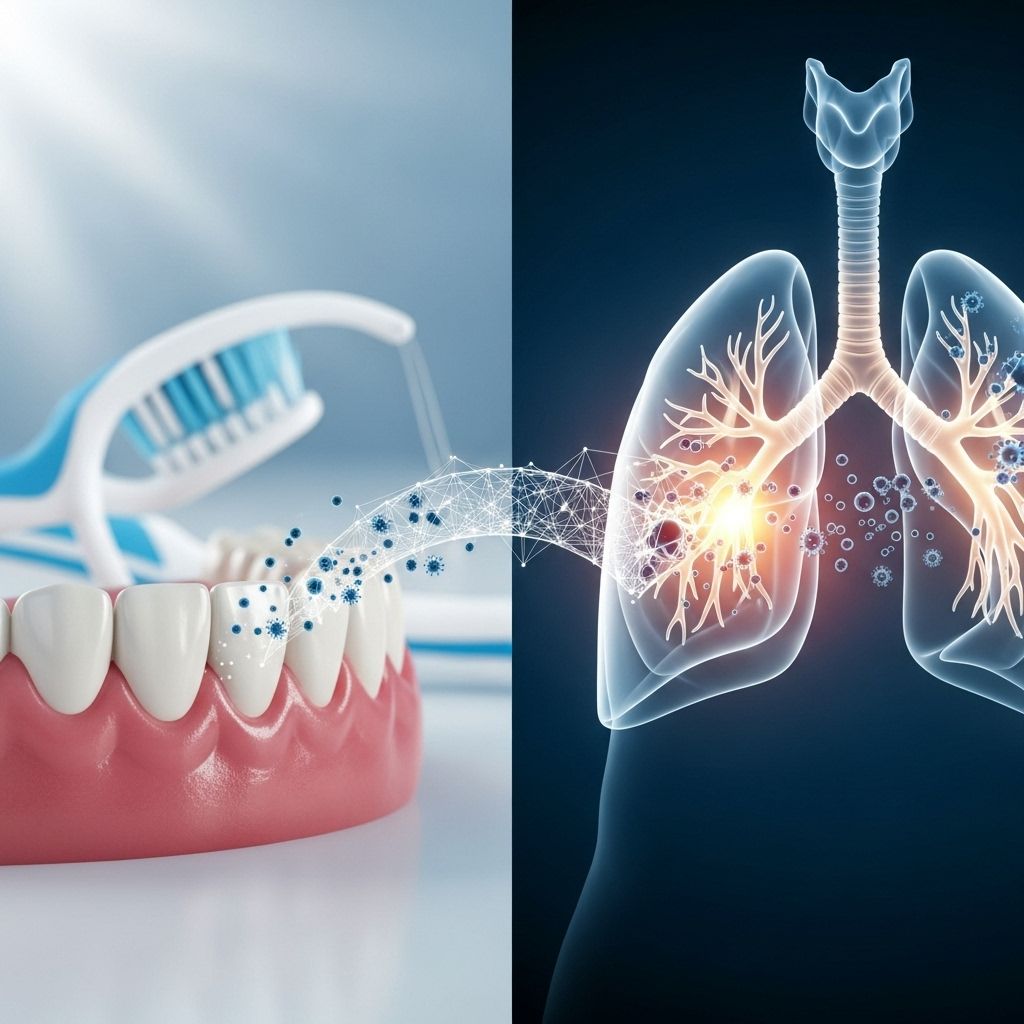
Gum disease is more than a dental problem—it’s increasingly recognized as a significant risk factor for respiratory infections. This in-depth article explores the vital connection between oral health and lung health, revealing how bacteria from the mouth can impact the entire respiratory tract, increasing vulnerability to conditions such as pneumonia, bronchitis, and chronic obstructive pulmonary disease (COPD).
Table of Contents
- Overview: Gum Health and Respiratory Risk
- The Science Behind the Oral-Respiratory Connection
- How Gum Disease Increases Respiratory Infection Risk
- Who is Most at Risk?
- Types of Respiratory Problems Linked to Gum Disease
- Inflammation: A Shared Pathway
- Oral Hygiene and Prevention Strategies
- Gum Disease and Systemic Health: More Than the Lungs
- Current Clinical Evidence
- Frequently Asked Questions (FAQs)
- Conclusion
Overview: Gum Health and Respiratory Risk
The oral cavity is home to hundreds of bacterial species, many of which are harmless or beneficial. However, when gum health is compromised due to inadequate oral hygiene or underlying medical conditions, pathogenic bacteria can flourish. Periodontal disease, also known as gum disease, is a chronic inflammatory condition that destroys the tissues supporting the teeth. Compelling evidence now links active gum disease with a significantly increased risk of respiratory infections, including pneumonia, bronchitis, and COPD.
