Demodex Mites in Refractory Rosacea & Blepharitis: Pathogenesis, Diagnosis, and Management
Addressing underlying triggers and inflammation leads to more effective symptom control.
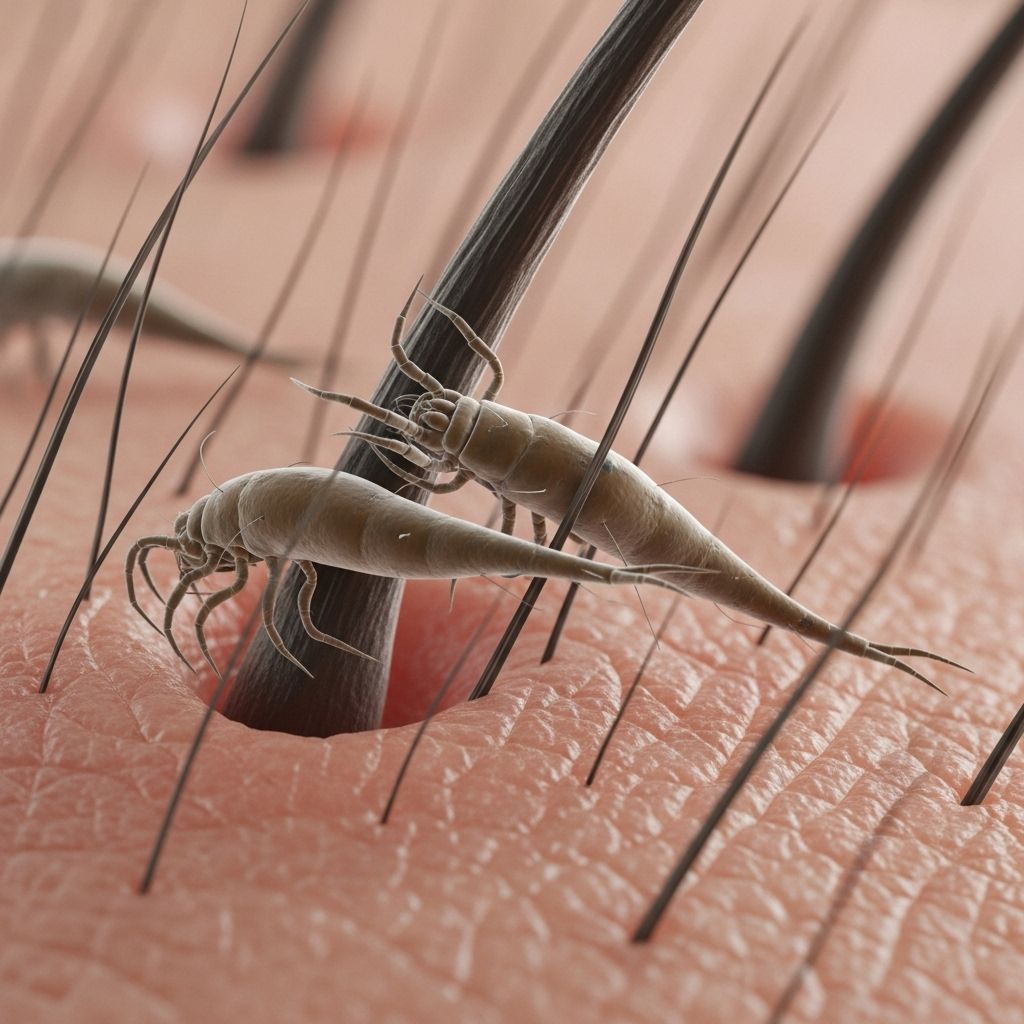
Demodex mites have long intrigued dermatologists and ophthalmologists due to their controversial but increasingly recognized role in refractory forms of skin and eyelid inflammation, particularly rosacea and blepharitis. This article thoroughly examines their biology, pathophysiological significance, clinical relevance in persistent disease, diagnostic approaches, and modern treatment strategies, aiming to deliver a state-of-the-art resource for clinicians and patients alike.
