Cluster vs. Sinus Headaches: Distinguishing Features, Diagnosis, and Treatment
Identifying the subtle signs that separate two common headache types for better care.
Headaches are a frequent complaint encountered in both clinical practice and daily life. Among the myriad headache disorders, cluster headaches and sinus headaches are two of the most commonly mistaken types due to overlapping symptoms but they are fundamentally different in their underlying causes, symptoms, and management approaches. This article provides a thorough comparison, exploring both conditions in depth to aid patients and clinicians in accurate identification and effective treatment.
Table of Contents
- Overview of Cluster and Sinus Headaches
- Definition and Basic Differences
- Underlying Causes
- Symptoms: Similarities and Key Differences
- Diagnosis: Clinical Approach and Challenges
- Treatment and Management Strategies
- Side-by-Side Comparison Table
- Prevalence and Risk Factors
- When to See a Doctor
- Frequently Asked Questions
- Summary and Key Takeaways
Overview of Cluster and Sinus Headaches
Distinguishing between cluster headaches and sinus headaches is critical, as they stem from different causes and require specific treatments. Despite some overlapping symptoms, these headaches vary greatly in their intensity, duration, and associated features.
Definition and Basic Differences
- Cluster Headache: A rare, primary headache disorder characterized by severe, strictly one-sided pain usually around the eye, occurring in repeated, cyclical patterns or “clusters.” The pain is often excruciating and accompanied by autonomic symptoms on the affected side, like tearing and nasal congestion.
- Sinus Headache: A secondary headache resulting from inflammation of the paranasal sinuses, often associated with sinus infection. The pain is generally dull, deep, and persistent, corresponding to the location of the affected sinus and usually accompanied by symptoms of sinus disease such as nasal discharge and congestion.
Underlying Causes
- Cluster Headache:
- Considered a vascular headache, typically classified as a trigeminal-autonomic cephalalgia.
- Exact cause is unknown, but involves activation of the trigeminal nerve and hypothalamic dysfunction.
- Not typically due to structural abnormalities, though secondary cases may rarely exist (tumors, infections).
Understanding the differences between sinus infections and other conditions is crucial for proper diagnosis and treatment. Discover more in our explanation of Sinus Infection vs. Cold: Key Differences, Causes, Symptoms, and Treatments Explained. This resource clarifies common misconceptions and helps in recognizing when to seek medical advice. - Sinus Headache:
- Caused by inflammation or infection (sinusitis) of the paranasal sinuses.
- May result from bacterial, viral, or allergic processes leading to mucosal swelling and blocked drainage.
Symptoms: Similarities and Key Differences
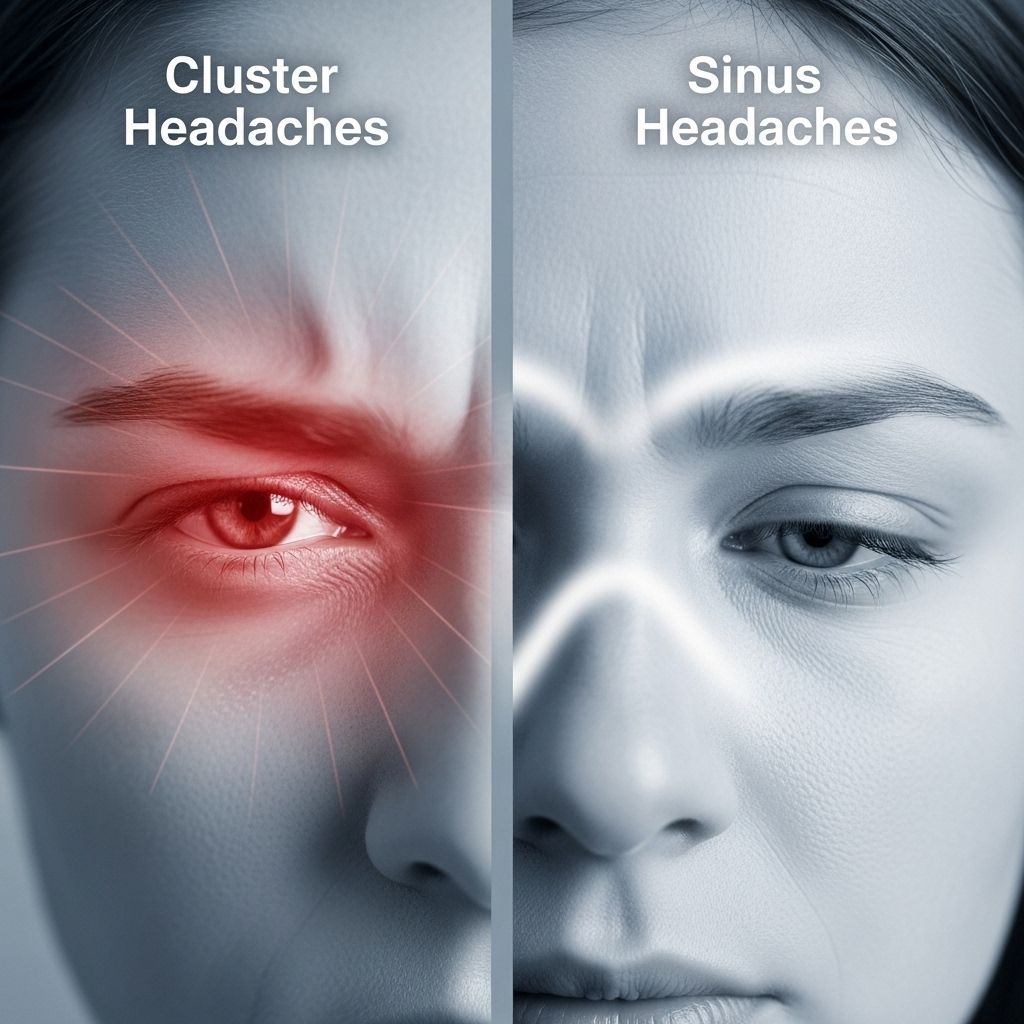
While symptoms sometimes overlap—particularly facial pain and nasal congestion—a closer look reveals distinguishing patterns and associations.
Similarities
- Pain around the eyes, forehead, and cheeks
