Chronic Sinus Issues and Gut Inflammation: Understanding the Hidden Link for Lasting Relief
Unlock comfort by balancing your microbiome and immune support for clearer breathing.
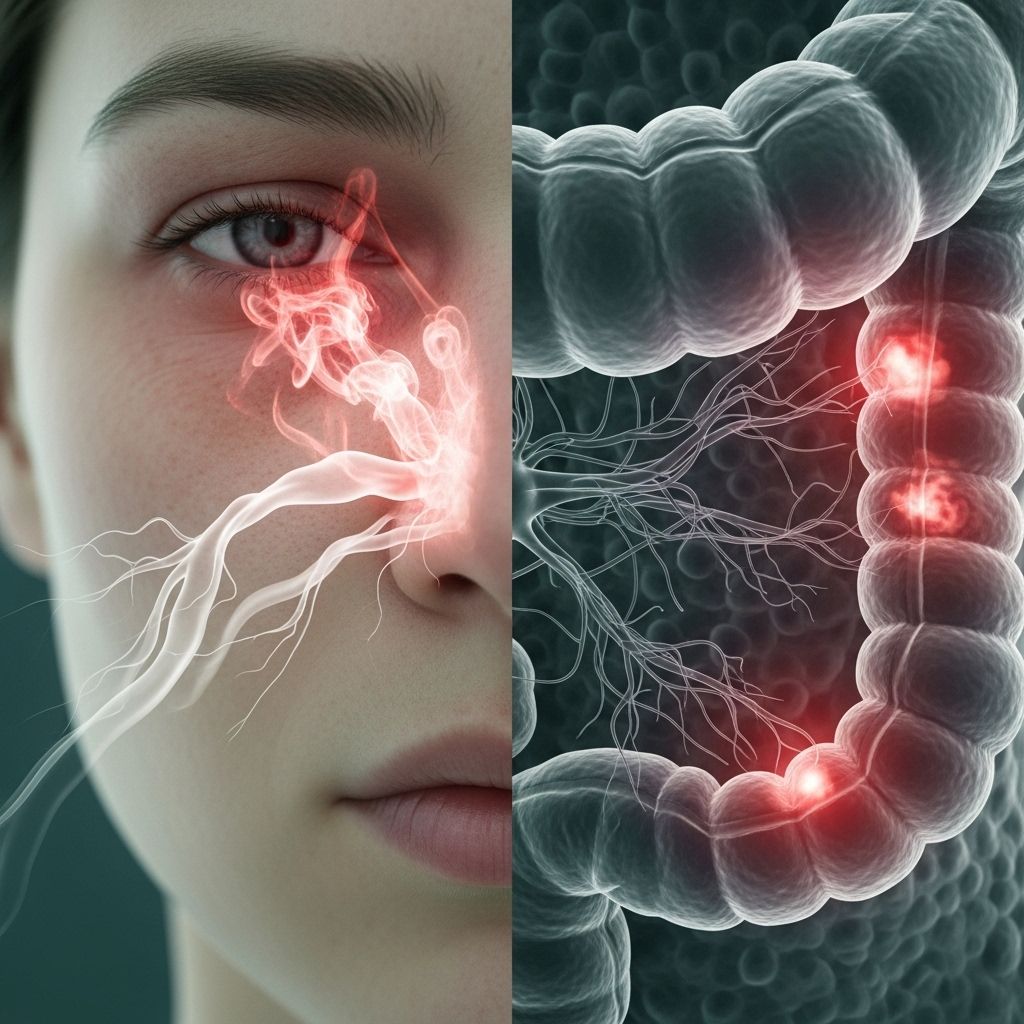
Chronic sinus problems affect millions worldwide, often causing persistent congestion, facial pain, and a decreased quality of life. While treatments usually focus on the sinuses themselves, emerging research reveals a powerful connection between chronic sinus inflammation and the health of your gut. This comprehensive article explores the evolving science behind this gut-sinus axis, how alterations in gut microbiota and inflammation can fuel unending sinus issues, and integrative strategies for recovery and prevention.
Table of Contents
- Overview: Chronic Sinus Issues and Their Causes
- How the Gut and Sinuses Are Connected
- The Science of Gut Inflammation and Its Systemic Effects
- The Microbiome: Key Player in Sinus and Gut Health
- Biofilm: A Hidden Driver of Chronic Infection
- Food Intolerances, Allergies, and their Impact
- Restoring Gut and Sinus Health: Approaches and Strategies
- Prevention Tips and Lifestyle Modifications
- Frequently Asked Questions
- References
Overview: Chronic Sinus Issues and Their Causes
Chronic sinusitis, also known as chronic rhinosinusitis (CRS), is characterized by inflammation of the tissues lining the sinuses lasting for 12 weeks or longer. Symptoms typically include nasal congestion, facial pain or pressure, postnasal drip, headaches, impaired sense of smell, and persistent fatigue.
