Colostrum vs Quercetin for Gut Barrier Repair: Mechanisms, Evidence, and Practical Use
Immune factors and antioxidants combine to preserve digestive tract integrity.
Gut barrier integrity is essential for nutrient absorption, immune defense, and overall health. Disruption of this barrier—known as “leaky gut” or increased intestinal permeability—has been linked to chronic inflammation, autoimmunity, metabolic disorders, and gastrointestinal diseases. Two of the most discussed nutraceutical interventions for supporting gut barrier repair are colostrum and quercetin. This article explores the mechanisms, scientific evidence, and the comparative roles of colostrum and quercetin in gut barrier restoration, offering guidance for practitioners, athletes, and individuals seeking optimal gut health.
Table of Contents
- Understanding the Gut Barrier: Structure and Function
- What is Colostrum?
- Colostrum: Mechanisms Supporting Gut Barrier Repair
- Colostrum: Scientific Evidence and Clinical Applications
- What is Quercetin?
- Quercetin: Mechanisms Supporting Gut Barrier Repair
- Quercetin: Scientific Evidence and Clinical Applications
- Colostrum vs Quercetin: A Comparative Table
- Practical Considerations: Choosing Between Colostrum and Quercetin
- Safety, Dosing, and Product Quality
- Frequently Asked Questions
Understanding the Gut Barrier: Structure and Function
The intestinal barrier is a selectively permeable layer—mainly the single-cell epithelium—that separates the internal environment from the gut lumen. It allows absorption of nutrients and water while blocking pathogens, toxins, and undigested macromolecules. Key components include:
- Epithelial cells connected by tight junctions
- Mucus layer produced by goblet cells
- Secretory IgA and antimicrobial peptides
- Gut-associated lymphoid tissue (GALT) for immune surveillance
Disruption refers to increased gut permeability, also called “leaky gut,” which is linked to chronic inflammation, autoimmune diseases, metabolic disorders, and gastrointestinal complaints.
What is Colostrum?
Colostrum is the first form of milk produced by mammals immediately after birth, containing high concentrations of immune factors, growth factors, and nutrients. Bovine colostrum (from cows) is widely used in dietary supplements for both children and adults due to its bioactive profile and safety record.
- Rich in immunoglobulins (Igs), especially IgG
- Contains lactoferrin, a multifunctional protein with antimicrobial actions
- Packed with growth factors like IGF-1 and transforming growth factor beta (TGF-β)
- Supplies cytokines, vitamins, and minerals for tissue repair and immune support
Colostrum: Mechanisms Supporting Gut Barrier Repair
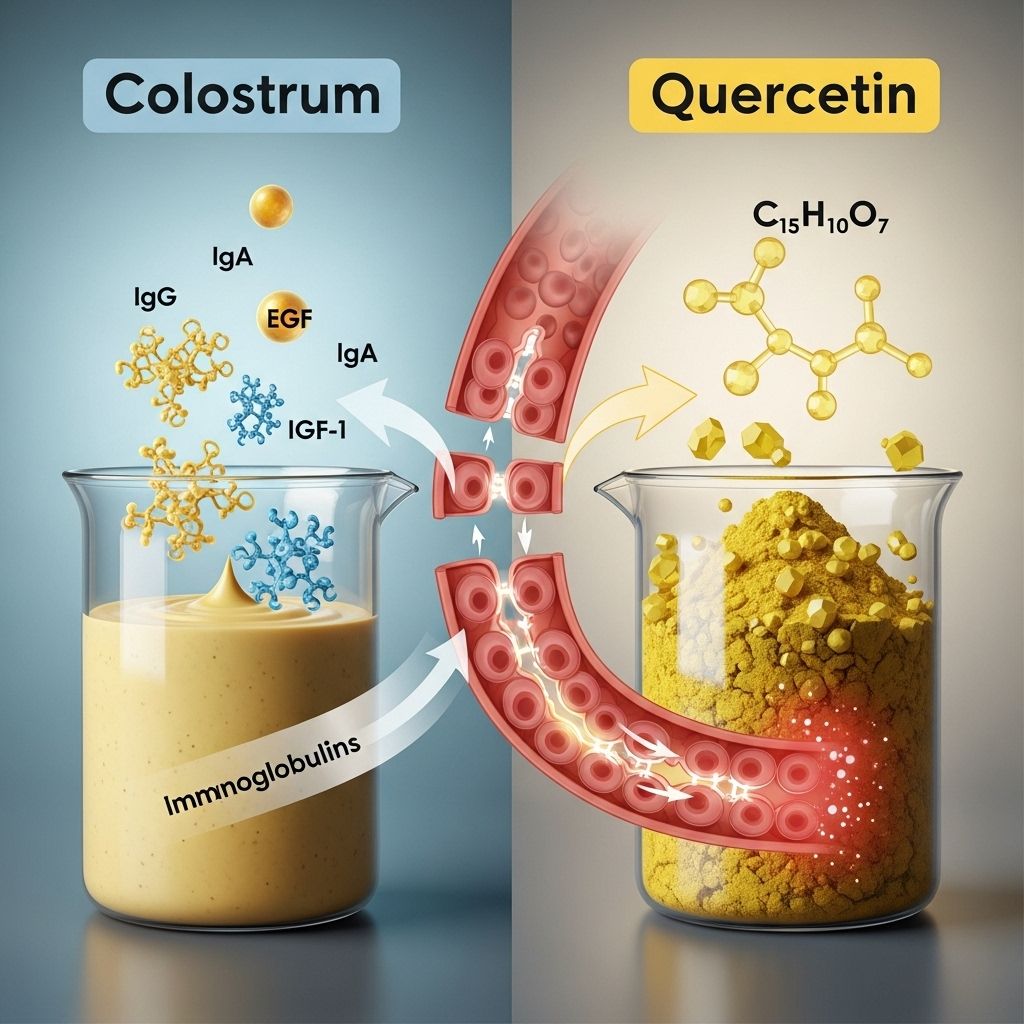
Bovine colostrum provides several bioactive compounds that synergistically support mucosal healing and the gut barrier:
- Immunoglobulins (Igs): Neutralize pathogens and block attachment to mucosa.
- Lactoferrin: Antimicrobial, anti-inflammatory, and supports growth of beneficial microbiota.
- Growth Factors (IGF-1, TGF-β): Promote proliferation and repair of epithelial cells, enhance villus growth, and stimulate tissue regeneration.
- Cytokines: Modulate immune response and dampen inflammation in the gut wall.
