Genetics of Skin Circulation: Exploring How Your Blood Flow is Shaped by DNA
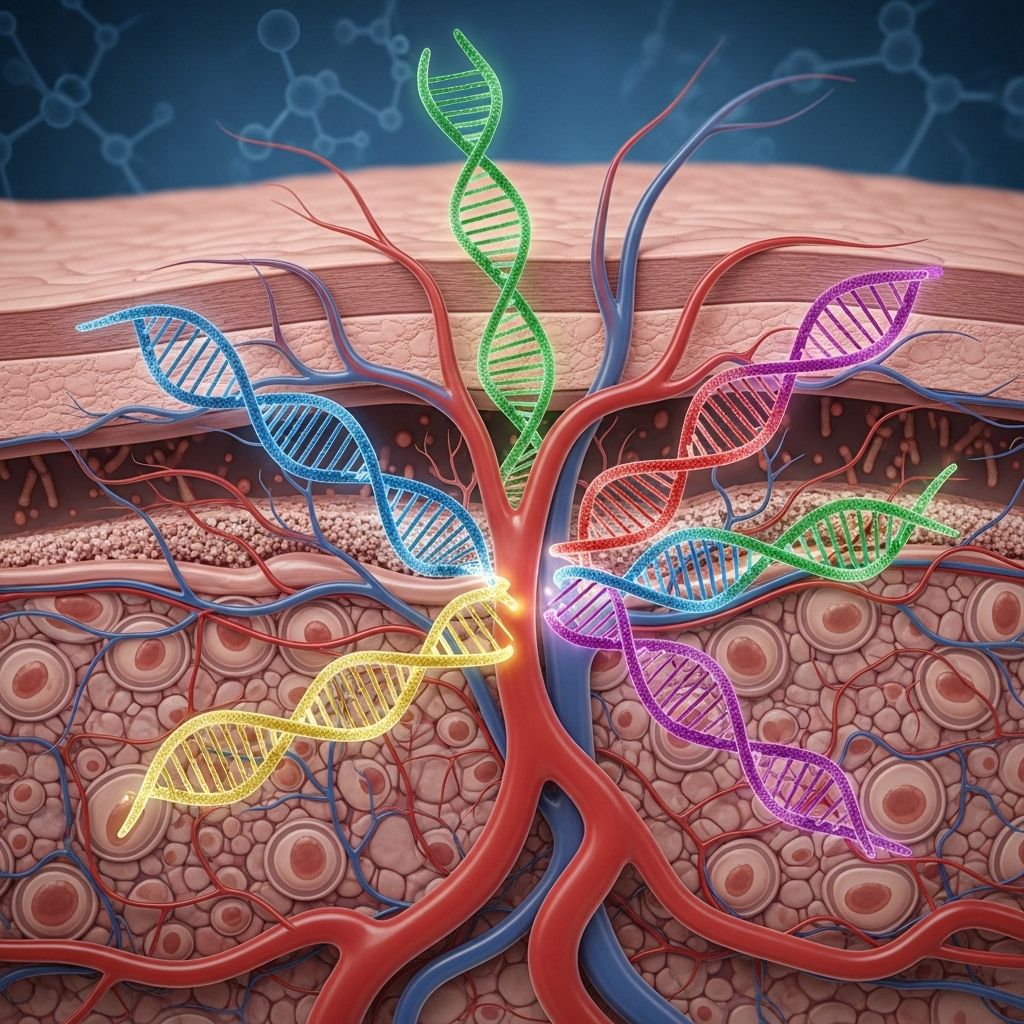
DNA clues reveal why your skin’s microvessels respond uniquely to heat and cold.
Genetics of Skin Circulation: Understanding Your Blood Flow
Skin microcirculation—the flow of blood through the skin’s intricate network of vessels—is critical not only for temperature regulation and nutrient delivery, but also for determining individual risk for vascular and metabolic diseases. Recent advances in genetics are revealing how our DNA governs the function of these tiny vessels, shaping both our physiological responses to the environment and our predisposition to disease. This comprehensive article explores the genetic basis of skin blood flow, examining how genes influence microvascular structure, function, and adaptation.
Table of Contents
- Introduction: Why Skin Circulation Matters
- Skin Microcirculation: Anatomy and Core Functions
- How Is Skin Blood Flow Regulated?
- The Role of Genetics in Skin Circulation
- Key Genetic Variants Affecting Skin Blood Flow
- Genetics, Skin Circulation, and Thermoregulation
- Aging, Genes, and Skin Circulatory Adaptation
- Genetics of Skin Microcirculation and Disease Risk
- Emerging Research Directions
- Frequently Asked Questions
- Conclusion
Introduction: Why Skin Circulation Matters
Few organs reveal the interplay of systemic health and genetics as visibly and dynamically as the skin. Through its rich vascular network, human skin serves as a barrier, heat regulator, and an early warning system for systemic vascular health. Robust skin blood flow is crucial for:
- Thermoregulation – balancing heat loss and retention in response to environmental temperature.