- Nasal symptoms: stuffiness or discharge
- Potential for tearing of the eyes
Key Distinguishing Features
| Feature | Cluster Headache | Sinus Headache |
|---|---|---|
| Pain Location | Strictly unilateral, periorbital/temple | Often bilateral or unilateral in sinus regions: forehead, cheeks, nose |
| Pain Nature | Sharp, burning, or stabbing; excruciating | Deep, constant, pressing/dull |
| Onset | Sudden; reaches peak in 5–10 minutes | Gradual; worsens with bending or sudden movement |
| Duration | Typically 30–90 minutes (15–180 min range) | Persists as long as infection/inflammation continues (often days to weeks) |
| Frequency | Can occur several times daily, during “clusters” (up to 8/day) | No cyclical grouping; often worse in morning, improves during day |
| Associated Features | Lacrimation, conjunctival redness, eyelid droop, restlessness, sweating | Nasal congestion/discharge, fever, fatigue, sometimes cough |
| Triggers | Alcohol, smoking, changes in sleep, histamine | Respiratory infections, allergies, weather changes |
| Restlessness During Attack | Common—patients pace or rock due to agony | Unusual; patients tend to rest quietly |
| Chronicity | Can be episodic or chronic (year-round) | Rarely chronic unless underlying sinus disease persists |
Diagnosis: Clinical Approach and Challenges
Given overlapping symptoms, careful clinical history and proper examination are essential for accurate diagnosis. Misdiagnosis is common; many cluster headaches are mistaken for sinus headaches and vice versa.
Diagnostic Methods
- History and Pattern: Document timing, duration, quality, associated symptoms, and triggers.
- Physical Examination: Check for signs of infection (fever, nasal discharge), Horner syndrome (ptosis, miosis, anhidrosis) during cluster attacks, and facial tenderness over sinuses.
- Imaging: MRI recommended for cluster headaches to exclude secondary causes, especially if presentation is atypical or with warning signs (neurologic deficits, persistent changes).
- ENT Evaluation: For sinus headaches, nasal endoscopy and sinus imaging (CT) may confirm sinus infection or anatomical abnormalities.
- Therapeutic Response: Cluster headaches may respond to specific abortive medications (e.g., sumatriptan, high-flow oxygen), whereas sinus headaches improve slowly with infection/inflammation treatment.
Common Causes of Misdiagnosis
- Overlapping autonomic features (tearing, stuffy nose, red eye)
- Pain localized to similar facial regions
- Lack of awareness that cluster headaches often have nasal symptoms without infection
Treatment and Management Strategies
Cluster Headache Management
- Acute Therapy: Inhaled high-flow oxygen, subcutaneous or intranasal sumatriptan. Other fast-acting triptans may be used.
- Preventive Therapy: Verapamil (first-line), corticosteroids for short-term prevention, lithium, or other prophylactic medications in chronic cases.
- Other Approaches: Occipital nerve blocks, deep brain or sphenopalatine ganglion stimulation, rarely surgery in refractory cases.
- Address Triggers: Avoid alcohol and other known precipitants during cluster periods.
Sinus Headache Management
- Targeted Treatment: Address underlying sinus pathology (infection, inflammation).
