Environmental Pollutants and Vascular Health: How Exposure Threatens Cardiovascular Well-Being
Cleaning up air, water, and soil contamination protects hearts at every stage of life.
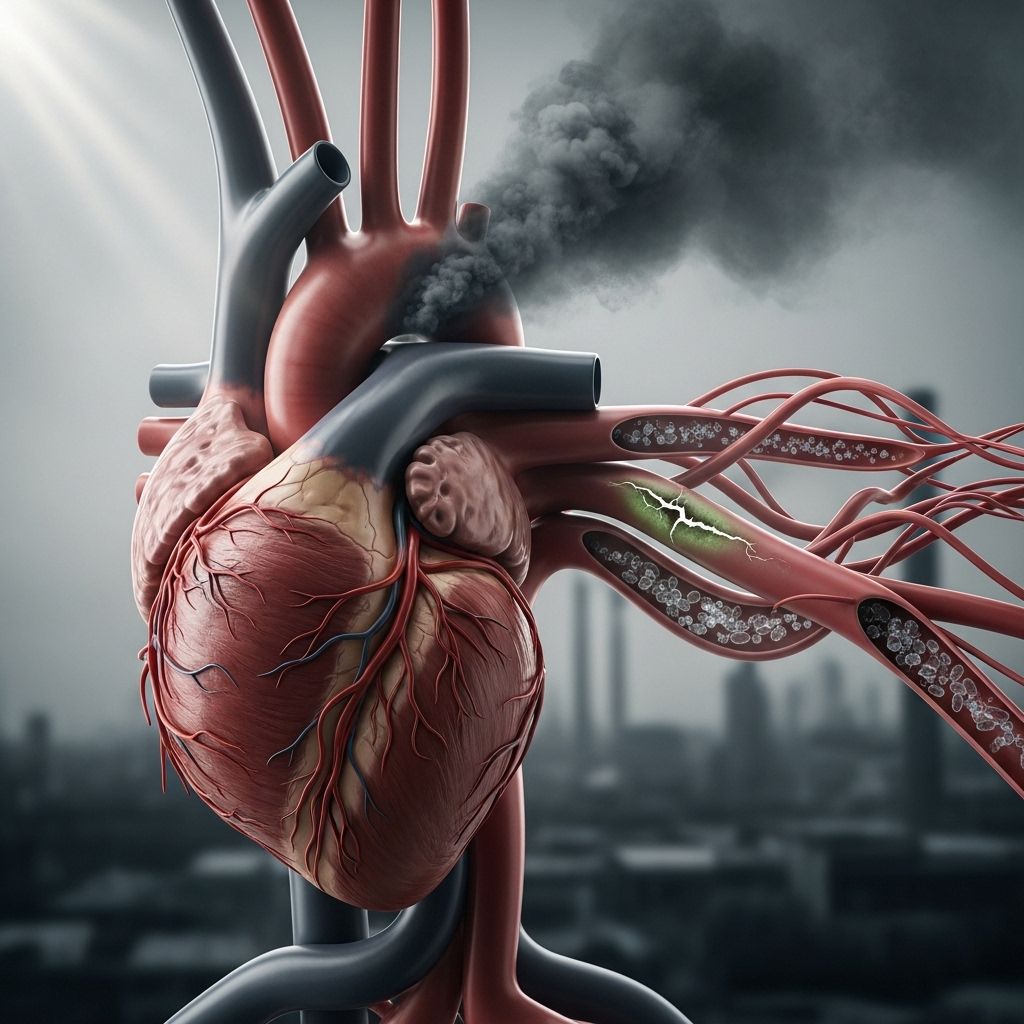
Cardiovascular disease (CVD) remains the leading cause of mortality globally, with mounting evidence implicating environmental pollutants as critical contributors to the burden of vascular health complications. This comprehensive article explores the mechanisms by which various environmental pollutants impact the vascular system, the breadth of associated risks, and contemporary approaches to mitigation and intervention. The interplay between pollutants and vascular health highlights urgent needs for regulatory policies and community-level interventions.