This connection is particularly relevant for the elderly, hospitalized, or immunocompromised, but anyone with poor gum health is potentially at risk.
The Science Behind the Oral-Respiratory Connection
Researchers have identified several biological mechanisms explaining how gum disease may facilitate respiratory infections:
- Direct Inhalation of Oral Bacteria: When gums are inflamed and bacterial load is high, pathogenic bacteria can be inhaled into the lungs during breathing, particularly during sleep or swallowing.
- Systemic Inflammation: Chronic periodontitis increases circulating pro-inflammatory cytokines (e.g., interleukins), which may lower the respiratory tract’s resistance to infection.
- Biofilm Formation: Oral pathogens may form biofilms in the mouth, which are harder for the immune system to eliminate and can serve as a reservoir for recurrent respiratory infections.
- Immune System Burden: Ongoing oral infection taxes the immune system, reducing its effectiveness throughout the body.
How Gum Disease Increases Respiratory Infection Risk
The two major mechanisms by which gum disease heightens respiratory infection risk are bacterial dissemination and inflammation:
- Bacterial Spread: Oral bacteria from gum disease, including Porphyromonas gingivalis and other anaerobic pathogens, can be directly inhaled, seeding the lower respiratory tract with organisms capable of causing pneumonia and bronchitis.
- Amplified Inflammation: Gum disease triggers local and systemic inflammation, leading to elevated levels of cytokines like interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α). These compounds can worsen the lung’s inflammatory response, facilitating the onset and severity of infection.
This is especially problematic for those with already compromised airway function, such as individuals with asthma or COPD.
Who is Most at Risk?
While anyone with gum disease is at increased risk, certain groups are markedly more vulnerable to respiratory complications arising from poor oral health:
- Elderly individuals: Aging brings decreased immunity and often diminished ability to maintain oral hygiene, making older adults especially susceptible.
- Hospitalized or long-term care patients: Bedridden individuals may practice poor oral hygiene and are at higher risk of both dental and respiratory infections.
- People with chronic respiratory conditions, such as COPD and asthma: Existing inflammation is often compounded by the introduction of oral pathogens, worsening symptoms.
- Immunocompromised patients: People with HIV/AIDS, cancer, or other conditions impairing immunity are less able to fight both dental and pulmonary infections.
- Smokers: Tobacco use is a shared risk factor for both periodontitis and respiratory diseases.
Types of Respiratory Problems Linked to Gum Disease
Oral pathogens and chronic inflammation stemming from gum disease have been linked to several major respiratory illnesses:
- Pneumonia: Bacterial aspiration is a leading cause of community-acquired and hospital-acquired pneumonia, especially among the elderly and those in institutionalized care.
- Chronic Bronchitis: Persistent oral bacteria can enter the bronchi, triggering or worsening chronic bronchitis and associated symptoms.
- Chronic Obstructive Pulmonary Disease (COPD): COPD patients are more susceptible to infection due to existing airway inflammation; poor oral health is associated with increased COPD exacerbations.
- Exacerbation of Asthma and Other Airway Diseases: Inflammatory mediators from gum disease may aggravate airway reactivity and asthmatic symptoms.
Table: Common Respiratory Conditions Linked to Gum Disease
| Condition | Mechanism | Impact |
|---|---|---|
| Pneumonia | Bacterial aspiration from mouth to lungs | Severe infection, especially in elderly |
| Bronchitis | Inflammation and bacterial infection of bronchi | Persistent cough, impaired breathing |
| COPD | Increased airway inflammation and infection risk | Frequent exacerbations, decline in lung function |
| Asthma | Inflammation potentiates airway reactivity | Worsened wheezing and attacks |
Inflammation: A Shared Pathway
Both gum disease and respiratory illnesses are chronic inflammatory conditions. The mouth serves as a gateway for systemic inflammation. In gum disease, the inflamed tissues produce cytokines and inflammatory enzymes that can enter the bloodstream, reaching distant organs such as the lungs.
