Understanding Digestion Issues After Gallbladder Removal: Symptoms, Causes, and Solutions
Practical strategies help you adjust your meals and routines for lasting comfort.
Understanding Digestion Issues After Gallbladder Removal
Gallbladder removal, or cholecystectomy, is a common surgical procedure primarily performed to treat gallstones and related complications. While the surgery often provides welcome relief, many people experience significant changes in their digestive system post-operation. This article explores the causes, symptoms, and management of digestive issues that frequently arise following gallbladder removal, providing detailed strategies for adapting and thriving after this major digestive shift.
Table of Contents
- The Role of the Gallbladder in Digestion
- How Digestion Changes After Gallbladder Removal
- Common Digestive Symptoms After Surgery
- Underlying Causes of Post-Surgical Digestive Issues
- Managing Digestive Issues Post-Gallbladder Removal
- Recommended Diet and Lifestyle Modifications
- Potential Complications and Long-Term Concerns
- Frequently Asked Questions (FAQs)
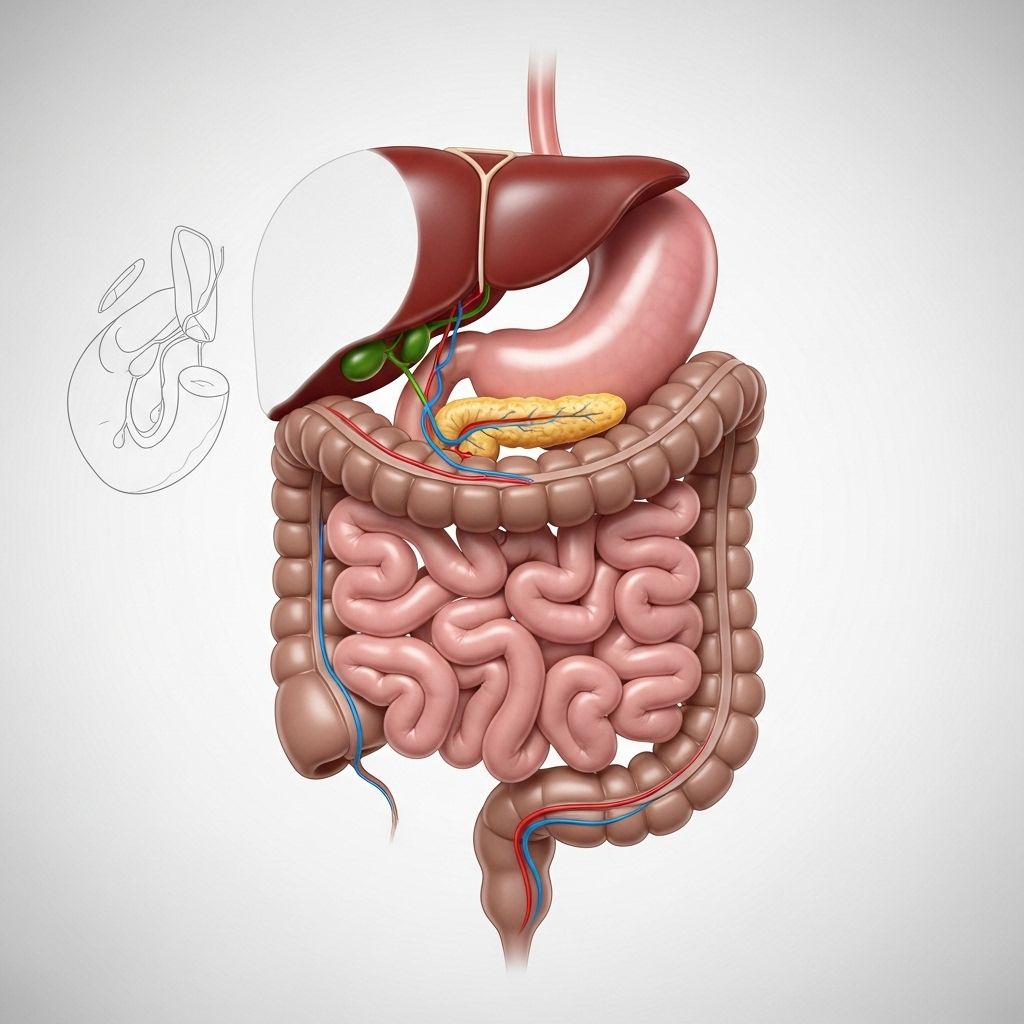
The Role of the Gallbladder in Digestion
The gallbladder is a small pear-shaped organ situated beneath the liver. Its primary purpose is to store and concentrate bile, a digestive fluid produced by the liver. Bile is released into the small intestine in response to dietary fat, where it assists in emulsifying fats, making them easier for the body to absorb and process.