- Nutrient and Oxygen Delivery – supporting cellular health and barrier repair.
- Immune Response – mediating inflammation and pathogen defense.
- Wound Healing – facilitating repair after injury or infection.
Yet, individuals show wide variability in skin vascular reactivity, susceptibility to cold or heat, and rates of skin-related complications—all shaped by a blend of environmental factors and genetic inheritance.
Skin Microcirculation: Anatomy and Core Functions
The skin’s microvascular system consists of networks of arterioles, capillaries, and venules, forming two primary plexuses: a superficial network close to the skin surface, and a deeper plexus in the dermis. Key features include:
- Arterioles: Regulate blood flow and tissue perfusion through constriction and dilation.
- Capillaries: Main site of oxygen and nutrient exchange, running in perpendicular loops from the superficial plexus.
- Venules: Drain deoxygenated blood back toward systemic circulation.
The skin is the body’s largest organ—its ability to constrict or dilate blood vessels rapidly is vital for immediate adaptations to environmental changes, such as moving from cold outdoors to a warm room.
How Is Skin Blood Flow Regulated?
Skin circulation is regulated by an array of neurovascular and endothelial mechanisms:
- Sympathetic Nervous System:
- Noradrenergic Vasoconstriction: Activation causes arteriolar tightening, reducing blood flow (e.g., cold response).
- Cholinergic Vasodilation: Less prominent in skin, but mediates active dilatation during heat exposure.
- Axon Reflexes: Local neural circuits using C-fiber nerve endings release vasoactive neuropeptides (substance P, CGRP) for rapid responses to local heating or injury.
- Endothelial Factors:
- Nitric Oxide (NO): Potent vasodilator, largely responsible for plateau phase of heat-induced skin blood flow increase.
- Prostacyclin, Endothelin: Additional mediators balancing dilation and constriction.
- Myogenic Response: Local vascular smooth muscle reactions to pressure or stretch—more pronounced in glabrous (hairless) skin.
- Hormonal and Local Metabolic Influences: Insulin, angiotensin, and hypoxia can locally modulate skin blood flow.
These systems are coordinated but differ in dominance based on skin region (e.g., glabrous palms/soles vs. hairy limbs) and environmental or physiological demands.
The Role of Genetics in Skin Circulation
While environment (climate, health status, physical fitness) alters skin vascular function, genetic factors have a profound and measurable influence:
- Heritability of Vascular Traits: Twin and family studies show skin blood flow responses—such as maximum dilatory capacity and cold-induced vasoconstriction—exhibit moderate to strong heritability, suggesting a significant genetic underpinning.
- Gene Expression in Skin: Genes shape the abundance and sensitivity of neurotransmitter receptors, endothelial enzymes mediating nitric oxide production, and the architectural development of skin microvessels.
- Ethnic and Population Differences: Documented differences in skin microcirculatory responses among populations reflect polymorphisms in key regulatory genes.
Genetic research is rapidly uncovering which specific genes and polymorphisms help explain why two people of similar health and fitness may react very differently to heat, cold, or vascular stress.
Key Genetic Variants Affecting Skin Blood Flow
Among the myriad genes influencing skin microcirculation, several key players stand out:
| Gene/Enzyme | Main Effect | Polymorphism Impact |
|---|---|---|
| eNOS (NOS3) | Encodes endothelial nitric oxide synthase, crucial for NO-mediated vasodilation | Variant G894T (Glu298Asp) linked to reduced NO, blunted flow responses |
| ACE | Angiotensin-converting enzyme regulates vasoconstriction | Insertion/deletion (I/D) variant influences skin vasomotor tone |
| ADRB2 | Beta-2 adrenergic receptor, affects vasodilatory signal in response to catecholamines | Polymorphisms like Gly16Arg and Gln27Glu alter vasodilation capacity |
| EDN1 | Encodes endothelin-1, a vasoconstrictor peptide | Coding variants associated with increased vasoconstriction, hypertension risk |
| TRPV1/TRPM8 | Transient receptor potential channels involved in thermal and pain sensation | Functional polymorphisms modulate thermal sensitivity and vascular reflexes |
Polymorphisms in these and other genetic loci explain population variance in skin perfusion, especially in stress responses such as cold exposure, exercise, or sustained heat.
Genetics, Skin Circulation, and Thermoregulation
Thermoregulation is one of the clearest areas where genetic differences in skin circulation matter on a daily basis:
- Individuals with genetically determined robust vasodilatory potential are less prone to heat stress—they dissipate heat faster and are less susceptible to heat stroke.