Table of Contents
- Introduction
- Biology of Demodex Mites
- Demodex and Refractory Rosacea
- Demodex and Blepharitis
- Diagnosis of Demodex-Associated Disease
- Treatment Strategies and Management
- Challenges: Refractoriness and Relapse
- Emerging Therapies & Research Directions
- Frequently Asked Questions
- Conclusion
Introduction
Rosacea and blepharitis are chronic, relapsing inflammatory diseases affecting the skin and ocular surfaces, respectively. A subset of patients remains refractory to standard therapy, often experiencing flares and ongoing discomfort. Mounting evidence implicates Demodex mites as a key trigger or amplifier in these stubborn cases, both through direct micro-inflammation and as carriers of pro-inflammatory bacteria.
Biology of Demodex Mites
The human skin is the natural host to two principal species of Demodex:
- Demodex folliculorum – primarily found in hair follicles, especially on the face and eyelids
- Demodex brevis – inhabits sebaceous and meibomian glands
These microscopic arachnids feed on sebum, cellular debris, and bacteria. While present in healthy adults, over-proliferation is linked to pathological changes and inflammation, particularly in immune-privileged or dysregulated hosts.
Demodex Lifecycle Characteristics
- Life cycle length: about 14–21 days
- Nocturnal migration to skin surface for mating
- Copious reproduction in sebum-rich environments
Population density is normally low, but factors like increased sebum, immune dysregulation, or chronic inflammation can prompt uncontrolled proliferation, driving clinical disease.
Demodex and Refractory Rosacea
Rosacea is a multifactorial chronic skin disorder characterized by facial redness, papules, pustules, and telangiectasias, primarily on the central face. In refractory cases, standard therapies yield limited or no benefit, and Demodex infestation is frequently observed at higher densities than in both healthy controls and responsive cases.
Pathogenetic Role
- Mite density correlates with disease severity, particularly papulopustular rosacea (PPR).
- Demodex acts as both a direct irritant and an immune trigger via its surface and gut bacteria, amplifying Th1/Th17 immune pathways.
- Proliferation forms a vicious cycle: inflammation promotes mite growth, which then worsens the inflammatory response.
Clinical Evidence
- Studies show significant improvement of rosacea symptoms following acaricidal (mite-killing) treatment.
- Topical ivermectin has proven more effective than metronidazole or other anti-inflammatories, reflecting the pivotal role of mites in refractory disease.
- Erythema and telangiectasias are less responsive, as these elements are less directly related to Demodex.
Demodex and Blepharitis
Blepharitis is a prevalent, sometimes chronic, inflammatory disorder of the eyelid margin, characterized by:
- Redness and swelling of lid margins
- Ocular discomfort and foreign body sensation
- Cylindrical dandruff (collarettes) at the base of eyelashes
Demodex mites are strongly implicated in refractory or recurrent blepharitis. Their mechanical irritation, in addition to their potential to harbor pro-inflammatory bacteria, worsens chronicity and symptom severity, especially in elderly and immunocompromised patients.
Key Clinical Signs Linked to Demodex in Blepharitis
- Dense cylindrical dandruff at lash roots
- Recurrent chalazia or hordeola
- Resistance to standard lid hygiene and antibiotic therapy
Diagnosis of Demodex-Associated Disease
Definitive diagnosis requires parasitological confirmation, combined with clinical context. Key methods include:
- Standardized skin surface biopsy (SSSB) – estimates mite density per cm2
- Eyelash epilation and microscopic examination – enables detection in refractory blepharitis
- Direct visualization via dermoscopy (reveals follicular plugs/cylindrical dandruff)
More than 5 mites per cm2 or consistent detection in multiple lash specimens strongly supports a diagnosis of clinically significant Demodex infestation.
Treatment Strategies and Management
Multiple treatment classes are available, each with varying efficacy depending on the predominance of mites versus inflammation as primary drivers of disease.
First-Line Therapies
| Agent | Mechanism | Indication | Notes |
|---|---|---|---|
| Ivermectin 1% cream | Acaricidal + anti-inflammatory | Moderate/severe papulopustular rosacea | More effective than metronidazole for Demodex-driven cases |
| Permethrin (1–5%) | Acaricidal | Topical demodicosis, sometimes used for eyelids (off-label) | Can cause local irritation at higher concentrations |
| Metronidazole | Anti-inflammatory/possible indirect anti-mite | Mild cases; adjunctive to acaricides | Less effective at reducing mite density |
| Benzyl benzoate (10–25%) | Strong acaricidal | Refractory demodicosis | No anti-inflammatory effect, causes irritation |
Systemic Therapy
- Oral ivermectin (single or repeated dose): For extensive or refractory cases.
