Gallstones and Unexplained Post-Meal Bloating: Understanding Causes, Symptoms, Diagnosis, and Treatment Options
A deeper look at why fatty meals trigger discomfort and strategies to ease digestion.
Unexplained bloating after meals can perplex and frustrate patients and healthcare providers alike. One of the often-overlooked causes is the presence of gallstones. Gallstones can silently form in the gallbladder, sometimes triggering digestive distress, particularly post-meal bloating, a sensation of fullness, and discomfort. This comprehensive guide explores the critical link between gallstones and post-meal bloating, the underlying mechanisms, distinguishing symptoms, diagnostic processes, and the best current management strategies for patients experiencing these complaints.
Table of Contents
- Introduction to Gallstones
- Understanding the Gallbladder
- Gallstones and Their Impact on Digestion
- Symptoms of Gallstones, Including Bloating
- Mechanisms Linking Gallstones and Post-Meal Bloating
- Risk Factors and Causes of Gallstones
- Diagnosing Gallstones in Patients with Bloating
- Treatment Options for Gallstones and Related Bloating
- Dietary and Lifestyle Tips for Prevention and Management
- When to Seek Medical Attention
- Frequently Asked Questions (FAQs)
Introduction to Gallstones
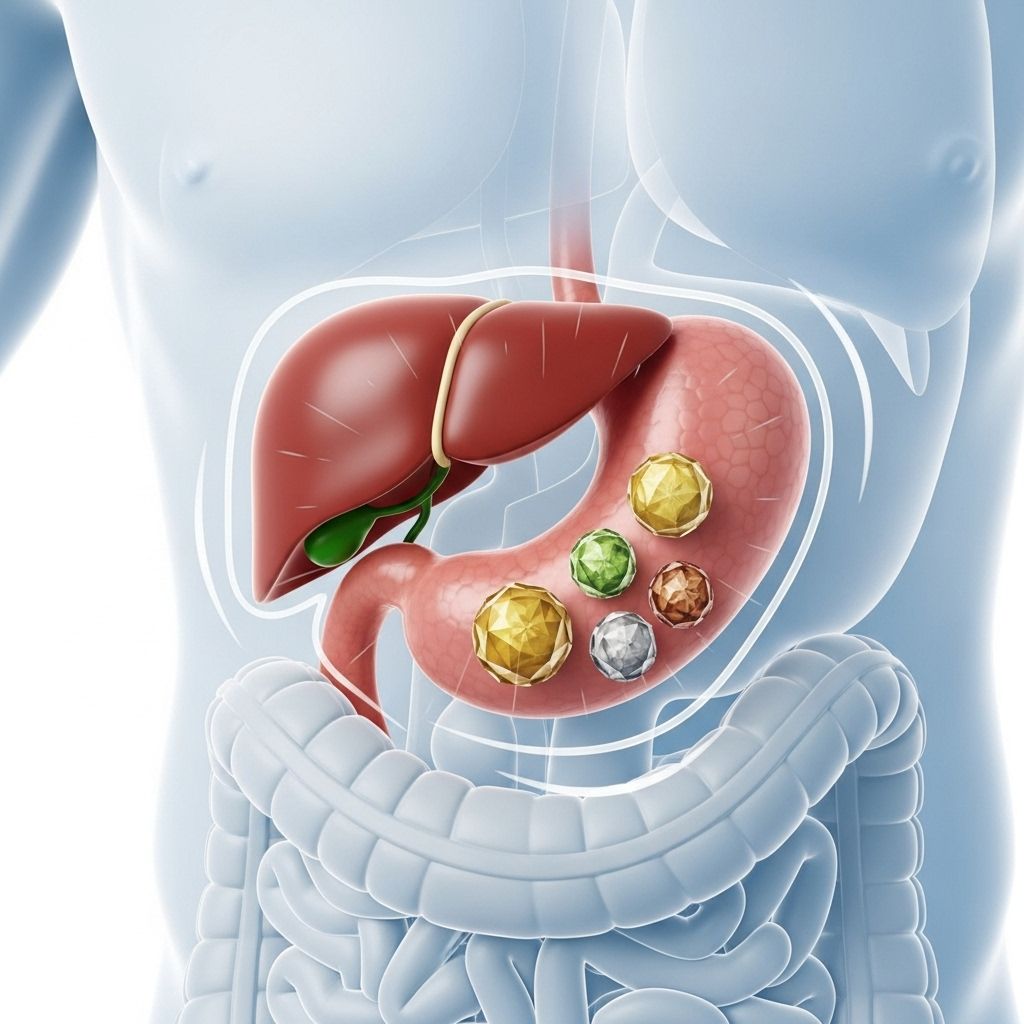
Gallstones are hardened deposits that form from components of bile, primarily cholesterol or bilirubin, within the gallbladder. Though common and often silent, they may provoke significant digestive symptoms, especially when obstructing the flow of bile, a crucial component of normal fat digestion and absorption.