This systemic inflammatory burden can weaken mucosal defenses in the lungs, making them more susceptible to infections and worsening outcomes for those already dealing with chronic lung diseases.
Oral Hygiene and Prevention Strategies
Maintaining dental and gum health is an important—yet sometimes overlooked—strategy to lower respiratory infection risk. Essential preventive measures include:
- Thorough Brushing and Flossing: Brushing twice daily and flossing removes plaque and reduces bacteria load.
- Routine Dental Checkups: Regular cleanings and professional assessment can detect gum disease at an early, reversible stage.
- Managing Dry Mouth: Adequate saliva helps wash away bacteria; stay hydrated and consider saliva substitutes if needed.
- Smoking Cessation: Quitting smoking reduces the risk for both periodontal and respiratory disease.
- Managing Chronic Illness: Keep conditions like diabetes under control, as high blood sugar can worsen gum disease and impair immune defenses.
- Prompt Treatment: Effectively treating early-stage gum disease can help decrease systemic inflammation and respiratory risks.
Gum Disease and Systemic Health: More Than the Lungs
Poor oral health doesn’t just impact the lungs. Periodontal disease is associated with a range of systemic health problems, including:
- Cardiovascular disease (heart attack, stroke)
- Poor pregnancy outcomes
- Diabetes complications
- Certain cancers
- Impaired bone density and healing
This underscores the importance of a healthy mouth as a foundation for a healthy body.
Current Clinical Evidence
Extensive clinical and epidemiological studies now reinforce the connection between gum health and lung health:
- People with severe periodontal disease are significantly more likely to be diagnosed with a respiratory infection, especially pneumonia and COPD, compared to those with healthy gums.
- Some studies have demonstrated that improving oral hygiene in institutionalized older adults leads to a reduction in rates of hospital-acquired pneumonia.
- During the COVID-19 pandemic, researchers observed that patients with untreated gum disease were more likely to require ventilator support, emphasizing the immune system’s systemic interplay between oral and respiratory health.
- Association is particularly strong in populations with weakened immune systems or additional risk factors (hospitalized, elderly, or chronic illness patients).
Frequently Asked Questions (FAQs)
Q: Can brushing my teeth really lower my pneumonia risk?
A: Yes, good oral hygiene reduces oral bacteria and, as a result, may lower your risk of pneumonia, particularly in elderly or hospitalized individuals, by preventing the aspiration of harmful bacteria into the lungs.
Q: How does gum disease contribute to COPD exacerbations?
A: Periodontal disease increases airway inflammation and exposes the respiratory tract to pathogenic bacteria, both of which are known to trigger COPD exacerbations.
Q: Are antibiotics or mouthwashes enough to prevent respiratory complications?
A: While medicated mouthwashes and, in certain cases, antibiotics can reduce oral bacterial levels, regular mechanical cleaning (brushing, flossing, and professional cleanings) remains essential for long-term prevention. Overuse of antibiotics may lead to resistance.
Q: Is everyone with gum disease at equal risk for respiratory problems?
A: No, risk is higher in those with severe, untreated gum disease and in vulnerable groups such as the elderly, hospitalized, immunocompromised, and smokers.
Q: Can the treatment of gum disease improve lung health?
A: Evidence suggests that successful periodontal treatment can reduce inflammatory markers systemically and potentially lower the risk of lung infections, particularly in those at high risk.
Conclusion
Gum health is an integral part of whole-body wellness. The burden of evidence indicates that maintaining healthy gums can help protect against serious respiratory infections, especially in vulnerable populations. Practicing diligent oral hygiene, seeking regular dental care, and managing risk factors not only preserve your smile but also may provide a critical layer of defense for your lungs and overall health.
References
- https://www.periocenter.com/blog/the-link-between-periodontal-disease-and-respiratory-disease/
- https://www.babylondentalcare.com/general-dentistry/gum-disease-treatment/respiratory-problems/
- https://www.santabarbaradds.com/respiratory-infection
- https://yourolathedentist.com/the-connection-between-oral-health-and-respiratory-issues/
- https://www.kellibradydds.com/periodontal-disease-and-respiratory-disease/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3786481/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3084574/
- https://hackensackdentistsnj.com/blog/how-poor-oral-health-can-affect-your-respiratory-health-the-importance-of-dental-hygiene/
- https://asm.org/press-releases/2024/january/how-gum-disease-aggravates-chronic-obstructive-pul
Read full bio of medha deb












