Differentiating Fibromyalgia Tender Points and Myofascial Trigger Points: Mechanisms, Diagnosis, and Management
Distinguishing pain types unlocks improved approaches for lasting relief.
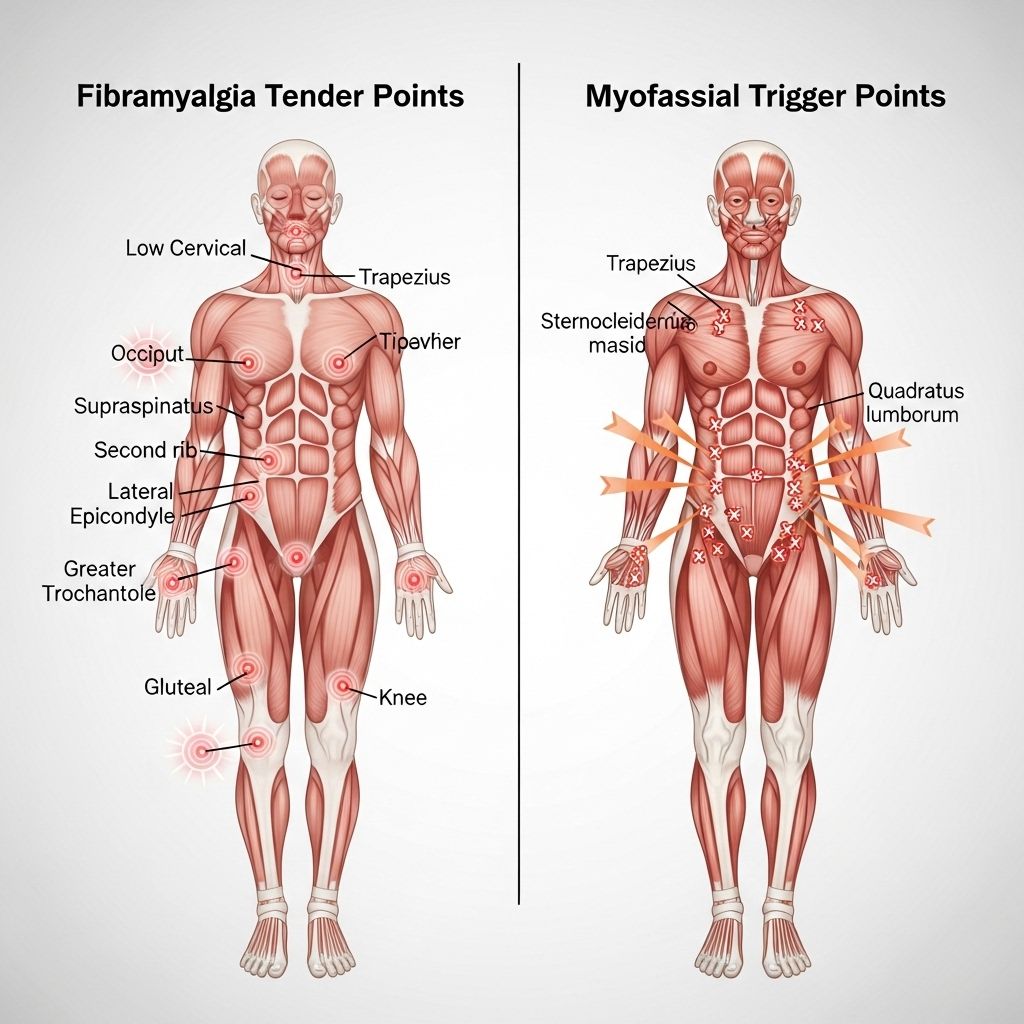
Chronic musculoskeletal pain syndromes are prevalent and challenging conditions in clinical medicine. Among these, fibromyalgia and myofascial pain syndrome are two frequently encountered disorders that are often confused due to overlapping presentations. Central to understanding these conditions is the distinction between fibromyalgia tender points and myofascial trigger points. While both represent focal areas of increased sensitivity, their underlying mechanisms, diagnostic criteria, treatment approaches, and clinical implications differ significantly.
Table of Contents
- Introduction
- Understanding Fibromyalgia Tender Points
- Myofascial Trigger Points Explained
- Comparison: Key Differences
- Diagnosis and Clinical Evaluation
- Overlap and Coexistence
- Mechanisms: Central vs. Peripheral Pain
- Treatment Approaches
- Clinical Implications and Management Strategies
- Frequently Asked Questions (FAQs)
- Conclusion
Introduction
The terms “tender points” and “trigger points” are widely used in the assessment of chronic pain disorders. However, inconsistent usage and misunderstanding can complicate diagnosis and management. Fibromyalgia (FM) is primarily characterized by widespread musculoskeletal pain and specific tender points, while myofascial pain syndrome (MPS) is associated with localized muscle pain and palpable trigger points. Distinguishing between these entities is crucial for delivering appropriate care and optimizing patient outcomes.
