Deciphering the Fructose-Uric Acid-Hypertension Pathway: Mechanisms, Impact, and Clinical Insights
A look at how sugar metabolism impairs vessel function and elevates blood pressure.
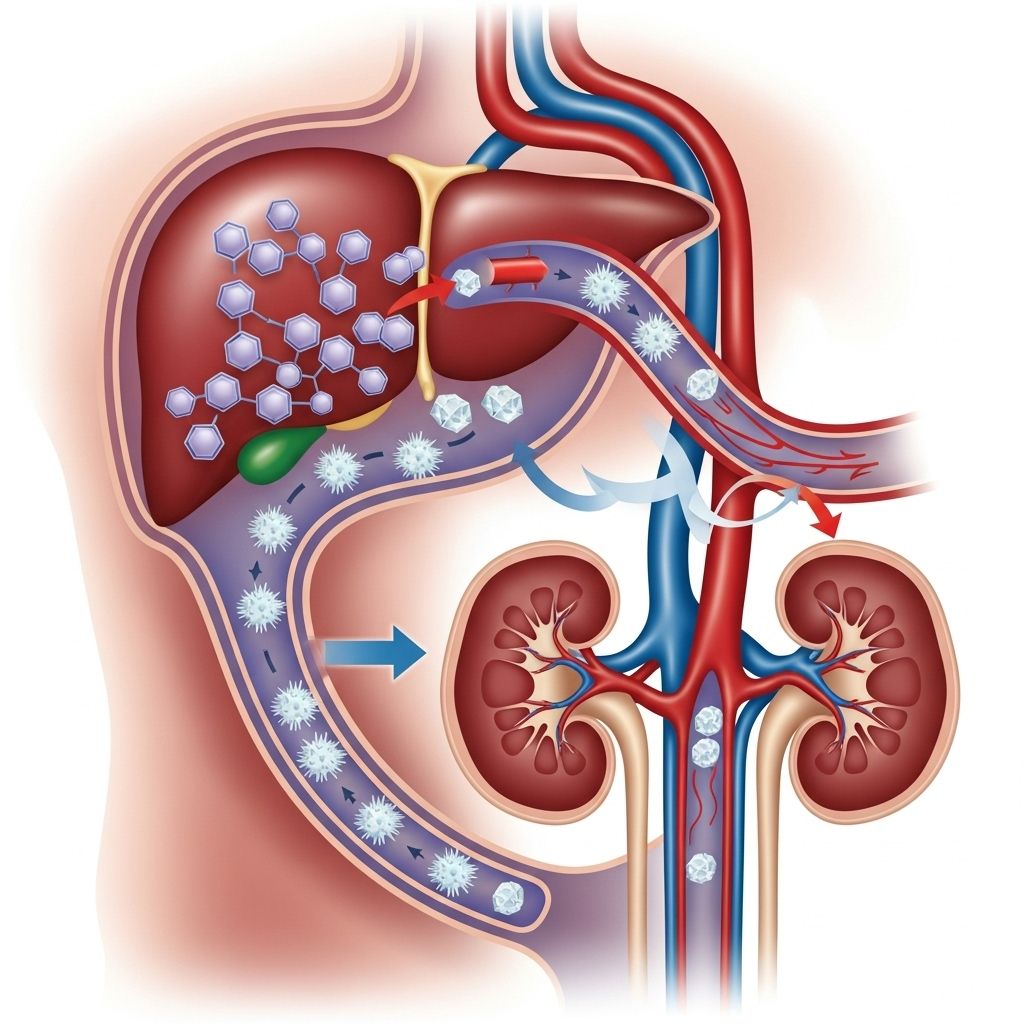
Table of Contents
- Introduction: The Fructose-Uric Acid-Hypertension Pathway
- Fructose Metabolism and Uric Acid Production
- Molecular and Physiological Pathways Linking Fructose, Uric Acid, and Blood Pressure
- Endothelial Dysfunction and the Role of Angiotensin II
- Evidence from Animal Models and Human Studies
- Clinical Implications and Risk Assessment
- Therapeutic Interventions
- Future Perspectives and Research Directions
- Frequently Asked Questions (FAQs)
Introduction: The Fructose-Uric Acid-Hypertension Pathway
High dietary intake of fructose, commonly found in sugar-sweetened beverages and processed foods, has emerged as a crucial contributor to the global epidemics of hypertension and metabolic syndrome. Recent mechanistic studies have elucidated a pathway linking fructose metabolism, increased uric acid production, and subsequent development of hypertension, mediated by endothelial dysfunction and molecular signaling cascades.