- Mucosal Barrier Enhancement: Encourages mucus production, fortifies tight junctions between epithelial cells, reducing permeability (“leakiness”).
- Endotoxin Neutralization: Reduces passage of toxins and bacteria into circulation, lowering systemic inflammation.
Colostrum: Scientific Evidence and Clinical Applications
Multiple lines of evidence demonstrate colostrum’s efficacy for gut barrier repair, especially under conditions of stress, injury, or inflammation:
- Inflammatory Bowel Disease (IBD): Human clinical trials indicate colostrum improves histological healing and reduces symptoms.
- NSAID-induced Enteropathy: Both animal and early human studies show colostrum mitigates damage and reduces increases in gut permeability caused by NSAIDs.
- Exercise-induced Gut Damage: Athletes taking colostrum report lower gut permeability and fewer GI symptoms after intensive exercise.
- Infectious Diarrhea and Surgical Stress: Supplementation reduces stool zonulin (a marker of permeability) and supports barrier restoration in patients recovering from GI infections or surgery.
- Microbiome Support: Associated with favorable shifts in gut microbiota composition.
However, many studies are small, heterogeneous in product/formulation, and often focus on specific populations (e.g., athletes, patients with gut disease). More rigorous and standardized research is needed for widespread clinical recommendations.
Limitations and Gaps
- Variable dosing and product quality in studies
- Most trials are short-term
- Scarcity of research in healthy general populations
What is Quercetin?
Quercetin is a plant-derived polyphenol—a type of flavonoid—naturally abundant in onions, apples, berries, and leafy greens. It is well documented as an antioxidant and anti-inflammatory agent, and is commonly used in nutraceutical formulations targeting gut, immune, and metabolic health.
Quercetin: Mechanisms Supporting Gut Barrier Repair
Quercetin’s multiple actions benefit the gut barrier by:
- Enhancing Tight Junction Integrity: Promotes the expression of tight junction proteins (occludin, claudins, ZO-1), thereby reinforcing the physical barrier between epithelial cells.
- Anti-inflammatory Activity: Suppresses NF-κB and pro-inflammatory cytokines (TNF-α, IL-6), dampening chronic mucosal inflammation.
- Antioxidant Effects: Neutralizes ROS (reactive oxygen species), protecting epithelial cells from oxidative damage.
- Mitigating Endotoxin Effects: Reduces systemic inflammation triggered by microbial products translocating across a leaky gut.
- Gut Microbiota Modulation: Fosters beneficial bacteria, which in turn support mucosal integrity.
Data from animal models, cell studies, and some human trials support these effects, although research is ongoing and somewhat less extensive compared to colostrum.
Quercetin: Scientific Evidence and Clinical Applications
- Cell and Animal Studies: Demonstrated decreases in gut permeability under inflammatory, infectious, and oxidative stress conditions.
- Human Evidence: Limited clinical studies show improved markers of permeability and reduced GI symptoms, especially in cases of exercise-induced stress or inflammatory conditions. More large-scale trials are needed.