- Pharmacotherapy: Antibiotics for bacterial sinusitis, nasal corticosteroids, decongestants, or antihistamines in allergic cases.
- Ancillary Measures: Steam inhalation, nasal saline irrigation, pain relief (acetaminophen, ibuprofen).
- Surgical Intervention: Rare; may be considered for chronic or recurrent sinus disease not responsive to standard therapy.
Note: When sinus congestion or infection is successfully treated, sinus headache typically resolves. Cluster headaches, being primary disruptions, often require long-term management.
Side-by-Side Comparison: Cluster vs. Sinus Headache
| Characteristic | Cluster Headache | Sinus Headache |
|---|---|---|
| Commonality | Rare (about 1/1000 adults) | More frequent, especially with upper respiratory infections |
| Gender Predilection | Traditionally more common in men; incidence in women rising | No gender predilection |
| Associated Mood Effects | Anger, restlessness, anxiety during attack | Fatigue, malaise, irritability |
| Chronic Course | Often chronic or recurrent (episodic or chronic types) | Rarely chronic; tied to persistent sinus disease |
Prevalence and Risk Factors
- Cluster Headaches:
- Estimated to affect 0.1% of adults; considered rare
- Risk factors: male sex, family history, smoking, alcohol use, specific chronobiologic factors
- Sinus Headaches:
- Common, especially following upper respiratory infections, allergies, or anatomical sinus issues
- Risk factors: frequent colds, allergic rhinitis, structural nasal/sinus abnormalities
When to See a Doctor
- Headache that is sudden, severe, or different from typical pattern
- Headache accompanied by fever, neurologic changes, vision loss, confusion, or persistent vomiting
- Pain not improving with over-the-counter measures or clearly linked to sinus infection that does not respond to appropriate treatment
- For recurring or disabling headaches affecting quality of life
Frequently Asked Questions (FAQs)
Q: Can sinus infections cause cluster headaches?
A: Cluster headaches are classified as primary headaches, meaning they are not usually caused by another medical condition. However, rare cases exist where sinusitis may trigger cluster-like attacks, and both conditions can occur simultaneously. Imaging is needed if the presentation is unusual or unresponsive to standard therapy.
Q: How can I distinguish a sinus headache from a cluster headache at home?
A: Sinus headaches often follow upper respiratory infections, feature constant dull pain that worsens on bending, and come with symptoms like thick nasal discharge or fever. Cluster headaches produce much more severe, sharp pain focused around one eye, occur in defined attacks, and are accompanied by autonomic features like tearing and restlessness.
Q: Can both headaches occur together?
A: Yes, cluster and sinus headaches can occasionally appear in the same patient, making diagnosis more complex. A careful history and sometimes imaging are needed to separate the two.
Q: Are cluster headaches dangerous?
A: While not life-threatening, cluster headaches are among the most painful conditions known. Sudden changes or new neurological symptoms warrant urgent evaluation to rule out other causes.
Q: What should I do if my headache treatment is not working?
A: Seek re-evaluation by a healthcare provider, as the underlying diagnosis may need reviewing and treatments can be adjusted based on clinical findings and response.
Summary and Key Takeaways
Accurately recognizing the distinguishing features of cluster and sinus headaches allows for faster relief and prevents mismanagement. While both may involve pain in similar locations and accompanying nasal symptoms, consider these core differences:
- Cluster headaches are rare, strictly one-sided, brief but severe, and present with autonomic features and marked restlessness.
- Sinus headaches are more frequent, associated with sinus inflammation/infection, have a gradual onset, and typically improve with appropriate treatment of sinus disease.
- In all cases of severe, recurrent, or atypical headaches, or where sinus infection does not resolve with routine care, seek thorough medical evaluation for tailored therapy and to exclude dangerous secondary causes.
Understanding these differences assures more accurate diagnosis, optimal treatment, and improved quality of life for those affected by headache disorders.
References
- https://nasodren.com/difference-between-cluster-and-sinus/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3795873/
- https://medlineplus.gov/ency/article/000786.htm
- https://www.excedrin.com/you-plus-excedrin/head-health-101/migraine-vs-headache/
- https://my.clevelandclinic.org/health/diseases/5003-cluster-headaches
- https://www.excedrin.com/headache-and-migraine-academy/headaches/headache-causes/headache-vs-migraine-whats-the-difference/
- https://www.webmd.com/migraines-headaches/ss/slideshow-headaches-types
- https://www.bansalneuro.com/sinus-cluster-tension-headaches-phoenix.html
- https://kanehallbarry.com/blog/understanding-the-different-types-of-headaches/
Read full bio of Sneha Tete