- Genetic variants reducing nitric oxide availability blunt the skin’s ability to increase flow during heat or exercise, raising risk for overheating.
- In contrast, enhanced vasoconstrictor responses are beneficial in cold environments—protecting against hypothermia, but also posing risk of frostbite or Raynaud’s phenomenon in susceptible genotypes.
- Ethnic differences in prevalent polymorphisms may explain why certain populations demonstrate lower baseline skin blood flow or higher rates of cold-related circulatory disturbances.
This area also underlies individual sport performance: athletes with favorable genotypes sustain higher skin blood flow during exertion, aiding in rapid dissipation of metabolic heat.
Aging, Genes, and Skin Circulatory Adaptation
Aging is a potent modifier of skin blood flow, with most individuals experiencing a 25–50% reduction in maximal skin perfusion by age 70, even in the absence of disease. Genes interact with age-related changes in several major ways:
- Reduction in NO Production: Genetic variants in eNOS or genes regulating substrate (L-arginine) and cofactor (BH4) availability can worsen the age-related decline in endothelial function.
- Altered Sympathetic Function: Age-driven changes in neurotransmitter synthesis and receptor sensitivity are compounded by polymorphisms in adrenergic and cholinergic pathway genes.
- Vascular Remodeling Genes: Genes involved in collagen, elastin, and angiogenesis modify the skin’s microvascular structure, influencing the rate and severity of aging-associated circulatory decline.
These factors collectively determine individual variation in age-related vulnerability to cold injuries, wound healing complications, and heat intolerance.
Genetics of Skin Microcirculation and Disease Risk
Genetic determinants of skin blood flow are directly linked to risk and presentation of several diseases:
- Raynaud’s Phenomenon: Multiple gene variants, especially in adrenergic pathways, contribute to excessive skin vasoconstriction and cold-triggered ischemia. Family clustering is often observed.
- Scleroderma and Connective Tissue Disorders: Genetic risk for impaired angiogenesis and autoimmunity underlies microvascular dysfunction in affected individuals.
- Diabetes Mellitus: Polymorphisms in genes regulating NO production, oxidative stress response, and endothelin pathways contribute to increased risk of impaired skin perfusion, ulcers, and delayed wound healing.
- Cardiovascular Disease: Skin microcirculation is a window into systemic vascular health; shared genetic determinants influence endothelial function, atherosclerosis risk, and overall vascular reactivity.
- Heat and Cold Intolerance Syndromes: Genetic defects in thermosensitive channels (e.g., TRPM8) or in neurotransmitter release lower an individual’s adaptive range.
Identifying at-risk genotypes can enable personalized care—such as tailored prevention or enhanced monitoring for individuals with a strong predisposition.
Emerging Research Directions
- Genome-wide Association Studies (GWAS): Large-scale research is pinpointing new gene loci (including non-coding RNAs) regulating vascular function in the skin.
- Epigenetic Modulation: Environmental exposures (sun, toxins, stress) can alter the expression of key vascular genes, influencing skin circulation independent of inherited DNA sequence.
- Personalized Medicine: Genetic profiling could eventually guide individualized skin health strategies, especially for athletes, individuals with chronic diseases, and those exposed to extreme climates.
- Novel Therapeutic Targets: Drugs designed to enhance or block specific signaling pathways in genetically at-risk individuals may prevent disease progression or limit adverse reactions to environment.
Frequently Asked Questions (FAQs)
Q: Can genetic testing reveal if I’m at risk for poor skin circulation?
A: Some advanced genetic panels include major variants affecting skin vascular function, but this area remains largely research-focused. While genetics can suggest predisposition, environmental factors and health status remain highly influential.
Q: Why do some people get cold hands and feet more easily than others?
A: This trait is influenced by both genetics and lifestyle. Genes affecting sympathetic nervous system sensitivity and vasoconstrictive signaling often underlie these differences.
Q: Can I improve my skin blood flow through exercise and healthy living, even if my genes aren’t favorable?
A: Yes, regular aerobic exercise, good nutrition, and avoiding smoking can enhance overall vascular health and modulate many of the impacts of less favorable genetics.
Q: Are certain populations or ethnicities more likely to have robust skin blood flow?
A: Population differences exist, with certain genetic variants being more or less common by ancestry, impacting average skin blood flow, cold tolerance, and responses to environmental stressors.
Conclusion
The genetics of skin circulation bridge the fields of dermatology, cardiovascular medicine, and genetics, revealing how our DNA shapes one of the most vital—and visible—microvascular systems in the body. Through a deepening understanding of gene-environment interactions, new frontiers in personalized vascular health and precision skin therapies are emerging—mapping the next generation of research and care in the field of microcirculation.
References
Read full bio of Sneha Tete












