Dangers of Using Expired OTC Medications: Risks, Myths, and Safe Practices
Learn practical tips to keep your medicine cabinet effective and hazard-free.
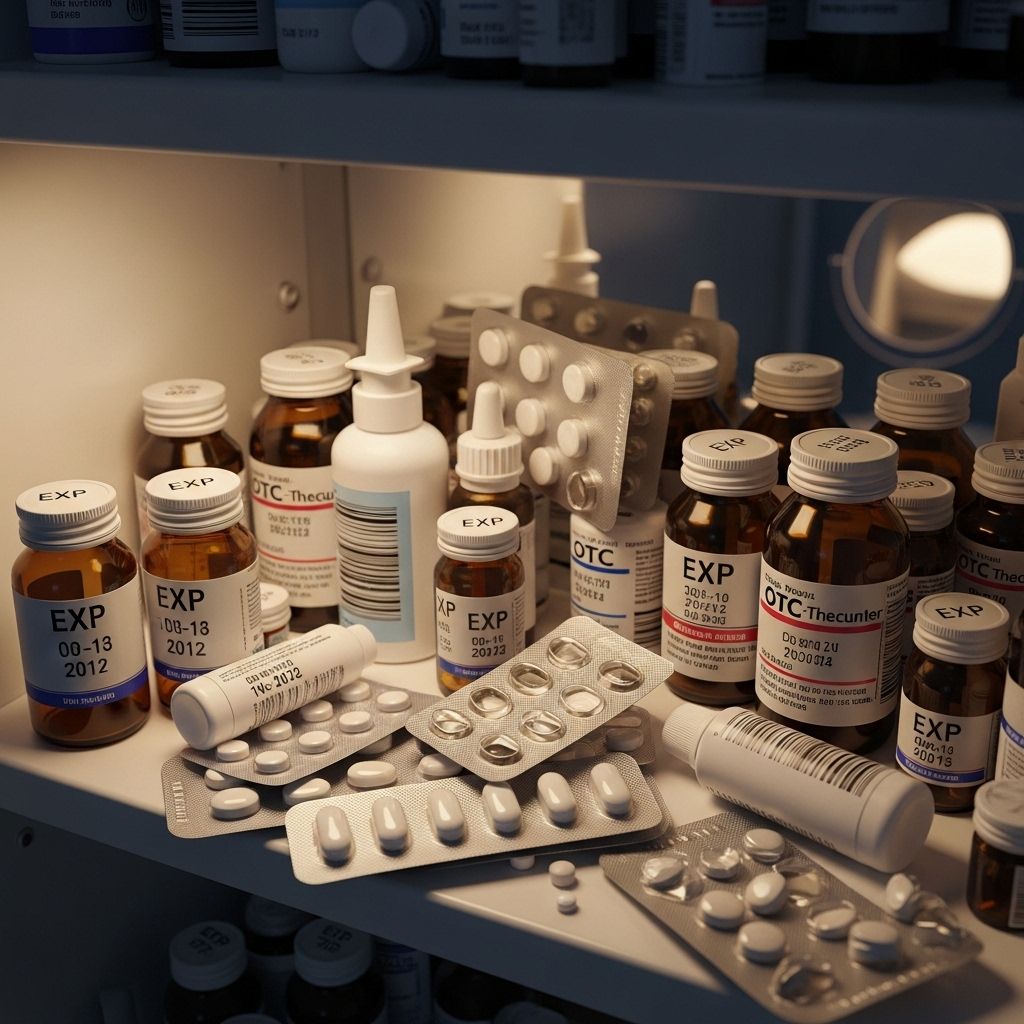
Millions of people rely on over-the-counter (OTC) medications for relief from headaches, colds, allergies, and pain every year. While grabbing a medication from your cabinet, you might notice it expired months or even years ago. Should you still take it? Do expired medications simply lose effectiveness, or do they pose genuine health risks? This article explores what happens when OTC medicines expire, debunks myths, highlights the real dangers, and offers practical guidance for consumers.
Table of Contents
- The Importance of Expiration Dates on Medications
- What Happens to OTC Medications After Their Expiration Date?
