Chronic Inflammation and Dermal Blood Vessel Damage: Mechanisms, Consequences, and Therapies
Disrupted blood flow fuels swelling and redness, pointing to new treatment possibilities.
Chronic Inflammation & Dermal Blood Vessel Damage
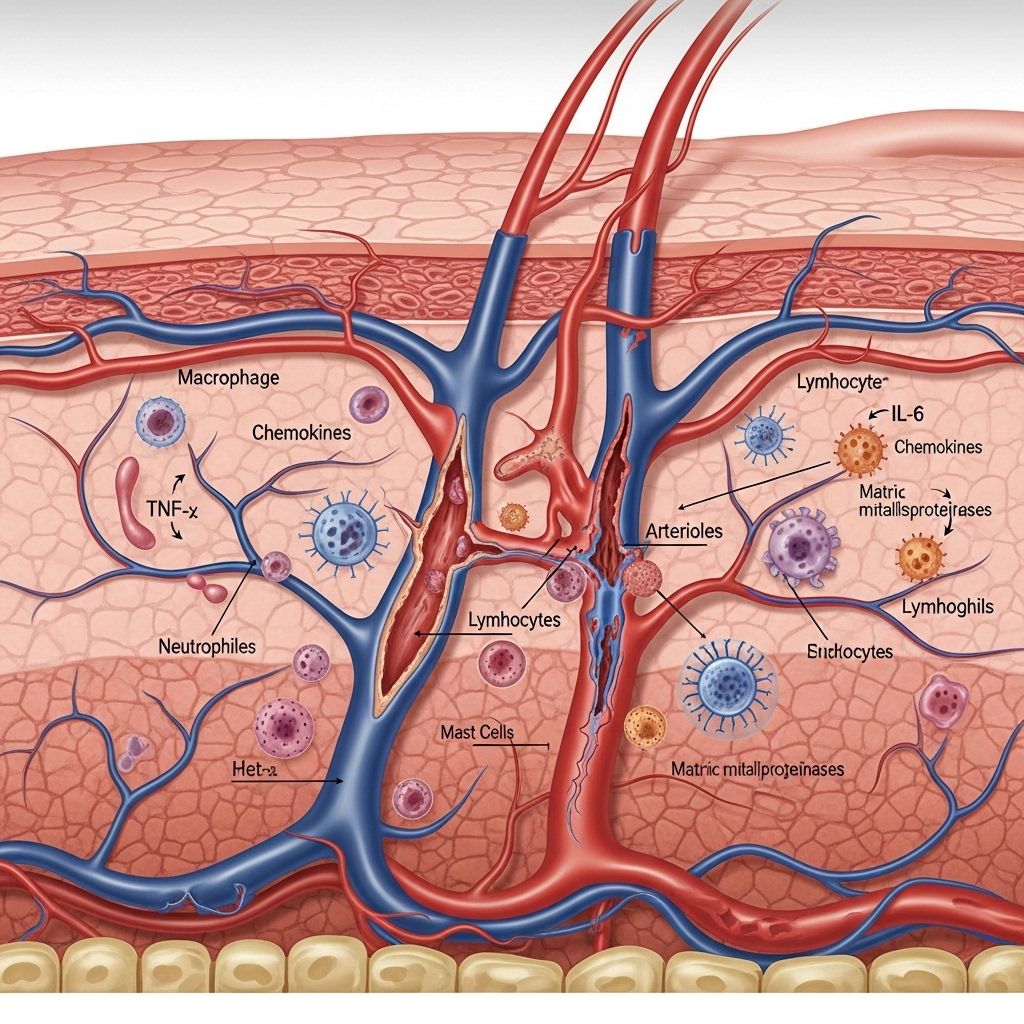
Chronic inflammation is a persistent immune response that can lead to significant tissue remodeling, dysfunction, and damage. In the skin, one of the most affected systems is the intricate network of blood and lymphatic vessels comprising the dermal vasculature. Understanding how chronic inflammation interacts with and damages these vessels is vital, as this process contributes to common skin diseases such as psoriasis, chronic dermatitis, and systemic inflammatory disorders. This article provides an in-depth exploration of the mechanisms by which chronic inflammation harms dermal blood vessels, the resultant pathophysiological consequences, and the evolving therapeutic approaches to prevent or reverse such damage.
Table of Contents
- Introduction
- Structure and Function of Dermal Blood Vessels
- Chronic Inflammation: An Overview
- Mechanisms of Dermal Blood Vessel Damage in Chronic Inflammation
- Vascular Remodeling and Hyperpermeability
- Immune-Vascular Axis in Chronic Skin Disease
- Clinical Consequences of Vascular Damage
- Therapeutic Strategies Targeting Vascular Dysfunction
- Conclusion
- Frequently Asked Questions (FAQs)
Introduction
The skin is not only a barrier against environmental threats but also a dynamic immunological organ. At the center of its reaction to injury and infection are networks of blood and lymphatic vessels. Chronic inflammation continuously activates these vessels, resulting in structural and functional changes that underpin much of the visible and symptomatic damage in chronic skin disease1. Understanding these processes is crucial for developing advanced therapies targeting skin inflammation at its vascular root.