Fructose Metabolism and Uric Acid Production
Biochemical Overview
Unlike glucose, fructose is metabolized primarily in the liver via a rapid phosphorylation step mediated by fructokinase, converting fructose into fructose-1-phosphate. This reaction significantly depletes intracellular ATP, generating ADP and subsequently AMP. AMP is then catabolized through the purine degradation pathway, activating AMP deaminase-2 (AMPD2) and triggering the formation of inosine monophosphate (IMP) and, ultimately, uric acid.
- Fructose metabolism bypasses insulin regulation, allowing rapid hepatic uptake and metabolism.
- Uric acid emerges as a byproduct of excessive fructose metabolism.
- This pathway leads to a marked depletion of cellular energy stores, which can activate a survival stress response.
Key Enzymes and Metabolic Steps
| Step | Enzyme | Product |
|---|---|---|
| Fructose → Fructose-1-phosphate | Fructokinase | Fructose-1-phosphate, AMP |
| AMP → IMP | AMP deaminase-2 | IMP |
| IMP → Uric Acid | Purinergic enzymes | Uric Acid |
In essence, high fructose intake not only provides excess calories but also accelerates nucleotide turnover, yielding copious amounts of uric acid.
Molecular and Physiological Pathways Linking Fructose, Uric Acid, and Blood Pressure
Uric Acid as a Pro-Hypertensive Molecule
- Uric acid stimulates local Renin-Angiotensin System (RAS), promoting vascular smooth muscle cell proliferation and stoking endothelial dysfunction.
- Uric acid encourages generation of reactive oxygen species (ROS) via NADPH oxidase activation, setting off oxidative stress within vessel walls.
- Inhibition of AMP-activated protein kinase by uric acid impairs cellular energy balance, promoting lipogenesis, reducing fatty acid oxidation, and lowering ATP production.
Salt Retention and Blood Pressure Elevation
- High-fructose diets up-regulate sodium and chloride transporters, resulting in salt overload and increased blood pressure.
- Chronic fructose consumption leads to increased reabsorption of sodium in the kidneys, further contributing to hypertension.
Interplay with the Sympathetic Nervous System
Fructose-mediated hyperuricemia activates the sympathetic nervous system, exacerbating vasoconstriction and further elevating blood pressure.
Endothelial Dysfunction and the Role of Angiotensin II
Angiotensin II Upregulation and Vasoconstriction
- Fructose feeding increases expression of Angiotensin II (Ang II) and its receptors in vascular tissues.
- Ang II binds AT1 receptors to induce vasoconstriction and activate NADPH oxidase, generating ROS that impairs the vascular endothelium.
- Elevated Ang II levels can be attenuated by ACE inhibitors or AT1 receptor antagonists, normalizing blood pressure in fructose-fed experimental models.
Impaired Nitric Oxide (NO) Bioavailability
- ROS generated by Ang II quickly inactivates nitric oxide, a crucial vasodilator.
- Impairment of endothelial NO synthase (eNOS) activity is observed in fructose-fed models; restoration is possible through blockade of Ang II signaling.
- Overall, the net effect of high fructose and uric acid is diminished vascular relaxation, promoting systemic hypertension.
Endothelin-1 and Additional Vasoconstrictors
- Endothelin-1 (ET-1) is upregulated in fructose consumption scenarios, further aggravating vascular tone.
- ET-1 interacts with Ang II and uric acid-mediated pathways, creating a complex network of endothelial dysfunction triggers.