- Risks and Dangers of Using Expired OTC Medications
- Risks of Specific OTC Medications After Expiry
- Factors Affecting Medication Stability and Safety
- Safe Storage Practices for OTC Medications
- Proper Disposal of Expired OTC Medications
- Frequently Asked Questions
- Key Takeaways
The Importance of Expiration Dates on Medications
All OTC and prescription medications in the United States must display an expiration date, as required by the Food and Drug Administration (FDA). This date indicates the last day the manufacturer guarantees full potency and safety of the drug when properly stored.
- Expiration dates are based on stability testing performed by the manufacturer. Beyond this date, the medication’s effectiveness and safety can no longer be assured.
- Drugs can degrade chemically or physically, making them less effective or, rarely, hazardous.
The expiration date applies not only to prescription drugs but also to OTC medicines, vitamins, supplements, and herbal products.
What Happens to OTC Medications After Their Expiration Date?
Once a medication passes its expiration date:
- The potency decreases as active ingredients may degrade over time.
- Some forms (especially liquids, creams, and injectable medications) are more susceptible to bacterial growth and contamination.
- Physical changes, such as discoloration, unusual smells, or changes in texture, may occur, signaling a loss of stability or contamination.
- Tablets and capsules generally remain stable longer than liquids, but even these lose effectiveness and may eventually degrade.
While most expired OTC pills and tablets stored properly in a cool, dry place are not likely to be acutely harmful, their reduced effectiveness can have significant consequences, especially for certain health conditions.
Risks and Dangers of Using Expired OTC Medications
Many believe that expired medications are simply less effective, but the truth is more nuanced. The main risks associated with using expired OTC medications include:
- Reduced effectiveness: Main concern for most medications. If a drug loses potency, it might not deliver the therapeutic benefit needed, putting health at risk.
- Potential toxicity: While rare, some medications, such as certain tetracyclines, can degrade into toxic compounds and pose direct health hazards.
- Failure to treat acute or chronic conditions: Relying on expired OTC drugs during emergencies (e.g., allergic reactions, asthma attacks) can be dangerous if the medication underperforms.
- Bacterial contamination: Especially common in expired liquids, suspensions, creams, eye drops, and antibiotics. This increases the risk of infection, irritation, or gastrointestinal upset.
- Resistance development: Using expired antibiotics or ointments with reduced potency may fail to eradicate bacteria, promoting resistance.
- Unintended consequences: Changes in smell, taste, or appearance could deter proper usage or signal chemical decomposition, further heightening risk.
Summary Table: Core Risks of Expired OTC Medications
| Risk | Explanation | Common Examples |
|---|---|---|
| Reduced Potency | Medication less effective, may not relieve symptoms as intended | Pain relievers, allergy meds, cold remedies |
| Contamination | Bacterial or fungal growth in old liquids or creams | Eye drops, ointments, syrups |
| Toxic Byproducts (Rare) | Certain drugs degrade into toxic or harmful chemicals | Aged tetracyclines, liquids |
| Unintended Effects | Changes in color, smell, or taste suggest instability | All medications |
Risks of Specific OTC Medications After Expiry
Some over-the-counter drugs are more susceptible to dangerous changes after their expiration date. Notable risks include:
- Liquid Medications: More prone to bacterial growth, cloudiness, and separation, leading to potential infections or reduced efficacy. This includes liquid cold remedies, cough syrups, antacids, and antibiotics.
- Pain Relievers (Ibuprofen & Acetaminophen): Generally safe a short period after expiry if stored properly, but potency wanes. For acetaminophen (Tylenol), after two to three years, effectiveness drops by about 20%. For ibuprofen (Advil, Motrin), the loss of potency is gradual, but the precise dose can no longer be guaranteed.
- Eye & Ear Drops: Risk of contamination and infection increases sharply after expiry, potentially leading to conjunctivitis, irritation, or even vision damage.
- Antacids & Allergy Tablets: Less risky in terms of toxicity but may not control heartburn or allergic reactions as well when potency drops.
- Antibiotic Creams/Ointments: Reduced effectiveness may allow minor wounds to become infected or resistant bacteria to thrive.
It is particularly dangerous to use expired medications for acute attacks (e.g., expired epinephrine for anaphylaxis), as underperformance could lead to severe health crises.