Structure and Function of Dermal Blood Vessels
The dermal circulatory system comprises:
- Superficial capillary loops: Provide nutrients and oxygen to the upper dermis and epidermis.
- Deep vascular plexus: Supplies larger blood flow to the skin, acts in thermoregulation and wound healing.
- Lymphatic vessels: Drain interstitial fluid and carry immune cells to and from local lymph nodes.
This system ensures tissue oxygenation, nutrient supply, thermoregulation, immune surveillance, and repair. Blood vessels in the dermis are lined by endothelial cells that regulate the selective passage of fluids, cells, and proteins between the blood and tissue—sometimes called the vascular barrier.
Chronic Inflammation: An Overview
Inflammation is generally a protective response to infection or injury. When well-regulated and transient, it facilitates healing. However, chronic inflammation is a long-term, dysregulated process marked by continual leukocyte infiltration, cytokine release, and tissue adaptation. In skin, this creates a sustained environment of danger signals and aberrant tissue remodeling, with blood vessels acting both as targets and mediators of damage1,2.
Mechanisms of Dermal Blood Vessel Damage in Chronic Inflammation
Vascular changes are both a cause and effect of ongoing inflammation. Key mechanisms include:
- Endothelial activation: Inflammatory mediators (such as VEGF-A, TNF-α, IL-6, IL-1β) activate endothelial cells, leading to increased expression of adhesion molecules (E-selectin, ICAM-1, VCAM-1), which facilitate leukocyte attachment and migration1.
- Vascular hyperpermeability: Activated endothelium becomes leaky, enabling plasma proteins and immune cells to exit the circulation, causing tissue edema and contributing to the “tumor” (swelling) of inflammation.
- Angiogenesis and vascular remodeling: Prolonged presence of VEGF and other pro-angiogenic cytokines induce the formation of new, larger, and more tortuous vessels—”remodeled” vasculature prone to chronic leakiness and dysfunction2.
- Lymphangiogenesis: Chronic inflammation also induces growth of new lymphatic vessels, primarily via VEGF-C and VEGF-D, but lymphatic function is often impaired, contributing to poor drainage and persistent edema.
- Oxidative stress: High oxidative burden and nitric oxide overproduction lead to endothelial injury and promote chronic inflammation-driven vascular disease.
Table 1 summarizes the sequence of molecular and cellular events by which chronic inflammation exerts its deleterious effects on blood vessels in the skin.
| Mechanism | Mediators | Result |
|---|---|---|
| Endothelial activation | VEGF-A, TNF-α, IL-1β, IL-6 | Leukocyte adhesion/migration; vessel leakiness |
| Hyperpermeability | VEGF-A, histamine, NO | Edema, plasma extravasation |
| Angiogenesis | VEGF-A, PDGF, HIF | Enlarged, aberrant vessels; chronic inflammation support |
| Lymphangiogenesis | VEGF-C, VEGF-D | New lymphatic growth but impaired drainage |
| Oxidative stress | ROS, nitric oxide | Endothelial dysfunction, vessel damage |
Vascular Remodeling and Hyperpermeability
In the setting of chronic inflammation, marked changes occur to the skin’s vasculature:
- Hyperpermeable and enlarged vessels: Vessels expand (dilated) and lose tight junction integrity, making them persistently leaky. This underlies ongoing redness, heat, and swelling seen in inflamed skin1.
- Angiogenesis: Driven by overexpressed growth factors (particularly VEGF-A), new blood vessels form but are frequently malformed, fragile, and contribute to disease chronicity.
- Lymphatic dysfunction: Although new lymphatic vessels also develop, they are often poorly functional. Experimental data show that enhancing lymphangiogenesis or boosting lymphatic function can reduce inflammation and promote healing1.
These processes fuel a self-perpetuating inflammatory cycle: leaky vessels allow more immune cells and fluid into tissues, increasing local pressure and further recruiting inflammatory mediators.
Immune-Vascular Axis in Chronic Skin Disease
The interaction between immune signaling and vascular remodeling is now recognized as a critical axis in skin inflammation:
- Activated endothelium expresses cell adhesion molecules, directing the migration of inflammatory leukocytes from bloodstream to skin tissue.
- Persistent angiogenesis not only supports increased blood flow and supply of inflammatory cells but also alters the tissue environment, making it favorable to chronic inflammation as seen in psoriasis and other chronic dermatoses2,4.
- Disordered capillaries and network structures (such as “glomerulus-like” loops) become a hallmark of chronic lesions, further amplifying disease2.
Critically, these vascular changes are now seen not just as consequences but as active drivers of chronic inflammatory disease.