Evidence from Animal Models and Human Studies
Experimental Animal Models
- Rodents fed high doses of fructose rapidly develop hypertension, elevated uric acid, insulin resistance, dyslipidemia, obesity, and fatty liver.
- Pharmacological reduction of uric acid (e.g., with allopurinol or febuxostat) blocks the formation of hypertension and metabolic syndrome features in these animals.
- Uricosuric agents also attenuate the rise in renal pro-renin receptor expression and salt-sensitive hypertension.
Human Clinical Studies
- Acute intake of fructose (e.g., soft drinks) raises both blood pressure and uric acid levels in humans within minutes.
- Large doses of fructose (200 g/day) over two weeks significantly elevate ambulatory blood pressure; this effect is blocked if uric acid is pharmacologically suppressed.
- High serum uric acid is a reliable predictor of future hypertension in both youth and adult populations, independent of body composition.
- Elevated uric acid blunts blood pressure reduction following lifestyle changes, underscoring its persistent pro-hypertensive effect.
Clinical Implications and Risk Assessment
Key Clinical Insights
- Uric acid assessment may help identify individuals, especially children and adolescents, at high risk for developing hypertension.
- Early detection of hyperuricemia provides a window for preventive intervention in hypertension and vascular disease.
- Persistent hyperuricemia can serve as a biomarker for essential hypertension, potentially guiding future management strategies.
Metabolic Syndrome and Vascular Health
Fructose-induced hypertensive states often co-exist with metabolic syndrome—characterized by obesity, insulin resistance, and fatty liver—worsening cardiovascular risk profiles.
Therapeutic Interventions
Pharmacological Approaches
- Allopurinol and Febuxostat (uric acid-lowering drugs) not only reduce uric acid levels but also block the development of hypertension and metabolic syndrome when administered to at-risk experimental models.
- ACE inhibitors and AT1 receptor antagonists prevent Ang II-mediated endothelial dysfunction and hypertension.
- Uricosurics show benefit in hyperuricemic children as effective antihypertensive strategies.
Lifestyle Interventions
- Dietary reduction of sugar-sweetened beverages and processed foods is recommended to limit fructose intake.
- Lifestyle modification to control body weight and metabolic syndrome features may improve vascular outcomes, but elevated uric acid may blunt blood pressure response.
Future Perspectives and Research Directions
Despite considerable advances, untangling the relative importance of all mechanistic pathways—from uric acid to ET-1 and Ang II—in fructose-induced hypertension remains a challenge. Further validation in diverse human populations, longitudinal studies, and clinical trials examining intervention efficacy will advance our understanding and inform targeted therapies.
- Key research priorities include: dissecting molecular signaling networks, identifying population risk factors, and developing efficient screening tools for hyperuricemia-related hypertension.
- Continued exploration of uric acid as a diagnostic and therapeutic target may lead to significant reduction in cardiovascular morbidity at population scale.
Frequently Asked Questions (FAQs)
Q: What makes fructose different from glucose in raising blood pressure?
Fructose metabolism generates uric acid much more rapidly and in greater amounts than glucose, depleting cellular ATP and activating vascular dysfunction mechanisms. This leads to a more pronounced impact on blood pressure regulation.
Q: Can reducing uric acid directly help lower hypertension?
Studies in both animals and humans show that lowering uric acid with drugs like allopurinol or febuxostat can block or reduce the development of hypertension associated with high fructose intake.
Q: Is hyperuricemia a reliable biomarker for predicting hypertension?
Yes, elevated serum uric acid is correlated with increased risk of future hypertension, especially in young populations. Its assessment may help identify high-risk individuals for early prevention.
Q: Are there other health problems linked to the fructose-uric acid pathway?
Excess fructose intake and hyperuricemia are linked not only to hypertension, but also to obesity, fatty liver, insulin resistance, dyslipidemia, and the broader metabolic syndrome.
Q: How quickly do blood pressure and uric acid levels rise after fructose consumption?
Human studies show increases in blood pressure and uric acid within minutes of acute fructose intake, highlighting the rapid onset of these metabolic effects.
References
Read full bio of Sneha Tete