Traditionally, the causes of chronic sinusitis were believed to be local: lingering infections, nasal polyps, anatomical blockages, or allergies. Medical interventions over the years have focused on:
- Antibiotics for bacterial infections
- Decongestants and antihistamines
- Intranasal or oral corticosteroids
- Surgical interventions to clear blockages
However, for many patients, symptoms persist despite these measures, suggesting underlying factors beyond the sinuses themselves .
How the Gut and Sinuses Are Connected
Recent discoveries reveal a substantial link between gut health and chronic sinus inflammation. The gut and upper respiratory tract, including the sinuses, are both lined with mucous membranes and are interconnected by the body’s immune, nervous, and lymphatic systems. This relationship, often called the “gut-sinus axis,” helps explain why gastrointestinal disturbances can manifest as respiratory or sinus symptoms .
Key mechanisms include:
- Immune signaling: About 70-80% of the immune system resides in the gut, meaning gut dysfunction and dysbiosis (microbial imbalance) can send inflammatory signals systemically, including to the sinuses.
- Leaky gut: Damage to the gut lining (increased intestinal permeability) allows particles, allergens, and bacteria to enter the bloodstream, triggering widespread immune activation and inflammation—even in distant sites like the sinuses .
- Microbial cross-talk: Microbiota imbalance in the gut is often mirrored in the microbial communities of the sinuses, affecting local immunity and susceptibility to infection .
The Science of Gut Inflammation and Its Systemic Effects
Several studies highlight the connection between gut inflammation and chronic sinus disorders:
- People with chronic sinusitis often exhibit gut microbiota imbalances, particularly reduced levels of beneficial bacteria like Bifidobacterium and Akkermansia muciniphila .
- Gut inflammation can impair immune regulation, leading to excessive or chronic inflammation in various tissues, including the sinuses .
- Certain autoimmune and allergic conditions, which are driven by immune dysregulation often originating in the gut, are frequently co-present with chronic sinusitis .
These findings underscore the importance of treating chronic sinus inflammation as a systemic issue rather than an exclusively local one.
Systemic Effects of Gut Inflammation
- Increased circulating inflammatory cytokines: These amplifying signals can lead to chronic swelling in distant organs, including sinus mucosa.
- Altered immune tolerance: Overactive immune responses to food antigens or gut microbes may increase the likelihood of allergies and sinus sensitivities.
- Metabolite production: Byproducts of an imbalanced gut microbiome can circulate and impact the function of the epithelial barriers throughout the body.
The Microbiome: Key Player in Sinus and Gut Health
Microbiota, the diverse ecosystem of bacteria, viruses, and fungi inhabiting our gut and sinuses, are central to immune health and inflammation control. Disruption of microbial balance (dysbiosis) has been repeatedly associated with chronic inflammatory disorders.
Key findings:
- Chronic sinusitis patients frequently show less microbial diversity in both nasal and intestinal microbiota .
- After repeated antibiotic use for sinus infections, not only the sinus but also the gut microbiome can become depleted, lowering protective bacteria and fostering conditions for antibiotic-resistant or opportunistic pathogens .
- Yeast overgrowth, particularly Candida, can develop after long-term antibiotics and contribute to stubborn biofilms in sinuses and the gut, fueling persistent symptoms .
| Healthy Microbiome Features | Dysbiotic Microbiome |
|---|---|
| High diversity & abundance of beneficial bacteria | Reduced diversity, overgrowth of pathogenic species or yeast |
| Strong epithelial barriers (gut & sinus lining) | Increased permeability (“leaky” membranes) |
| Balanced immune signaling | Overactive or suppressed immune response |
| Symptom-free sinus and gut function | Chronic sinus congestion, pain, GI symptoms |
Biofilm: A Hidden Driver of Chronic Infection
Biofilms are complex communities of microbes encased in a protective matrix, allowing them to evade the immune system and resist antibiotics. In the context of chronic sinusitis:
- Harmful biofilms (often from yeast overgrowth or pathogenic bacteria) can form in both the gut and sinuses, perpetuating chronic infection and inflammation .
- Antibiotics are often ineffective against biofilms, and attempting to eradicate them can sometimes worsen gut dysbiosis .
- Natural biofilm disruptors (like colostrum, lactoferrin, digestive enzymes, and xylitol) and specific probiotics may help restore microbial balance and break the cycle .
Food Intolerances, Allergies, and their Impact
Food allergies and intolerances are increasingly recognized as contributors to both gut inflammation and sinus dysfunction. The typical offenders include:
- Dairy products
- Gluten-containing grains
- Highly processed foods
- Common allergenic foods (soy, eggs, nuts)
When individuals with a predisposition (such as a leaky gut) consume trigger foods, their immune system mounts a localized and systemic inflammatory response, often resulting in sinus congestion, pressure, and headaches .