Table of Contents
- Understanding Vascular Health
- Environmental Pollutants: An Overview
- Major Environmental Pollutants and Their Vascular Effects
- Mechanisms of Vascular Injury
- Populations at Increased Risk
- Epidemiological Evidence
- Prevention and Public Health Strategies
- Frequently Asked Questions (FAQs)
Understanding Vascular Health
The vascular system, comprising arteries, veins, and capillaries, is responsible for delivering blood, oxygen, and nutrients throughout the body. Healthy blood vessels adapt to changes in blood pressure, regulate inflammation, and prevent clot formation. Disruption of vascular health can cause a range of conditions—hypertension, atherosclerosis (hardening and narrowing of arteries), heart attacks, strokes, and peripheral artery disease.
- Endothelial function refers to the capacity of the inner lining of blood vessels to maintain vascular tone and homeostasis.
- Vascular dysfunction is a precursor for many cardiovascular diseases and is aggravated by both genetic and environmental factors.
Environmental Pollutants: An Overview
Environmental pollutants are substances introduced into the ecosystem by human activity, industrial processes, and urbanization. Over time, chronic exposure—even at low concentrations—has pronounced negative effects on human health, particularly on the cardiovascular system. These pollutants include not just traditional air pollutants but also emerging contaminants such as microplastics and persistent organic chemicals.
- Air pollutants: Particulate matter (PM2.5 and PM10), nitrogen dioxide (NO2), ozone (O3), sulfur dioxide (SO2), and carbon monoxide (CO).
- Heavy metals: Lead, mercury, cadmium, and arsenic infiltrate the environment via industrial activities, water contamination, and food chain accumulation.
- Persistent chemicals: Perfluoroalkyl substances (PFAS), pesticides, and plasticizers disrupt endocrine and immune systems.
- Microplastics and nanoparticles: Tiny plastic debris and ultrafine particles are increasingly found in the air, water, and food supply.
Major Environmental Pollutants and Their Vascular Effects
Multiple classes of environmental pollutants contribute to vascular disease through distinct and overlapping mechanisms. This section highlights the major environmental threats and summarizes current scientific understanding of their impact on vascular health.
| Pollutant | Main Sources | Key Vascular Effects |
|---|---|---|
| PM2.5 (Fine Particulate Matter) | Combustion engines, industry, biomass burning |
|
| Nitrogen Dioxide (NO2) | Vehicle exhaust, power plants |
|
| Sulfur Dioxide (SO2) | Fossil fuel combustion, industrial processes |
Environmental pollutants pose significant risks not only to cardiovascular health but also to skin barrier integrity. To fully understand these implications, check out our in-depth exploration of how environmental pollutants impact skin barrier health for essential strategies to protect your skin's defense. |
| Ozone (O3) | Atmospheric photochemical reactions, urban smog |
|
| Heavy Metals (Lead, Cadmium) | Industrial pollution, old pipes, contaminated water |
|
| Pesticides & Microplastics | Agricultural runoff, plastics breakdown |
|
Air Pollutants
PM2.5, or fine particulate matter with a diameter less than 2.5 microns, is especially dangerous due to its ability to penetrate deep into lung tissue and enter the bloodstream, initiating acute vascular events and chronic cardiovascular disease.
Nitrogen dioxide (NO2) is a major contributor to traffic-related air pollution and is associated with vascular remodeling and heightened risk of acute cardiac incidents.
Ozone (O3) and carbon monoxide (CO) exposure cause oxidative stress and dysfunction in blood vessels, further aggravating the risk of heart attacks and strokes.
Heavy Metals
Metals such as lead and cadmium have long been recognized for their cardiovascular toxicity. Chronic exposure impairs endothelial function, promotes inflammation, and is associated with increased arterial stiffness, hypertension, and atherogenesis.
Pesticides and Microplastics
Pesticides and microplastics represent emerging threats. Both are linked to chronic endothelial inflammation, metabolic disruptions, and the risk of vascular tissue damage. The mechanisms are under active investigation but include induction of oxidative stress and direct cellular toxicity.
Mechanisms of Vascular Injury
Environmental pollutants can disrupt vascular health through several interconnected biological pathways:
- Inflammation: Environmental toxins stimulate the release of pro-inflammatory cytokines, accelerating plaque formation and arterial blockage.
- Oxidative stress: Many pollutants induce the generation of reactive oxygen species (ROS) that damage cell membranes, proteins, and DNA in vascular tissues.
- Endothelial dysfunction: Damage to the endothelial cells lining blood vessels impairs vasodilation, promotes clotting, and increases permeability.
- Autonomic imbalance: Pollutants can alter nervous system regulation of vascular tone, raising blood pressure and increasing arrhythmia risk.