Understanding the Gallbladder
The gallbladder is a small, pear-shaped organ beneath the liver. Its function is to store and concentrate bile produced in the liver, releasing it into the small intestine after meals—especially meals rich in fat. Bile aids in fat digestion, promoting nutrient absorption and normal gut function.
Gallstones and Their Impact on Digestion
When gallstones develop, they may either remain asymptomatic (silent gallstones) or block the bile ducts, especially after food intake, triggering digestive problems. A key symptom is post-meal bloating, sometimes accompanied by upper abdominal pain, nausea, or discomfort. The underlying issue is the obstruction or impaired release of bile, which disrupts fat digestion and leads to various symptoms.
Symptoms of Gallstones, Including Bloating
The presentation of gallstones can range dramatically:
- Bloating—one of the most frequently reported symptoms, may be especially noticeable after high-fat meals.
- Upper right abdominal pain—often severe, occurring minutes to hours after eating.
- Nausea or vomiting, sometimes without explanation, particularly after meals.
- Pain radiating to the right shoulder or between the shoulder blades.
- Jaundice (yellowing of skin or eyes) if bile flow is severely blocked.
- Fever or chills in cases of infection or inflammation.
- Changes in stool and urine color, such as light-colored stools or tea-colored urine.
Sustained, severe, or recurring symptoms, particularly if associated with fever or jaundice, signal a potential complication and merit urgent medical evaluation.
Mechanisms Linking Gallstones and Post-Meal Bloating
The relationship between gallstones and bloating after meals is rooted in bile flow obstruction:
- Gallstones can get temporarily lodged in the neck of the gallbladder or the bile ducts, blocking the release of bile during digestion.
- This disruption to bile flow causes improper digestion of fats, leading to incomplete breakdown and fermentation of nutrients in the gut.
- Fatty foods, which rely heavily on bile for digestion, can be particularly problematic and trigger both bloating and abdominal discomfort post-meal.
- Repeated episodes of obstruction and release may lead to chronic inflammation of the gallbladder (chronic cholecystitis), further impairing digestion and contributing to persistent bloating.
In addition to direct blockages, sluggish emptying of the gallbladder—a condition sometimes associated with gallstones—can amplify these symptoms, even in the absence of continuous stone obstruction.
Risk Factors and Causes of Gallstones
Several factors increase the likelihood of gallstone formation, including:
- Excess cholesterol in bile—often linked to obesity, metabolic syndrome, certain diets, and rapid weight loss.
- Increased bilirubin—due to certain blood disorders or liver diseases.
- Insufficient bile salts for cholesterol dissolution.
- Impaired gallbladder emptying, which allows bile to concentrate and crystallize.
Risk factors for developing gallstones include:
- Family history of gallstones
- Female sex
- Age over 40 years
- Poor diet or rapid weight loss
- Certain medical conditions (e.g., diabetes, liver disease)
- Pregnancy
- Prolonged fasting
Diagnosing Gallstones in Patients with Bloating
The diagnosis of gallstones in individuals with unexplained post-meal bloating involves a combination of clinical evaluation and diagnostic imaging:
- Detailed medical history and review of symptoms
- Physical examination, focusing on abdominal tenderness and signs of gallbladder inflammation (e.g., positive Murphy’s sign)
- Laboratory blood tests to assess liver enzymes, bilirubin, and inflammation markers
- Imaging studies—most commonly abdominal ultrasound—are highly effective for detecting gallstones, gallbladder wall thickening, and duct dilation
- Further imaging (CT scan or MRI) may be warranted if complications or alternative diagnoses are suspected
Timely identification is crucial, especially if infection, pancreatitis, or other serious complications (such as biliary obstruction with jaundice) are suspected.
Treatment Options for Gallstones and Related Bloating
Treatment is guided by the frequency, severity, and impact of symptoms, as well as the presence of complications:
- Observation: Asymptomatic (silent) gallstones usually require no treatment. Many people have gallstones their entire life without issues.
- Surgical removal of the gallbladder (cholecystectomy): This is the most common and effective treatment for symptomatic gallstones, with minimally invasive (laparoscopic) surgery preferred. Removing the gallbladder usually resolves repeated episodes of pain and bloating.