Factors Affecting Medication Stability and Safety
The safety and effectiveness of OTC medications can be affected by several factors besides the expiration date:
- Storage Conditions: Exposure to heat, sunlight, moisture, and air can degrade medication faster. Bathrooms and direct sunlight are higher risk spots for storing drugs.
- Original Packaging: Keeping medications in their original, sealed packaging helps maintain their stability longer.
- Physical or Chemical Form: Liquids and creams deteriorate faster than solid pills or tablets, making them more hazardous after expiry.
- Frequency of Opening: Opening and closing containers repeatedly introduces air and potential contaminants.
Safe Storage Practices for OTC Medications
- Store medications in a cool, dry place—kitchen cabinets and closets are better than bathrooms.
- Some drugs (such as insulin or probiotics) require refrigeration; always check the label or ask a pharmacist.
- Keep medications out of reach and sight of children and pets to avoid accidental ingestion.
- Periodically review your medicine cabinet and discard expired or questionable products.
- Store drugs in their original containers to prolong shelf life and ensure correct identification.
Proper Disposal of Expired OTC Medications
Improper disposal of expired medications is a public health and environmental issue. Throwing medicines in the trash or flushing them down the toilet can contaminate water supplies and harm wildlife. Follow these best practices:
- Use authorized drug take-back programs available at many pharmacies or local law enforcement agencies.
- If no take-back is available, mix expired medicines with coffee grounds, cat litter, or another unpalatable substance in a sealed bag before placing them in the trash.
- Remove or scratch out all identifying personal information from medicine containers before disposal.
- Never flush medicines unless labeled specifically for that method of disposal.
Frequently Asked Questions (FAQs)
Q: Is it ever safe to take expired OTC medication?
A: Some solid pills may retain partial potency after expiration, but safety and effectiveness can’t be guaranteed. For life-threatening conditions or infections, do not rely on expired drugs. In emergencies (e.g., severe allergy and no other option), taking an expired medication is better than nothing, but seek medical help immediately.
Q: What symptoms might occur from taking expired medications?
A: Most people experience ineffectiveness, but there are risks of stomach upset, ulcers, gastrointestinal bleeding, allergic reactions, or infection—particularly from expired liquids and ointments.
Q: Do all medications become toxic after expiration?
A: No. The vast majority do not become toxic, but exceptions exist (notably, some tetracyclines). Decreased effectiveness is a much more common issue.
Q: How can I tell if a medication has gone bad, aside from the date?
A: Any change in color, consistency, smell, or taste suggests it should be thrown away, regardless of the expiration date.
Q: Why are expiration dates relatively short?
A: Expiry dates reflect the period for which manufacturers guarantee full potency and quality, not necessarily the precise moment a medication ‘goes bad.’ Safety, legal, and logistical reasons factor in. Shelf life may be longer under optimal storage, but certainty declines after expiration.
Key Takeaways
- Do not use expired OTC medications unless absolutely necessary. Loss of potency is the main risk, but contamination and rare toxicity are concerns for certain products.
- Liquid medications, eye or ear drops, creams, and injectables pose the highest risk after expiration.
- Always store medications correctly and regularly check expiration dates.
- Use take-back programs for safe disposal and prevent environmental contamination or accidental ingestion.
- Consult your pharmacist or healthcare provider when in doubt about the safety or effectiveness of a medication.
Remember: While being frugal is important, it should never come at the expense of your health or safety. When it comes to medications, up-to-date is up-to-life.
References
- https://www.uhhospitals.org/blog/articles/2023/08/expired-medications-dangerous-or-just-less-effective
- https://www.centerwellpharmacy.com/articles/medication-disposals.html
- https://sarh.org/about-us/news/are-expired-medications-safe-to-use
- https://www.swedish.org/news/uf/690623258?streamid=3129983
- https://blog.providence.org/blog/how-bad-is-it-to-take-expired-medication-2
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7040264/
- https://health.clevelandclinic.org/can-you-take-expired-medicine
- https://www.health.harvard.edu/staying-healthy/is-it-ok-to-use-medications-past-their-expiration-dates
Read full bio of medha deb