Identifying and eliminating these foods from the diet has been shown to reduce both gut and sinus symptoms in many patients with chronic problems.
Restoring Gut and Sinus Health: Approaches and Strategies
Given the interwoven relationship between gut inflammation and chronic sinusitis, a multidisciplinary approach is often necessary for lasting symptom control.
Core Steps to Restore Gut and Sinus Harmony
- Microbiome testing and targeted probiotics: Personalized testing can reveal deficiencies in beneficial bacteria or the presence of harmful species. Quality probiotics (especially containing *Lactobacillus* and *Bifidobacterium* strains) and prebiotic fibers can help re-establish a balanced microbiome .
- Anti-inflammatory nutrition: Consuming a diet rich in plant-based foods, healthy fats, antioxidant-rich fruits and vegetables, bone broth, and fermented foods can help reduce inflammation and heal both gut and sinus linings .
- Elimination of dietary triggers: Identify and avoid foods that provoke inflammatory responses—dairy, gluten, or processed foods—and consider working with a nutritionist for a tailored plan .
- Natural biofilm disruptors: Supplements like colostrum, digestive enzymes, and xylitol may help disperse persistent biofilms .
- Stress reduction: Chronic stress profoundly disrupts gut immunity. Integrate relaxation techniques like deep breathing, yoga, and mindfulness to support the gut-sinus axis .
- Avoid unnecessary antibiotics: Reserve antibiotics for acute, confirmed bacterial infections, as overuse can worsen both gut and sinus dysbiosis .
- Support natural detoxification: Dandelion, spirulina, and cilantro, along with adequate hydration, can assist the body’s removal of inflammatory toxins .
Prevention Tips and Lifestyle Modifications
Reducing the risk of chronic sinus and gut inflammation requires ongoing attention to daily habits. Here are practical prevention strategies:
- Maintain a diverse, fiber-rich diet to encourage healthy microbial diversity
- Incorporate fermented foods (e.g., yogurt, kefir, sauerkraut) and occasional prebiotic supplements
- Minimize ultra-processed foods, artificial sweeteners, and added sugars
- Ensure good sleep hygiene to support immune balance
- Address allergies early to prevent sinus and gut flares
- Monitor and manage environmental toxins (e.g., mold, air pollution)
For at-risk individuals—especially those with a history of antibiotic use, autoimmunity, or severe allergies—a proactive, gut-focused strategy can be transformative.
Frequently Asked Questions (FAQs)
Q: Are most chronic sinus infections actually caused by bacteria?
A: No. Over 90% of chronic sinusitis cases have underlying inflammatory or immune-based causes rather than infections. Gut inflammation, immune imbalance, or allergies are often to blame .
Q: How does gut dysbiosis lead to persistent sinus symptoms?
A: Dysbiosis impairs gut barrier function and immune regulation, increasing inflammatory mediators in the bloodstream, which can inflame sinus tissues, perpetuate congestion, and promote the growth of pathogenic biofilms .
Q: What signs suggest both gut and sinus involvement?
A: Individuals often notice a pattern of gastrointestinal discomfort (bloating, irregular stools, food intolerances) along with sinus congestion, headaches, and postnasal drip. Symptom flares may coincide with consuming trigger foods .
Q: Can probiotics alone resolve chronic sinus issues?
A: Probiotics are helpful, especially multi-strain, high-quality supplements, but they are most effective when combined with dietary changes, avoidance of triggers, and lifestyle modifications .
Q: Should antibiotics be used repeatedly for chronic sinusitis?
A: Repeated courses are discouraged, as they can worsen both gut and sinus microbiome imbalance, making symptoms more persistent. Antibiotics should be reserved for confirmed bacterial cases that do not resolve spontaneously .
References
- Victoria Bailey Health & Wellness. “Your Chronic Sinus Inflammation Could Be Affecting Your Brain.”
- NCBI (PMC10521374). “Alteration of indicator gut microbiota in patients with chronic sinusitis.”
- ION Intelligence of Nature. “The Surprising Connection Between Your Gut and Your Sinuses.”
- Dr. Will Cole. “Chronic Sinus Infections? Here’s How To Stop Them For Good.”
References
- https://victoriabaileyhealthandwellness.com/your-chronic-sinus-inflammation-could-be-affecting-your-brain/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10521374/
- https://intelligenceofnature.com/blogs/ion/gut-sinus-connection
- https://drwillcole.com/why-you-keep-getting-sinus-infections-exactly-what-to-do-about-it/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4982648/
- https://www.youtube.com/watch?v=UoBgYUaStSA
- https://greaterknoxent.com/the-link-between-gut-health-and-ent-health/
- https://www.rupahealth.com/post/a-functional-medicine-approach-to-sinusitis
- https://www.cvsurgicalgroup.com/does-diet-have-an-impact-on-sinus-infections-and-allergies/
Read full bio of medha deb












