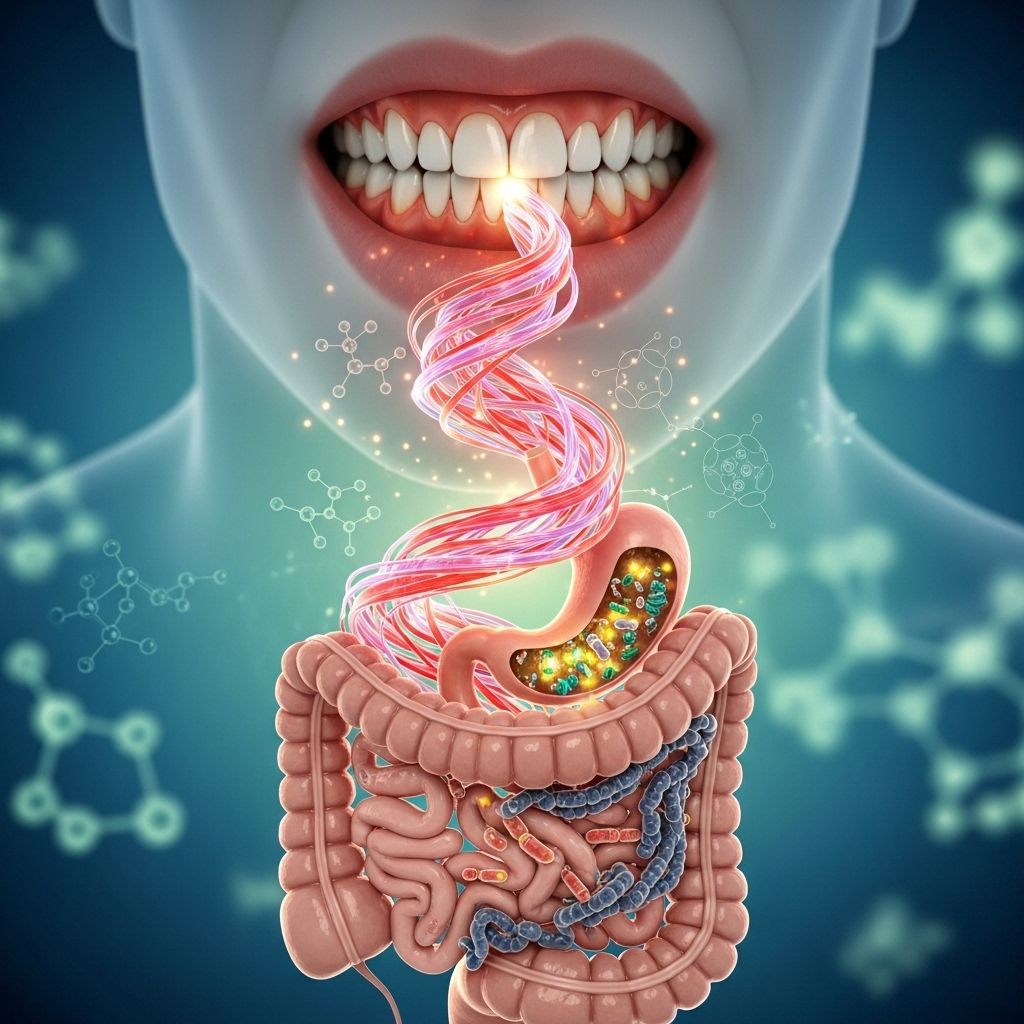
Unveiling the Oral-Gut Axis: How Gum Disease (Periodontitis) Influences Gut Health and Systemic Wellness
Oral inflammation can shape gut microbiota, linking dental health to overall well-being.
nn
Modern research increasingly reveals that health is an interconnected web. Nowhere is this more evident than in the emerging links between gum disease (periodontitis) and gut health. This article explores insights from microbiology, immunology, and gastroenterology to provide a comprehensive overview of the oral-gut axis—demonstrating how periodontal disease may impact gastrointestinal wellbeing and even contribute to systemic conditions beyond the obvious boundaries of the mouth.
nn
Table of Contents
n
- n
- Understanding Gum Disease (Periodontitis)
- Gut Health: Microbiota and Immunity
- The Oral-Gut Axis: Connecting Mouth and Gut
- Mechanisms Linking Periodontitis to Gut Health
- Scientific Evidence of the Gum-Gut Link
- Implications for Systemic Health
- Integrated Care: Oral and Gastrointestinal Collaboration
- Preventive Strategies and Recommendations
- Frequently Asked Questions (FAQs)
- Conclusion
n
n
n
n
n
n
n
n
n
n
nn
Understanding Gum Disease (Periodontitis)
n
Gum disease, medically termed periodontitis, is a chronic inflammatory condition affecting the tissues that support teeth. It is characterized by:
n
- n
- Gingival inflammation (red, swollen, bleeding gums)
- Loss of periodontal ligament and bone (leading ultimately to tooth mobility and loss)
- Caused primarily by bacterial dysbiosis within dental plaque
n
n
n
n
Long considered a localized process, periodontitis has far-reaching effects owing to the mouth’s vascularity and immune connections. Over 50 systemic conditions—including cardiovascular, metabolic, and inflammatory diseases—have been associated with chronic periodontal inflammation.
