Chronic Pain and Mental Health Cycle: Strategies to Break the Vicious Loop
Integrated therapies and support deliver relief and strengthen emotional wellbeing.
Chronic Pain and Mental Health Cycle: Breaking It
Chronic pain is a complex and disruptive condition that reshapes lives. Often lasting for months or even years, it is closely woven with mental health struggles, forming a feedback cycle that is difficult to escape. Breaking this cycle requires understanding how pain and psychological distress interact—and employing strategies that address both simultaneously.
Table of Contents
- Understanding Chronic Pain
- How Chronic Pain Impacts Mental Health
- The Biopsychosocial Cycle of Pain
- Strategies to Break the Cycle
- Integrated Care: Treating Both Mind and Body
- Practical Tips for Patients and Caregivers
- Frequently Asked Questions (FAQs)
- Helpful Resources
Understanding Chronic Pain
Chronic pain is defined as pain persisting for three months or longer—extending well beyond the normal healing period. Unlike acute pain, which serves as a warning signal, chronic pain often loses its protective purpose, evolving into a standalone health issue.
Common sources include:
- Arthritis
- Fibromyalgia
- Back or neck pain
- Migraines
- Nerve-related conditions
Chronic pain may be constant or intermittent, mild or severe, but its impact is always significant.
How Chronic Pain Impacts Mental Health
Living with chronic pain creates a heavy psychological burden. Individuals often report:
- Depression: Rates are significantly higher in those with chronic pain than the general population, affecting up to 45% of sufferers. Feelings of hopelessness can arise from constant discomfort and diminished ability to participate in activities.
- Anxiety: Persistent worry about pain attacks, future disability, finances, or relationships can lead to ongoing stress and anxiety disorders.
- Mood Disorders: Chronic pain affects sleep, increases irritability, and disrupts daily routines.
- Post-Traumatic Stress Disorder (PTSD): Those with traumatic injury-related pain may also develop PTSD.
Social Isolation is common, as pain can limit mobility and participation, eroding social supports and increasing loneliness.
Key Statistics
| Condition | Prevalence Among Chronic Pain Sufferers |
|---|---|
| Depression | 35%–45% |
| Anxiety | Up to 50% |
| Social Isolation | Common but variable |
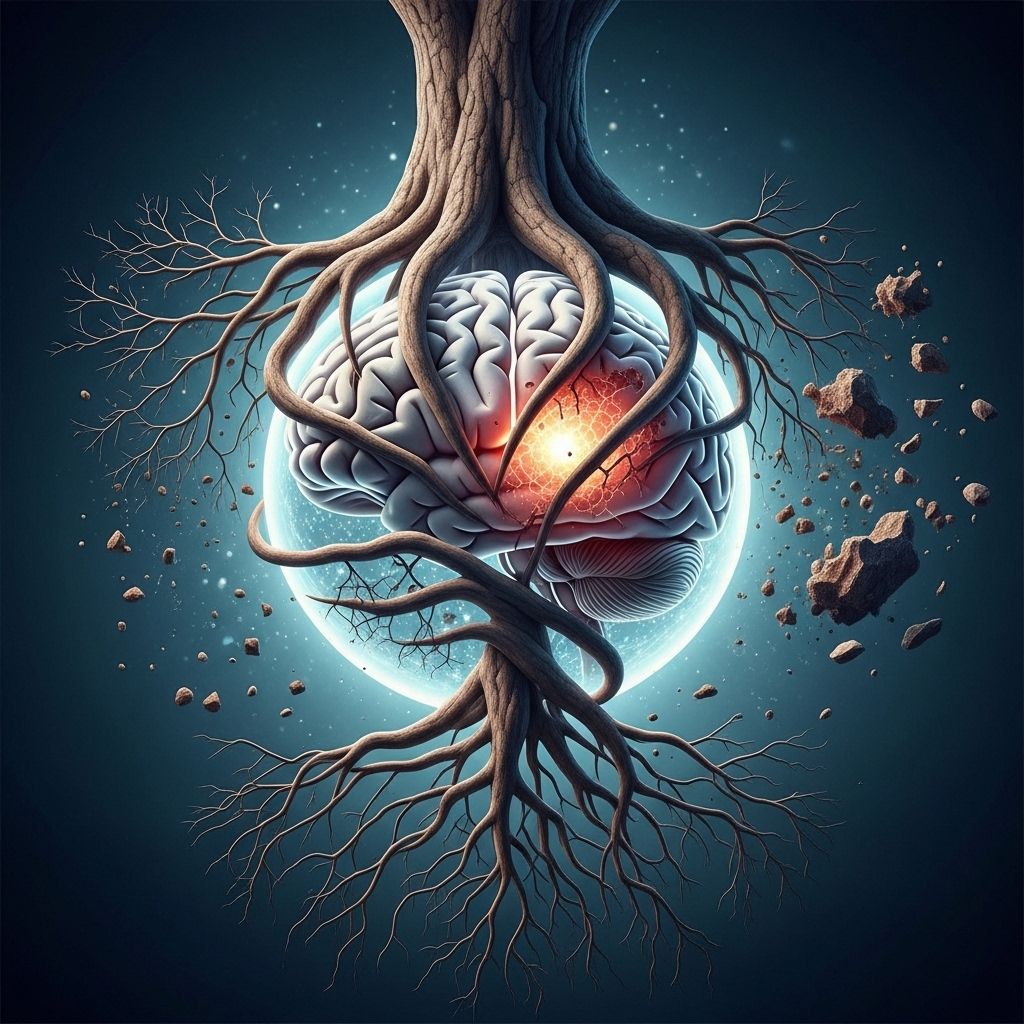
The Biopsychosocial Cycle of Pain