- Storage: Bile produced by the liver is temporarily held and becomes concentrated in the gallbladder.
- Fat Digestion: During a meal, especially one rich in fat, the gallbladder contracts and releases bile into the small intestine to aid in breaking down fat molecules.
Without the gallbladder, this tightly regulated process is disrupted, leading to continuous bile flow into the intestine rather than the timely, concentrated release that occurs during digestion of fatty foods.
How Digestion Changes After Gallbladder Removal
Post-cholecystectomy, the body must adapt to the direct flow of bile from the liver into the small intestine. This seemingly minor anatomical change has meaningful physiological effects:
- Continuous Bile Flow: Bile enters the digestive tract steadily but less concentrated, making fat digestion less efficient—especially after high-fat meals.
- Incomplete Fat Digestion: The weaker, continuous bile flow may not match the fat load of meals, leaving excess fat undigested and resulting in digestive discomfort such as diarrhea or greasy stools.
- Adjustment Period: Most people notice symptoms within a few weeks after surgery, but for many, the digestive system gradually adapts, and symptoms lessen over time.
Common Digestive Symptoms After Surgery
Many people adjust smoothly following gallbladder removal, but a significant proportion experience ongoing or new digestive symptoms. The most frequent complaints include:
- Bloating and Gas: Irregular release and less potent bile can increase gas production and bloating, notably after eating fatty foods.
- Diarrhea: Excess bile has a laxative effect, often leading to loose stools or frequent trips to the bathroom—especially soon after eating. Around 20% of patients experience chronic diarrhea, but it usually resolves within a few months.
- Steatorrhea: Fatty, greasy stools indicate undigested fats in bowels, a relatively common occurrence when bile is insufficient to process dietary fat.
- Abdominal Pain: Mild or intermittent discomfort may occur as the intestines adapt to the new digestive environment, sometimes resembling the pain previously caused by gallstones.
These symptoms are commonly categorized under post-cholecystectomy syndrome (PCS), an umbrella term for persistent or recurrent digestive distress following removal of the gallbladder.
Underlying Causes of Post-Surgical Digestive Issues
Understanding the mechanisms driving these symptoms is essential for effective management. The primary causes include:
- Bile Acid Malabsorption (BAM): Also known as bile acid diarrhea, BAM occurs when bile salts reach the colon in larger quantities than the intestine can absorb, resulting in watery diarrhea.
- Sphincter of Oddi Dysfunction: The sphincter of Oddi, a muscular valve controlling bile and pancreatic juice flow, can malfunction after surgery. Dysfunction may lead to abdominal pain, diarrhea, nausea, and vomiting.
- Retention of Gallstones: Occasionally, stones remain in the bile ducts after surgery, triggering pain, jaundice, fever, and digestive distress that may require further medical intervention.
- Bile Reflux: Without the regulatory control of the gallbladder, bile may flow backward into the stomach, causing gastritis, heartburn, and even inflammation.
| Cause | Symptoms | Management |
|---|---|---|
| Bile Acid Malabsorption | Loose stools, urgent diarrhea | Bile acid sequestrants, dietary adjustments |
| Sphincter of Oddi Dysfunction | Abdominal pain, nausea | Medication, endoscopic procedures |
| Bile Reflux | Heartburn, gastritis | Medications, lifestyle changes |
| Retained Gallstones | Pain, jaundice, fever | Further surgery or endoscopy |
Managing Digestive Issues Post-Gallbladder Removal
Although these symptoms can be bothersome, effective strategies exist to help patients regain digestive comfort:
- Bile Acid Sequestrants: Medications like cholestyramine bind to bile acids in the intestine, reducing diarrhea due to bile acid malabsorption.
- Gradual Diet Progression: Start with a bland, low-fat diet after surgery and slowly reintroduce other foods to identify tolerance levels.
- Portion Control: Eat smaller, more frequent meals to avoid overwhelming the digestive tract with large quantities of fat at once.
- Medical Follow-up: Persistent or severe symptoms warrant consultation. Additional interventions, such as imaging, bile acid studies, or endoscopy, may be necessary to rule out retained stones or sphincter dysfunction.
- Supplements: Occasionally, fat-soluble vitamins (A, D, E, K) supplementation is recommended if malabsorption becomes significant.