Understanding Fibromyalgia Tender Points
Tender points in fibromyalgia are defined as areas of exquisite sensitivity found in specific locations on the body. Their identification formed the basis of the American College of Rheumatology (ACR) 1990 diagnostic criteria for fibromyalgia.
Key Characteristics of Tender Points
- Not palpable—the examiner cannot feel them but can provoke pain by applying moderate pressure.
- Located in predictable, symmetric locations—classically 18 points in the neck, back, chest, elbows, hips, buttocks, and knees.
- Cause local pain—not deep, radiating, or referred pain.
- Very superficial—often right under the skin and not in the joints or deep muscles.
- Induce a characteristic flinch or withdrawal when pressed.
- No objective tissue abnormality is detectable upon examination or imaging.
Mechanism of Tenderness
Tenderness is believed to arise primarily from dysregulation of the central nervous system—referred to as “central sensitization.” This leads to heightened pain perception in response to minimal stimuli at these points.
Diagnostic Considerations
- No structural pathology—tenderness is not related to muscle, joint, or nerve injury.
- Historically, diagnosis required 11 of 18 points to be tender to pressure, but more recent criteria emphasize widespread pain and associated symptoms instead.
- Tender points by themselves do not explain the depth or pattern of pain experienced by fibromyalgia patients.
Myofascial Trigger Points Explained
Trigger points—particularly those seen in myofascial pain syndrome—are distinctly different from fibromyalgia tender points. Their identification and treatment have a unique clinical pathway.
Features of Trigger Points
- Palpable nodules or taut bands—examiners can feel discrete knots within muscle tissue.
- Reproduce characteristic pain patterns when pressed—often radiating pain to predictable locations away from the trigger point (referred pain).
- Associated with muscle weakness, stiffness, diminished range of motion, and sometimes visible twitch responses to palpation.
- Can be visualized by imaging such as ultrasound.
- Considered a peripheral pain generator, often secondary to muscle overuse, trauma, or postural dysfunction.
Types and Stages of Trigger Points
- Active Trigger Points: Cause local and referred pain spontaneously and when compressed.
- Latent Trigger Points: Only cause pain when compressed, do not spontaneously generate pain.
Pathophysiology
Trigger points are caused by the accumulation of dysfunctional muscle fibers due to overload, trauma, or chronic poor posture, leading to local ischemia and release of pain-inducing chemicals.
Comparison: Key Differences
| Feature | Fibromyalgia Tender Points | Myofascial Trigger Points |
|---|---|---|
| Location | Predictable, symmetric points; superficial | Anywhere in muscle; often deep, palpable |
| Pain Type | Local pain only—no referred pain | Radiates pain in consistent specific patterns (referred pain) |
| Palpability | Not palpable; examiner feels nothing unusual | Palpable as taut bands or knots in muscle |
| Clinical Features | No muscle weakness or twitching | Muscle weakness, twitch response, limited mobility possible |
| Associated Mechanism | Central sensitization (CNS dysfunction) | Peripheral muscle pathology (muscle injury or dysfunction) |
| Diagnostic Imaging | Non-detectable by imaging or ultrasound | May be identified on ultrasound |
| Response to Treatment | Not responsive to local injection or manual therapy | Frequently responds to physical therapy, injection, needling |
Diagnosis and Clinical Evaluation
Clinical assessment is the cornerstone of both conditions, though with different approaches.
Fibromyalgia Tender Points
- Diagnosis is largely clinical. Physical exam focuses on tender areas as per ACR criteria, but diagnosis now increasingly relies on widespread pain and accompanying symptoms such as sleep issues, fatigue, and cognitive disturbances.
- No confirmatory imaging or laboratory tests. The presence of at least 11 of 18 tender points was once required, but newer criteria emphasize a broader clinical syndrome.
Myofascial Trigger Points
- Identification is by manual palpation—clinician feels for taut bands, nodules, or knots and assesses for twitch and referred pain.
- Patients usually recognize the pain pattern as familiar.
- Ultrasound or EMG studies occasionally support diagnosis but are not routinely needed.
Overlap and Coexistence
Researchers have established that fibromyalgia and myofascial pain syndrome can coexist within the same patient. In fact, active myofascial trigger points may substantially contribute to the overall pain experience pattern seen in fibromyalgia patients.
- Studies have shown a strong correlation between the number of active myofascial trigger points and fibromyalgia pain severity.
- Each time an active trigger point is pressed in fibromyalgia sufferers, the local and referred pain mapped closely matches their chronic pain pattern.
- Trigger points contain pain-sensitizing chemicals, which may lower pain thresholds and exacerbate central sensitization in fibromyalgia.
Clinical Implications of Overlap
- Careful examination is required to distinguish between fibromyalgia-related tenderness (primarily central) and myofascial trigger point pain (primarily peripheral).
- Individualized treatment strategies are essential, as therapies effective for trigger points may not relieve fibromyalgia pain and vice versa.
- Management of coexisting trigger points can help improve overall function and reduce widespread pain.
Mechanisms: Central vs. Peripheral Pain
The primary difference stems from whether the pain is generated mainly by the central nervous system (CNS) (as in fibromyalgia) or by peripheral musculoskeletal issues (as in myofascial pain syndrome).