The connection between chronic pain and mental health isn’t one-way. The interaction forms a biopsychosocial cycle, where:
- Pain drives emotional distress: Persistent discomfort leads to frustration, stress, and negative thoughts.
- Emotional distress amplifies pain: Depression and anxiety can sensitize the nervous system, making pain feel more severe—a phenomenon known as central sensitization.
- Disrupted sleep and fatigue: Poor sleep worsens pain and mental health, fueling irritability and cognitive difficulties.
- Reduced movement and social activity: Physical limitations lower mood and reinforce feelings of helplessness.
- Substance use risk: Some individuals turn to alcohol or drugs to cope, increasing risk for substance use disorders.
Genetic, neurochemical, and environmental factors blend together, creating a self-perpetuating feedback loop.
Illustration of the Cycle
- Pain → Sleep Problems → Anxiety/Depression → Increased Pain Sensitivity → Greater Pain → Social Isolation → Further Emotional Distress → More Pain
Breaking any part of this loop can reduce suffering and improve outcomes.
Strategies to Break the Cycle
Recovery starts by treating both the physical and the mental dimensions of chronic pain. No single intervention suffices; a comprehensive, multidisciplinary approach works best.
1. Psychotherapy and Psychological Support
- Cognitive Behavioral Therapy (CBT): Helps reframe negative thinking and reduce pain perception. CBT lessens depression and increases coping skills.
- Mindfulness-Based Stress Reduction (MBSR): Meditation and mindfulness techniques ease anxiety and reduce pain intensity by changing how the brain processes discomfort.
- Acceptance and Commitment Therapy (ACT): Encourages acceptance of pain and focuses on living a meaningful life despite ongoing symptoms.
- Peer Support Groups: Sharing experiences in group settings reduces isolation and builds resilience.
2. Medical Management
- Medications: Antidepressants and anticonvulsants can effectively treat both pain and mood disorders for some individuals.
- Pain specialist care: Collaboration with specialists ensures best practices and targeted therapies.
- Physical rehabilitation: Gradual movement, physical therapy, and occupational therapy help restore function and reduce pain flare-ups.
3. Lifestyle Modifications
- Exercise: Light aerobic activities (walking, swimming, stretching) boost endorphins, improve mood, and decrease pain sensitivity.