nn
Key Features of Periodontitis
n
- n
- Chronic, often painless evolution
- Risk factors: genetics, smoking, diabetes, poor oral hygiene
- Bacterial overgrowth: notably Porphyromonas gingivalis, Fusobacterium nucleatum, Aggregatibacter actinomycetemcomitans
- Potential for systemic bacterial spread and inflammatory response
n
n
n
n
nn
Gut Health: Microbiota and Immunity
n
The gut is a complex organ system responsible not just for digestion and absorption, but also immune modulation and systemic homeostasis.
n
What Defines Gut Health?
n
- n
- Microbiota Balance: A diverse, stable microbial community dominated by Bacteroidetes and Firmicutes
- Intestinal Barrier Integrity: Tight junctions keeping pathogens and toxins out of the bloodstream
- Active Mucosal Immunity: Resident immune cells maintain surveillance and tolerance
- Healthy Inflammatory Tone: Low-grade, regulated inflammation; disruption leads to ‘leaky gut’ and disease
n
n
n
n
n
Unhealthy gut states—termed gut dysbiosis—are implicated in metabolic disorders, autoimmunity, liver disease, and even neurodegeneration.
nn
The Oral-Gut Axis: Connecting Mouth and Gut
n
Recent scientific advances reveal a two-way communication system—the oral-gut axis.
n
| Oral-Gut Axis Component | Description |
|---|---|
| Anatomic Continuity | Mouth and GI tract directly connect; saliva, bacteria, and immune cells travel quickly between sites. |
| Microbial Migration | Oral bacteria can reach the gut via swallowing, seeding distant microbial communities. |
| Immune Crosstalk | Inflammatory signals and immune cells can influence both oral and gut immune environments. |
n
This link means disturbances in oral health—especially in the setting of periodontitis—may ripple throughout the digestive tract and beyond.
nn
Mechanisms Linking Periodontitis to Gut Health
n
Several pathways underpin the relationship between periodontal disease and altered gut homeostasis:
n
- n
- Translocation of Oral Bacteria: Swallowed pathogenic oral bacteria, such as P. gingivalis and F. nucleatum, can colonize the gut, shifting microbial balance and potentially promoting gut inflammation.
- Induction of Gut Dysbiosis: Experimental models show that oral administration of periodontal pathogens can induce significant changes in gut bacterial diversity and abundance, leading to increased intestinal permeability (”leaky gut”) and altered immune activation.
- Molecular and Immune Signaling: Chronic oral inflammation can drive systemic inflammation by increasing circulating cytokines like IL-6, exacerbating intestinal and other organ inflammation.
- Breach of Epithelial Barriers: Periodontitis increases endotoxin load and compromises gut tight junctions, facilitating the entry of bacterial products and fueling localized and systemic inflammation.
- Oral Microbiome as a Reservoir: The oral cavity, especially in gum disease, becomes a reservoir for pathogenic bacteria and pro-inflammatory mediators that can influence distant sites.
n
n
n
n
n
nn
Bidirectional Relationship
n
There is increasing evidence for a bidirectional gum–gut axis:
n
- n
- Dysbiosis or chronic inflammation in the gut (e.g., in inflammatory bowel disease) can worsen oral health, further feeding the cycle of disease.
n
nn
Scientific Evidence of the Gum-Gut Link
n
Multiple experimental, clinical, and review studies underpin the mouth-gut connection.
n
Key Studies and Findings
n
- n
- Animal studies: Oral introduction of P. gingivalis in mice disrupts the gut microbiome, increases inflammation, and promotes disease such as arthritis and liver dysfunction. Transfer of gut bacteria from these mice to healthy ones can reproduce disease features.
- Human data: Higher levels of common periodontal pathogens have been found in the stools of patients with inflammatory bowel diseases (IBD) and other gut disorders. The severity of periodontitis appears to correlate with worse gut outcomes.
- Fecal microbiota transplantation (FMT): Restoring gut bacterial diversity via FMT can reverse some pathological features caused by oral bacteria, including liver damage and joint inflammation.