Clinical Consequences of Vascular Damage
Chronic inflammation-induced blood vessel damage in the skin results in numerous clinical and pathological effects:
- Edema: Hyperpermeable vessels leak fluid and proteins into the skin, causing persistent swelling.
- Erythema and warmth: Dilated vessels increase blood flow, underlying visible redness and increased temperature.
- Impaired barrier and tissue repair: Edema and lack of proper lymphatic drainage disrupt tissue architecture, slow wound healing, and enhance susceptibility to infection or fibrosis.
- Histological changes: In diseases like psoriasis, there are widened and tortuous dermal capillaries, sometimes organizing into “glomeruloid” masses2,4.
- Chronic pain and itch: Fluid accumulation and inflammatory mediator release activate skin nerve endings.
- Accelerated aging and photodamage: UV exposure exacerbates inflammation-induced vascular injury, worsening aging signs and increasing skin cancer risk.
Case Example: Psoriasis
Psoriasis, a prototypical chronic inflammatory skin disorder, illustrates these mechanisms clearly. Its pathology includes:
- Vastly increased pro-angiogenic signals (especially VEGF-A)
- Widened, distorted, and leaky capillaries in dermal papillae
- Persistent infiltration by inflammatory leukocytes (T cells, neutrophils)
The end result is the formation of scaly, red, thickened plaques with persistent symptoms and a chronic course2,4.
Therapeutic Strategies Targeting Vascular Dysfunction in Chronic Skin Inflammation
Research into treatments now increasingly focuses on the vasculature—inhibiting aberrant blood vessel activity or boosting defective lymphatic function to break the cycle of chronic inflammation.
- Anti-angiogenic therapy: Inhibitors targeting VEGF and its receptors can reduce new blood vessel formation, leakage, and infiltration of immune cells in experimental models4.
- VEGFR-3 activation: Stimulating this lymphatic growth factor receptor improves lymphatic drainage and reduces inflammation in preclinical models1.
- Blocking endothelial adhesion molecules: Treatments aimed at E-selectin or ICAM-1 can reduce leukocyte entry and inflammation.
- Immunomodulatory therapies: Classic immunosuppressive drugs (e.g., corticosteroids, cyclosporine) and newer biologics (e.g., TNF-α inhibitors) can indirectly reduce vascular activation.
- Targeting neuropilin-2 (NRP-2): NRP-2 modulation represents a new avenue for altering vascular remodeling and lymphatic function in chronic inflammation2.
Ongoing research aims to determine which combination of these approaches is most effective for different chronic inflammatory skin diseases.
Conclusion
Chronic inflammation of the skin leads to a feedback loop of dermal blood vessel remodeling, hyperpermeability, lymphatic dysfunction, and sustained tissue injury. These complex interactions underscore the need for therapies that target both the immune system and the vascular compartment. Recognizing and addressing vascular damage in chronic skin inflammation offers potential for improved treatment outcomes and restoration of healthy skin function.
Frequently Asked Questions (FAQs)
Q: What are the main signs of dermal blood vessel damage in chronic inflammation?
A: The main clinical signs are persistent redness (erythema), swelling (edema), visible dilated or distorted blood vessels, impaired wound healing, and occasionally chronic pain or itch due to increased inflammation and nerve sensitization.
Q: Why do blood vessels become leaky in chronic inflammatory skin diseases?
A: Inflammatory mediators like VEGF-A and cytokines activate the endothelium, causing loosening of cell junctions. This makes blood vessels hyperpermeable, which allows proteins and immune cells to escape into surrounding tissues, resulting in edema and inflammation1.
Q: Can chronic inflammation destroy blood vessels permanently?
A: Yes. Prolonged inflammation can cause irreversible remodeling, atrophy, or occlusion of smaller vessels, leading to chronic tissue hypoxia, scarring, and impaired regenerative responses.
Q: How is lymphatic function involved in chronic skin inflammation?
A: With chronic inflammation, lymphatic vessels expand (lymphangiogenesis) but may function poorly, reducing effective fluid drainage and perpetuating local swelling and inflammation1,2.
Q: Are there new treatments specifically targeting blood or lymphatic vessels in chronic skin disease?
A: Research is progressing in anti-angiogenic therapies (such as VEGF inhibitors), pro-lymphangiogenic agents (VEGFR-3 agonists), and modulation of endothelial cell adhesion, aiming to interrupt the cycle of vessel activation and chronic inflammation4.
References:
1. “The cutaneous vascular system in chronic skin inflammation.” PMC.
2. “Blood and lymphatic vascular systems during inflammation.” Journal of Inflammation Research.
4. “Targeting the Immune-Vascular Axis in Psoriasis.” Psoriasis.org.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3398151/
- https://www.dovepress.com/interaction-between-blood-vasculatures-and-lymphatic-vasculatures-duri-peer-reviewed-fulltext-article-JIR
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7610698/
- https://www.psoriasis.org/targeting-the-immune-vascular-axis-in-psoriasis/
Read full bio of Sneha Tete