- Nutrition: Balanced diets rich in antioxidants and anti-inflammatory nutrients support healing and mental clarity.
- Sleep hygiene: Setting regular sleep routines and reducing stimulants improve restorative sleep.
4. Stress Management
- Relaxation Techniques: Breathing exercises, muscle relaxation, visualization, and biofeedback calm the body’s stress response.
- Mindful awareness of triggers: Awareness helps break reactive cycles and find healthier coping mechanisms.
- Creative therapies: Art, music, and recreational activities provide emotional release and foster a sense of mastery.
5. Social Support and Communication
- Family and friends: Supportive relationships buffer stress and facilitate healing.
- Community engagement: Volunteering, joining clubs, or engaging with faith communities reduces isolation.
- Professional guidance: Social workers, peer support specialists, and health workers create holistic support networks.
Integrated Care: Treating Both Mind and Body
Multidisciplinary care models—where doctors, mental health professionals, physical therapists, and support specialists collaborate—offer the most effective solutions for breaking the chronic pain-mental health cycle. This approach may include:
- Comprehensive assessment of both pain and emotional factors.
- Shared decision-making between patient and care team.
- Regular screening for depression, anxiety, and PTSD in pain clinics.
- Combination of psychotherapy, medication, and physical treatments.
Treating both conditions improves treatment adherence, functional outcomes, and overall quality of life.
Practical Tips for Patients and Caregivers
- Track symptoms: Maintain a pain diary to monitor triggers, mood, and patterns.
- Set realistic goals: Small achievements build confidence and create momentum.
- Prioritize self-care: Schedule downtime and pleasurable activities to recharge.
- Educate yourself: Learn about your condition and evidence-based treatments.
- Communicate: Share feelings with trusted supporters or health providers.
- Seek help early: Early intervention yields better outcomes and prevents worsening of symptoms.
- Be patient: Recovery is gradual; persistence pays off.
Frequently Asked Questions (FAQs)}
Q: How common is depression in people with chronic pain?
A: Research indicates that 35% to 45% of individuals with chronic pain report significant depressive symptoms.
Q: Can treating mental health help reduce physical pain?
A: Yes. Interventions like psychotherapy and certain medications affect brain pathways, reducing both emotional distress and pain perception.
Q: What is central sensitization?
A: Central sensitization is a process where prolonged stress or untreated mental health issues amplify pain signals in the nervous system, increasing sensitivity to pain.
Q: Are lifestyle changes really effective?
A: Lifestyle modifications—including exercise, better sleep, and stress reduction—significantly influence both pain and emotional well-being, improving overall outcomes.
Q: How can caregivers help?
A: Caregivers should encourage positive coping, provide emotional and social support, facilitate access to care, and educate themselves about the interplay of pain and mental health.
Helpful Resources
- American Pain Society: Patient guides and support
- Mental Health America: Resources for coping with pain and depression
- National Institute of Neurological Disorders and Stroke: Chronic pain research
- Local pain clinics specializing in integrated care
- Online support groups and peer forums for chronic pain and mental health
Conclusion
Chronic pain and mental health form an intertwined cycle that is as much psychological as it is physical. By tackling both aspects with integrated, evidence-based strategies, one can break free from the cycle and move toward healing and improved quality of life.
References
- https://www.ptcoa.com/the-link-between-chronic-pain-and-mental-health-breaking-the-cycle
- https://www.psychiatry.org/news-room/apa-blogs/chronic-pain-and-mental-health-interconnected
- https://www.cumedicine.us/health-insights/chronic-pain-and-mental-health
- https://www.sepainandspinecare.com/the-psychological-impact-on-chronic-pain/
- https://painspecialty.net/the-link-between-stress-and-chronic-pain-how-to-break-the-cycle/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10326936/
- https://www.americanpainconsortium.com/patient-resources/news/2024/february/the-link-between-chronic-pain-and-mental-health-/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5494581/
Read full bio of Sneha Tete