- Chronic Disease and Gut Disorders: Observational data suggests benefit in various chronic inflammatory and metabolic syndromes where gut barrier compromise is common.
Quercetin’s broad effects on inflammation and oxidative stress translate well into gut barrier protection, but comparative studies with colostrum are rare, and the direct clinical evidence remains more limited overall.
Colostrum vs Quercetin: A Comparative Table
| Feature | Colostrum | Quercetin |
|---|---|---|
| Source | Animal-derived (bovine milk) | Plant-derived (flavonoid/polyphenol) |
| Main Bioactive Compounds | Immunoglobulins, lactoferrin, growth factors (IGF-1, TGF-β), cytokines | Flavonoid with antioxidant, anti-inflammatory activity |
| Mechanisms of Gut Barrier Support | Enhances mucosal immunity, stimulates epithelial repair, strengthens tight junctions, supports microbiome | Enhances tight junction proteins, antioxidant, anti-inflammatory, modulates microbiota |
| Clinical Evidence | Strongest for IBD, exercise-induced permeability; emerging evidence in surgery, infection | Mostly preclinical & small human studies; more human data needed for gut barrier repair |
| Additional Health Benefits | Immune boosting, tissue repair, possible microbiome support | Systemic anti-inflammatory, metabolic and vascular support |
| Safety/Side Effects | Generally safe; avoid in milk allergy/intolerance | Generally safe; high doses may cause headaches, tingling, or drug interactions |
| Best Use Cases | Gut injury (IBD, infection, NSAID use), athletic recovery, post-surgical healing | Chronic inflammation, adjunct for metabolic & allergy disorders, everyday antioxidant support |
Practical Considerations: Choosing Between Colostrum and Quercetin
- Colostrum may be preferred for overt gut barrier compromise or clinical gut injury (e.g., IBD, NSAID-induced damage, post-infection, post-surgery).
- Quercetin is appealing for individuals seeking plant-based, anti-inflammatory, and antioxidant benefits, or as an adjunct in milder cases of gut dysfunction and for long-term wellness support.
- Combination Use: There is theoretical synergy—colostrum heals the mucosal surface and recruits growth factors, while quercetin modulates inflammation and oxidative stress. However, clinical trials examining their combined effect are lacking.
Consultation with a healthcare provider or clinical nutritionist is advisable, especially when addressing known digestive disorders or chronic illness.
Safety, Dosing, and Product Quality
- Colostrum: Doses in studies range from 10g to 60g/day. Lower retail doses may not match those used in clinical research. Generally contraindicated for people with severe dairy allergies.
- Quercetin: Common supplemental doses are 250-1000mg/day. Well-tolerated, but high doses may interact with medications or cause mild side effects (headache, tingling).
- Quality Control: Both supplements are poorly regulated. Choose products from reputable manufacturers with third-party testing.
Frequently Asked Questions (FAQs)
Q: What is the main difference between colostrum and quercetin for gut health?
A: Colostrum is an animal-derived source packed with immune proteins and growth factors for mucosal healing, while quercetin is a plant-derived polyphenol mostly providing antioxidant and anti-inflammatory support.
Q: Is it safe to take colostrum and quercetin together?
A: There are no known interactions, and theoretical synergy may exist, but always consult with a healthcare professional before combining nutraceuticals.
Q: Who should avoid colostrum or quercetin?
A: Avoid colostrum if you have milk allergies or severe lactose intolerance. Quercetin is generally safe, but high doses should be avoided during pregnancy, lactation, or with certain medications (anticoagulants, antibiotics).
Q: How long does it take to see results for gut barrier repair?
A: Benefits may start within a few weeks, but most studies are short-term (4–12 weeks). Chronic conditions may require longer supplementation under supervision.
Q: Are there other lifestyle factors important for gut barrier health?
A: Yes—diet rich in prebiotics and fiber, exercise, stress management, and avoiding unnecessary NSAIDs or alcohol support gut integrity alongside targeted supplementation.
Key Takeaways
- Colostrum offers direct mucosal and immune repair for clinically significant gut barrier issues.
- Quercetin provides plant-based anti-inflammatory and antioxidant support for milder or adjunctive gut barrier aid.
- Quality, dosage, and patient-specific factors are crucial for efficacy. Consultation with healthcare professionals is strongly advised for gut barrier concerns.
References
- https://www.news-medical.net/health/Colostrum-for-Adults-Boosting-Immunity-Gut-Health-and-Recover.aspx
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8228205/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9227274/
- https://www.cspi.org/article/should-you-take-bovine-colostrum-supplement
- https://pubs.rsc.org/en/content/articlehtml/2024/fb/d3fb00256j
- https://www.nature.com/articles/s41390-024-03379-x
Read full bio of Sneha Tete