- Liver disease linkage: Oral bacteria associated with periodontitis have been identified as significant contributors to the altered gut flora in patients with liver diseases, suggesting their migration and influence beyond the mouth.
n
n
n
n
n
Table: Clinical Conditions with Evidence Linking Gum Disease and Gut Health
n
| Condition | Oral Involvement | Gut/Extra-Oral Impact |
|---|---|---|
| Inflammatory Bowel Diseases (IBD) | Gingivitis/Periodontitis flares | Worsening of IBD symptoms; increased gut inflammation |
| Rheumatoid Arthritis | Colonization by P. gingivalis | Accelerated joint destruction via gut dysbiosis |
| Liver Disease (NAFLD, Cirrhosis) | Periodontal pathogens migrate to gut | Aggravated liver inflammation, changes in bile acid metabolism |
nn
Implications for Systemic Health
n
The oral-gut axis has consequences well beyond digestive health. Dysregulated oral and gut microbiomes serve as mediators between periodontal disease and broader systemic disorders:
n
- n
- Metabolic Diseases: Periodontitis-induced inflammation impairs insulin signaling; oral pathogens contribute to metabolic endotoxemia.
- Liver Disease: Oral bacteria alter gut barrier and microbiota, impacting liver inflammation and biochemistry. Periodontal therapy has shown improvements in markers of liver disease and patient quality of life.
- Atherosclerosis and Cardiovascular Disease: Inflammation originating in periodontal tissues can contribute to vascular dysfunction via systemic immune activation and microbial components in circulation.
- Autoimmune and Rheumatic Disorders: Altered gut immune environments triggered by oral bacteria may promote chronic joint and tissue inflammation.
n
n
n
n
nn
Integrated Care: Oral and Gastrointestinal Collaboration
n
Given these links, collaborative care between dental and gastrointestinal (GI) practitioners is crucial:
n
- n
- Shared assessment protocols: Screening patients with chronic gut or liver disease for oral health problems, and vice versa.
- Integrated therapeutic approaches: Periodontal treatments can modulate systemic and local inflammation, benefiting gut health; gastroenterologists should recognize oral symptoms as possible contributors to disease progression.
- Research synergy and communication: Joint research and clinical management can optimize outcomes for patients with intersecting oral and gastrointestinal disorders.
n
n
n
nn
Preventive Strategies and Recommendations
n
- n
- Routine oral hygiene: Brushing, flossing, and regular professional cleaning to limit dysbiosis.
- Screening and early intervention: Early detection and management of periodontitis in patients with known GI, liver, or autoimmune diseases.
- Dietary optimization: Fiber-rich diets support both oral and gut microbial health.
- Probiotics and prebiotics: Ongoing research investigates roles for targeted supplementation in restoring microbial balance.
- Smoking cessation: Smoking is a shared risk factor worsening both gum and gut health.
- Medical-dental coordination: Encourage communication among healthcare teams about patient oral and gut health status.
n
n
n
n
n
n
nn
Frequently Asked Questions (FAQs)
n
Q: How do oral bacteria reach the gut?
n
A: Pathogenic bacteria from periodontal pockets can be swallowed with saliva, traveling through the digestive tract and potentially colonizing or altering gut microbial communities.
n
Q: Can treating gum disease improve gut health?
n
A: Evidence suggests that periodontal therapy can restore both oral and gut microbiota balance, reduce systemic inflammatory markers, and improve related symptoms in liver and digestive diseases, though more research is needed on long-term organ outcomes.
n
Q: Are some people more at risk for gum-gut problems?
n
A: Yes. Patients with chronic inflammatory diseases (e.g., IBD, autoimmune disorders), poorly controlled diabetes, or liver disease are at higher risk and should be monitored closely for oral-systemic interactions.
n
Q: Is the relationship between gum disease and gut health one-way?
n
A: No, the gum–gut axis is bidirectional; changes in gut microbiota and chronic gut inflammation can also worsen oral disease and vice versa.
n
Q: What’s the best way to protect overall health?
n
A: Maintain excellent oral hygiene, seek regular dental and medical checkups, follow an anti-inflammatory diet, and address risk factors like smoking and poorly controlled systemic diseases.
nn
Conclusion
n
The concept of the oral-gut axis heralds a new era in understanding human health—where gum disease is not merely a local problem but a potential contributor to gut dysbiosis, systemic inflammation, and multi-organ disease. Evidence highlights the importance of maintaining oral health as an essential pillar of total well-being, warranting integrated care pathways and preventive strategies. Continued research promises to reveal even deeper connections, underscoring the need for collaboration among dental, medical, and gastroenterology professionals for the benefit of patients worldwide.
n
References
Read full bio of Sneha Tete