- Accelerated atherosclerosis: Chronic exposure speeds the development and instability of atherosclerotic plaques.
These mechanisms often occur simultaneously, increasing the likelihood of triggering acute cardiovascular events in susceptible individuals.
Populations at Increased Risk
Not all populations face equal risk. Certain groups are more vulnerable to the effects of environmental pollutants on vascular health due to physiological, genetic, or socioeconomic factors.
- Older adults: Aging-related vascular changes magnify pollutant impact.
- People with preexisting cardiovascular disease: History of heart attack, stroke, or congestive heart failure increases sensitivity to pollutant exposure.
- Individuals with diabetes or high cholesterol: These metabolic conditions exacerbate pollutant-induced inflammation.
- Low socioeconomic status communities: Greater likelihood of living near pollution sources with less access to health care or mitigation resources.
- Non-white populations: Racial minorities are often overrepresented in high-exposure areas due to environmental injustice.
Epidemiological Evidence
Decades of research firmly connect environmental pollution to increased rates of vascular disease. Key observational and experimental findings include:
- Short- and long-term exposure to PM2.5 is linked to higher rates of heart attacks, stroke, arrhythmias, heart failure, and sudden cardiac death.
- Longitudinal cohort studies demonstrate that every 10 μg/m3 increase in annual PM2.5 is associated with a measurable rise in cardiovascular events and mortality.
- Hospitalizations for acute heart problems spike during air pollution episodes, especially among those with already compromised heart or blood vessel health.
- Emerging data implicate microplastics and chemical contaminants in early atherosclerosis in animal models, with suggestive evidence building in humans.
Signs and Symptoms of Exposure-Linked Vascular Dysfunction
- Heart palpitations
- Unusual fatigue
- Lightheadedness
- Shortness of breath
- Chest tightness or pain in the chest, neck, or shoulder
Prevention and Public Health Strategies
Addressing the vascular risks of environmental pollutants requires action on multiple fronts:
Policy and Regulation
- Enforcing air quality standards (such as PM2.5 limits) at local, national, and global levels.
- Banning or regulating known toxic substances (e.g., lead, certain pesticides).
- Promoting green urban planning, with more green spaces, less reliance on fossil fuels, and improved public transportation.
Community and Individual Actions
- Monitoring local air quality reports and minimizing outdoor activities during high-pollution periods.
- Using air filtration systems indoors.
- Adopting cleaner energy and transportation technologies.
- Supporting policies that address social determinants of health, especially in vulnerable communities.
Healthcare Interventions
- Identifying high-risk individuals based on their clinical history and exposure profiles.
- Counseling patients to reduce modifiable risk factors (smoking, cholesterol, hypertension).
- Early screening and preventive management of cardiovascular risk in susceptible populations.
Frequently Asked Questions (FAQs)
Q: What are the most dangerous environmental pollutants for vascular health?
A: The most dangerous are fine particulate matter (PM2.5), nitrogen dioxide, sulfur dioxide, ozone, heavy metals like lead, and persistent organic pollutants such as pesticides and PFAS.
Q: How quickly can air pollution affect the cardiovascular system?
A: Health consequences can occur after short-term exposures (hours to days), triggering acute cardiovascular events in people with existing heart disease, but the cumulative effects of long-term exposure cause lasting vascular damage.
Q: Who is most at risk from pollutant-induced vascular disease?
A: Older adults, individuals with preexisting heart or vascular diseases, people with metabolic syndromes, socioeconomically disadvantaged communities, and racial minorities.
Q: What can individuals do to protect their vascular health from pollution?
A: Limit exposure during high-pollution days, use indoor air filtration, maintain overall heart health, and support policies for cleaner air and reduced toxin emissions.
Q: Are emerging pollutants like microplastics a real threat to human vascular health?
A: Evidence is growing that microplastics and nanoplastics can induce inflammation and tissue injury in blood vessels, but more research is needed for definitive conclusions.
Q: How do socioeconomic factors influence pollutant-related cardiovascular risk?
A: Lower socioeconomic status is linked to higher pollutant exposure, limited access to healthcare, and greater cumulative cardiovascular risk.
References: This article draws upon leading scientific reviews and data from public health agencies on environmental pollutant exposure and vascular health, including research published in peer-reviewed journals and official governmental advisories.
References
Read full bio of medha deb