- Low-dose isotretinoin: Reduces sebum, inhibits sebaceous gland function, indirectly limits mite habitat; usually adjunctive.
- Oral tetracyclines (e.g., doxycycline): Target inflammation, may modestly reduce mite density.
Ophthalmic Blepharitis-Specific Treatments
- Lid scrubs with tea tree oil (TTO): TTO (≥50%) kills mites, but lower concentrations (5–10%) are better tolerated on lids.
- Mechanical removal via microblepharoexfoliation
- Adjunctive lubricants and anti-inflammatory drops for ocular surface healing
Combination and Sequential Therapy
Combination regimens, such as permethrin cream plus isotretinoin, or ivermectin with topical metronidazole, address both the mite population and the associated inflammatory cascades in refractory disease. Combination may reduce relapse rates and improve outcomes when conventional monotherapy fails.
Challenges: Refractoriness and Relapse
Even after aggressive elimination of Demodex, recurrence is common due to persistent risk factors, incomplete eradication, or ongoing immune dysregulation. Key challenges include:
- Mite recolonization if contributing factors (e.g., oily skin, immunosuppression) are not addressed
- Partial symptom control—erythema and telangiectasia less amenable to mite-centric therapy
- Treatment intolerance (allergic reaction to acne agents or ocular surface irritation)
- Chronicity of eyelid involvement, particularly with longstanding blepharitis
Emerging Therapies & Research Directions
Ongoing research is exploring additional strategies to break the inflammatory-mite cycle:
- Novel acaricidal agents with improved tolerability for sensitive skin and ocular use
- Targeted immunomodulation (e.g., Th1/Th17 inhibitors) to prevent the inflammatory niche that promotes mite survival
- Bacterial therapy targeting Demodex-associated endotoxin-producing bacteria
- Personalized therapies based on genetic, microbiome, and immune profiling
Frequently Asked Questions (FAQs)
Q: How do I know if Demodex is causing my refractory rosacea or blepharitis?
A: If your symptoms persist despite standard treatment and are accompanied by new or worsening papules, pustules, or characteristic cylindrical dandruff at the eyelid roots, your physician may perform mite detection tests to confirm Demodex involvement.
Q: Are Demodex mites contagious?
A: Demodex mites can transfer between individuals via direct close contact, but clinical disease only develops in predisposed individuals with additional risk factors (seborrhea, immune disorders, chronic inflammation).
Q: Can eliminating Demodex cure rosacea or blepharitis?
A: Elimination of Demodex can lead to marked symptom improvement in refractory cases, particularly for inflammatory lesions. However, some features (such as redness and broken blood vessels) may persist, and relapse is possible if underlying factors are not controlled.
Q: What is the best treatment approach if first-line therapies fail?
A: Combination therapy—targeting both mites (e.g., ivermectin or permethrin) and inflammation (e.g., topical/oral anti-inflammatories, isotretinoin)—often yields superior results in refractory cases.
Q: How can I prevent Demodex-related relapse?
A: Regular skin and lid hygiene, maintenance treatments, and ongoing control of triggers (oil production, environmental or immune factors) can reduce recurrence risk.
Conclusion
Demodex mites are established contributors to refractory rosacea and blepharitis. Diagnostic vigilance and mite-targeted therapies, often in combination with anti-inflammatory agents, offer substantial improvements for patients with persistent disease. Continued innovation is needed to refine treatments and reduce relapses for these chronic, impactful conditions.
References
- https://karger.com/drm/article/240/1/95/866652/Evidence-for-the-Clinical-Association-between
- https://ahdbonline.com/payer-perspectives-in-dermatology/ivermectin-cream-will-contribute-much-to-the-treatment-of-patients-with-rosacea-interview-with-dr-zoe-draelos
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9350859/
- https://my.clevelandclinic.org/health/diseases/22775-demodex-face-mites
- https://www.rosacea.org/patients/the-ecology-of-your-face-demodex-rosacea-and-you
- https://www.eyeworld.org/2008/demodex-treatment-options/
Read full bio of medha deb