Central Sensitization in Fibromyalgia
- Dysregulation leads to amplified pain signals for mild or even non-painful stimuli.
- Neuroendocrine axis dysfunction, altered pain pathways, and abnormal neurotransmitter levels (e.g., serotonin, substance P) play a role.
- Broadly affects pain threshold throughout the body.
Peripheral Pain in Myofascial Trigger Points
- Localized biochemical and mechanical muscle dysfunctions are central.
- Overuse, trauma, and chronic strain generate tight muscle bands and local ischemia, precipitating trigger points.
- Pain is usually limited to distinct regions but can refer in characteristic patterns.
Treatment Approaches
Management approaches significantly differ between fibromyalgia and myofascial pain syndrome due to their distinct pathophysiologies.
Fibromyalgia Treatment Principles
- Multidisciplinary and holistic—incorporating medication, physical activity, psychological support, lifestyle modification, and sometimes physical therapy.
- Pharmacologic agents include low-dose antidepressants, gabapentinoids, SNRIs, and occasional use of cognitive enhancers.
- Non-pharmacological: Cognitive behavioral therapy (CBT), graded aerobic exercise, sleep management, stress reduction.
- Local treatment of tender points (injections, needling, manual therapy) is generally ineffective.
Myofascial Trigger Point Treatment
- Focuses on the direct treatment of trigger points—manual therapies, dry needling, trigger point injections (anesthetic or saline), and stretching.
- Physical therapies like ultrasound, heat, massage, and posture correction can bring relief.
- Specific muscle relaxation and self-management techniques help prevent recurrence.
- Effective local treatment provides dramatic improvement in most cases.
Clinical Implications and Management Strategies
For healthcare professionals, understanding the distinctions ensures appropriate diagnosis and treatment planning:
- Misidentification may result in ineffective or even harmful interventions.
- Both diagnoses can coexist, complicating management and requiring individualized approaches.
- Differential diagnosis is vital: systemic symptoms (fatigue, sleep disturbance, cognitive issues) point to fibromyalgia, while focal muscle pain and dysfunction favor myofascial involvement.
- Patient education is paramount; empowering individuals to participate in self-management improves long-term outlook.
Frequently Asked Questions (FAQs)
What are fibromyalgia tender points, and where are they located?
Fibromyalgia tender points are small, specific areas near joints—such as the neck, shoulders, chest, hips, and knees—that respond with local pain when pressed. These points are more sensitive than surrounding tissues and are not related to underlying joint or muscle injury.
How do myofascial trigger points differ from fibromyalgia tender points?
Myofascial trigger points are palpable knots in muscle that cause pain locally and in referred areas when pressed. They arise from muscle dysfunction and can be treated with local therapies such as needling or massage, unlike fibromyalgia tender points, which are due to central nervous system sensitization and do not improve with local treatments.
Can a person have both fibromyalgia and myofascial trigger points?
Yes, the conditions often overlap. Active trigger points are frequently found in fibromyalgia patients and may amplify overall pain symptoms. Addressing both central and peripheral contributions to pain is important for effective management.
What is the best approach to diagnose these conditions?
Diagnosis is clinical, based on physical examination, detailed history, and pattern of symptoms. Tender points are evaluated by assessing sensitivity, while trigger points are identified by palpating for taut muscle bands and reproducing familiar pain patterns. Laboratory or imaging tests are rarely helpful except to rule out other conditions.
Are tender points still required for fibromyalgia diagnosis?
No, recent criteria emphasize widespread pain and associated symptoms such as sleep disorder, fatigue, and cognitive complaints rather than strictly relying on tender point count.
Conclusion
The clinical distinction between fibromyalgia tender points and myofascial trigger points is essential in chronic pain medicine. Fibromyalgia is primarily a syndrome of central pain sensitization with characteristic, non-palpable tender points and systemic symptoms, whereas myofascial trigger points are palpable, local muscle abnormalities that generate referred pain. Accurate differentiation allows for tailored treatment strategies and improved patient outcomes. As research advances, greater clarity will further improve the understanding and care for patients struggling with chronic musculoskeletal pain syndromes.
References
- https://www.healthcentral.com/article/the-difference-between-fibromyalgia-tender-points-and-myofascial-trigger-points
- https://www.fibromyalgiafund.org/tender-points-are-mostly-mtps/
- https://pubmed.ncbi.nlm.nih.gov/7595112/
- https://www.webmd.com/fibromyalgia/fibromyalgia-tender-points-trigger-points
- https://chiroup.com/blog/10-key-differences-between-trigger-points-fibromyalgia
- https://www.youtube.com/watch?v=UyEJyEplYYs
- https://www.droracle.ai/articles/197290/define-trigger-points-vs-tender-points
- https://woodlandspaindr.com/understanding-fibromyalgia-pressure-points-causes-and-treatments/
- https://www.medicalnewstoday.com/articles/myofascial-pain-syndrome-vs-fibromyalgia
Read full bio of Sneha Tete