- Medications: Oral medications to dissolve cholesterol gallstones are available, but rarely used due to their limited effectiveness, lengthy course, and high recurrence after discontinuation.
- Treating complications: If signs of infection, pancreatitis, severe jaundice, or duct obstruction occur, hospitalization, intravenous antibiotics, endoscopic interventions, or emergency surgery may be required.
| Treatment | Ideal For | Pros | Cons |
|---|---|---|---|
| Observation | Silent gallstones, no symptoms | No risks or interventions required | Symptoms may develop later |
| Laparoscopic Cholecystectomy | Most patients with symptoms | Definitive; rapid symptom relief | Standard surgical risks; rare post-surgery diarrhea |
| Medications | Poor surgical candidates with cholesterol stones | Non-surgical | Slow; high risk of recurrence |
Dietary and Lifestyle Tips for Prevention and Management
Diet and lifestyle modifications are important for both reducing risk and managing symptoms:
- Adopt a balanced, fiber-rich diet with moderate fat intake and avoid large amounts of fried or fatty foods.
- Maintain a healthy weight; avoid rapid weight loss or crash diets, which can increase gallstone risk.
- Exercise regularly—at least 30 minutes of moderate activity most days of the week.
- Stay hydrated and limit processed foods.
- If you have had your gallbladder removed, consume smaller, more frequent meals with lower fat content to minimize temporary digestive symptoms.
When to Seek Medical Attention
Certain symptoms associated with gallstones and post-meal bloating require urgent evaluation. Seek immediate medical care if you experience:
- Severe, persistent upper abdominal pain lasting more than a few hours
- Pain associated with fever or chills
- Yellowing of the skin (jaundice) or eyes
- Vomiting that does not resolve
- Light-colored stools or dark, tea-colored urine
These symptoms may indicate a more serious problem, such as acute cholecystitis (gallbladder inflammation), cholangitis (infection of the bile ducts), or pancreatitis, each of which can be life-threatening if left untreated.
Frequently Asked Questions (FAQs)
Q: Can gallstones cause bloating after eating even if there’s no pain?
A: Yes, gallstones can cause bloating and fullness even in the absence of classic gallstone pain. In some cases, the obstruction is partial or intermittent, leading to subtler symptoms like bloating and indigestion, especially after high-fat meals.
Q: What foods should I avoid if I have gallstones and experience bloating?
A: It’s advisable to limit fatty, fried, and processed foods. Eating smaller meals and avoiding rapid weight loss can also help manage symptoms. High-fiber content and a moderate fat intake support healthy digestion and may reduce gallstone risk.
Q: Is it possible for gallstones to resolve without surgery?
A: Most gallstones do not dissolve spontaneously. In a small subset of patients with cholesterol stones, oral medications can help dissolve stones, but the process is slow, and recurrence is common. Surgery remains the gold standard for symptomatic cases.
Q: How is gallbladder removal surgery performed and what is recovery like?
A: Gallbladder removal is typically done laparoscopically, involving small incisions and the use of a camera. Most patients return home the same day, recover quickly, and can resume normal activity within a week. Some may experience mild, temporary diarrhea as their body adapts.
Q: Are there long-term digestive problems after gallbladder removal?
A: Most people digest food normally after surgery, with few lasting issues. A minority experience changes in bowel habits or mild indigestion, which usually improves over time with dietary adaptations.
Key Takeaways
- Gallstones are a common but sometimes overlooked cause of unexplained post-meal bloating.
- Symptoms typically include bloating, abdominal pain, and digestive discomfort after high-fat meals.
- Careful evaluation and imaging can confirm the diagnosis, and treatment options depend on symptom severity.
- Lifestyle and dietary adjustments play a significant role in both prevention and management.
- Prompt medical attention is critical if pain, fever, or jaundice develops, signaling potential complications.
References
- https://www.niddk.nih.gov/health-information/digestive-diseases/gallstones/symptoms-causes
- https://www.aurorahealthcare.org/services/gastroenterology-colorectal-surgery/gallstones
- https://my.clevelandclinic.org/health/diseases/22976-gallbladder-disease
- https://www.mayoclinic.org/diseases-conditions/gallstones/diagnosis-treatment/drc-20354220
- https://healthcare.utah.edu/general-surgery/gallbladder
- https://my.clevelandclinic.org/health/diseases/7313-gallstones
- https://www.mayoclinic.org/diseases-conditions/gallstones/symptoms-causes/syc-20354214
- https://www.nhs.uk/conditions/gallstones/
- https://www.pennmedicine.org/conditions/gallstones
Read full bio of Sneha Tete