Recommended Diet and Lifestyle Modifications
Dietary Strategies
- Limit Fats: Restrict high-fat foods, fried items, and rich desserts—opt for lean proteins and low-fat cooking methods.
- Increase Fiber: Gradually add soluble fiber (oats, bananas, carrots) to help regulate stool consistency and slow bile-induced transit.
- Monitor Dairy Intake: Some people become temporarily lactose intolerant after surgery—reduce dairy if it worsens symptoms.
- Stay Hydrated: Drink plenty of water, especially if experiencing diarrhea, to prevent dehydration.
- Mind Food Triggers: Keep a food diary to track which foods aggravate symptoms and consider eliminating or substituting these triggers.
Lifestyle Adjustments
- Avoid Alcohol and Tobacco: Both can increase gastrointestinal irritation, promote reflux, and worsen digestive symptoms.
- Regular Physical Activity: Light exercise helps maintain gut motility and overall digestive health.
- Stress Management: Practice mindfulness, yoga, or relaxation exercises to minimize stress-related gastrointestinal discomfort.
Potential Complications and Long-Term Concerns
Beyond immediate digestive symptoms, gallbladder removal can increase risk for certain uncommon but serious complications over time:
- Bile Duct Stones: Without a gallbladder, new stones may form in the bile ducts, occasionally causing pain or jaundice and requiring medical intervention.
- Bile Reflux Gastritis: Chronic bile reflux can inflame the lining of the stomach and esophagus if unmanaged.
- Colon Cancer: Some data suggest a slightly elevated risk of colon cancer after cholecystectomy, though this remains an area of ongoing research. Regular check-ups and colonoscopies may be recommended for individuals with risk factors.
It is crucial to maintain regular follow-ups with your healthcare provider to monitor these risks and intervene early if complications arise.
Frequently Asked Questions (FAQs)
Q: How long do digestive symptoms last after gallbladder removal?
Most people experience symptoms for a few weeks to a few months as the digestive tract adapts. For many, symptoms gradually resolve, but up to 20% of patients may have persistent diarrhea or other issues lasting longer than three months. Work with your healthcare provider for tailored management if symptoms persist.
Q: Are there foods I should permanently avoid after surgery?
High-fat, greasy, and fried foods are most likely to cause ongoing symptoms. While many people can gradually tolerate more varied diets as time goes on, it is generally wise to limit these foods indefinitely if they continue causing problems. Spicy, highly processed foods, and large amounts of dairy can also be problematic for some individuals.
Q: When should I seek medical attention?
Contact your doctor if you experience severe or worsening abdominal pain, ongoing diarrhea for more than three months, significant weight loss, jaundice (yellowing of the skin or eyes), fever, or persistent vomiting. These symptoms may signal retained stones, bile duct injury, or an unrelated digestive disorder requiring further evaluation.
Q: Can supplements help with digestion after gallbladder removal?
Yes. In cases of significant fat malabsorption, your physician may recommend supplements, including digestive enzymes or fat-soluble vitamins. Probiotics and soluble fiber supplements may also alleviate symptoms in some people, but always discuss with a healthcare professional before starting new supplements.
Q: Is long-term medication required?
Most people do not require ongoing medication, but those with severe bile acid diarrhea may need long-term bile acid sequestrants. If you develop bile reflux or gastritis, acid-suppressing medication or other drugs may be prescribed.
Key Takeaways
- Gallbladder removal commonly leads to changes in bile flow, affecting fat digestion and sometimes causing diarrhea, bloating, and abdominal discomfort.
- Most people adapt within months, but a subset experience ongoing symptoms necessitating dietary changes, medications, or supplements.
- Monitor for warning signs of complications such as severe pain or jaundice and seek medical advice promptly when needed.
- Working closely with your healthcare team is the best way to optimize digestive health and live well after gallbladder removal.
References
- https://www.missionsurgical.com/blogs/the-surprising-impact-of-gallbladder-surgery-on-digestion-and-long-term-health/
- https://www.healthline.com/health/ibs-after-gallbladder-removal
- https://texasherniaspecialists.com/navigating-digestive-changes-after-gallbladder-removal/
- https://my.clevelandclinic.org/health/procedures/21614-gallbladder-removal
- https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=134&ContentID=181
- https://www.mayoclinic.org/tests-procedures/cholecystectomy/expert-answers/gallbladder-removal/faq-20058481
- https://www.vinmec.com/eng/blog/complications-of-abdominal-pain-after-cholecystectomy-en
- https://allieddigestivehealth.com/digestive-problems-after-gallbladder-surgery/
Read full bio of medha deb












