Exploring the Causes of Compromised Barrier Function in the Skin and Gut: Mechanisms, Risks, and Solutions
Disruptions in microbiome balance and immune regulation can weaken natural defenses.
Causes of Compromised Barrier Function (Skin, Gut)
The skin and gut serve as our primary interfaces with the external world, forming dynamic barriers that protect against pathogens, toxins, and physical injury. Recent advances in medical research have revealed that the health of these barriers is tightly interconnected, and that disruptions on one front can reverberate throughout the body. This article explores the mechanisms underlying compromised barrier function in both the skin and gut, highlighting the contributing factors, consequences, and potential interventions.
Table of Contents
- Overview of Barrier Function
- The Skin Barrier: Structure and Function
- The Gut Barrier: Components and Purpose
- The Gut–Skin Axis: Bidirectional Influence
- Primary Causes of Barrier Dysfunction
- Role of the Microbiome
- Inflammation and Immune Dysregulation
- Environmental and Lifestyle Factors
- Clinical Consequences of Barrier Compromise
- Restoring Barrier Function: Interventions and Strategies
- Frequently Asked Questions (FAQ)
Overview of Barrier Function
The body relies on epithelial barriers—the skin and gut being the largest and most exposed—to maintain homeostasis and defend against external threats. A healthy barrier prevents penetration by pathogens and allergens, regulates fluid loss, and allows selective absorption of nutrients. Dysfunction in either barrier can result in increased permeability, inflammation, and disease susceptibility.
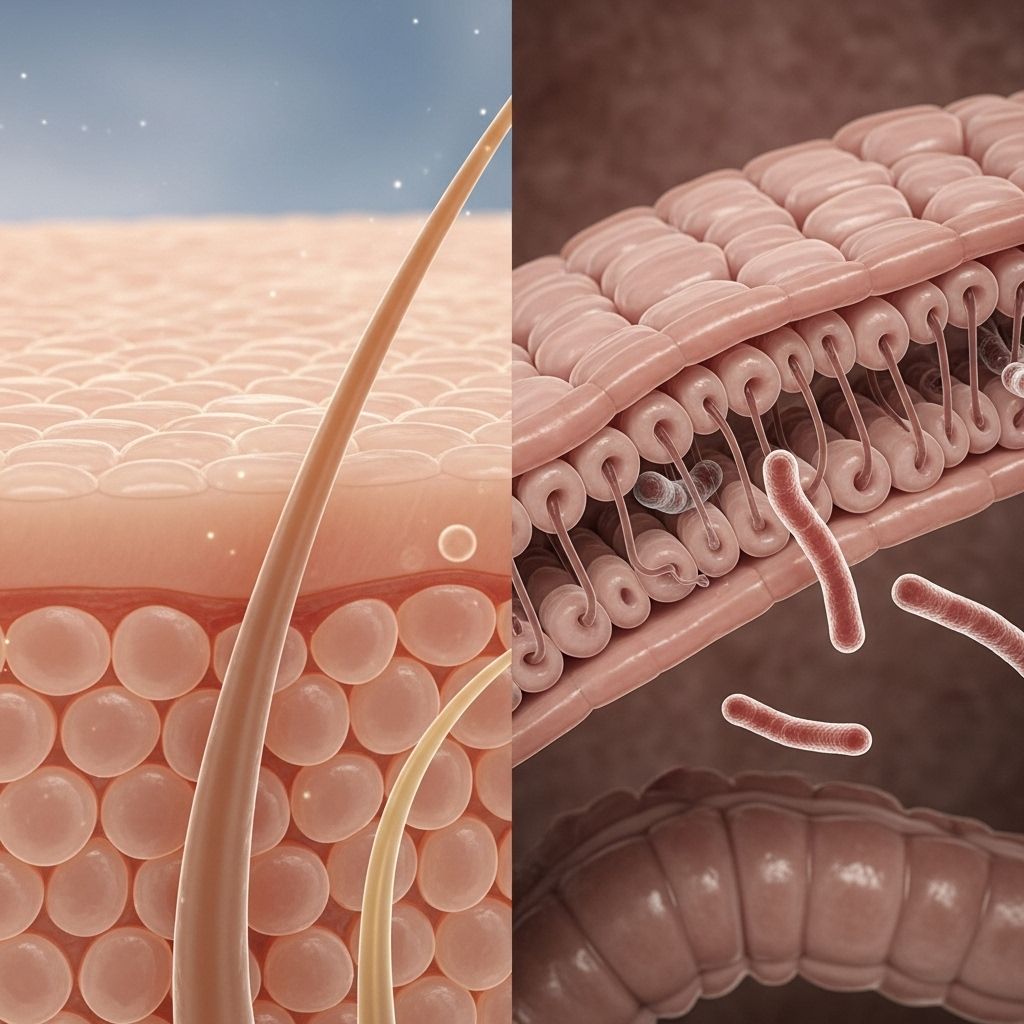
The Skin Barrier: Structure and Function
The skin barrier primarily consists of the outermost layer, the stratum corneum, composed of corneocytes held together by lipids. Key functions include:
- Protection against microbial invasion and toxins
- Prevention of water loss (transepidermal water loss, TEWL)
- Regulation of immune responses
The integrity of the stratum corneum is supported by intercellular lipids, natural moisturizing factors, and tight junction proteins. Disruption leads to increased permeability, making the skin more vulnerable to inflammation and infection.
The Gut Barrier: Components and Purpose
The gut barrier is composed of several layers:
- Physical barrier: A single layer of epithelial cells connected by tight junctions
- Mucus layer: Secreted by goblet cells, preventing direct contact of microbes with the epithelium
- Immunological barrier: Includes secretory IgA, antimicrobial peptides, and immune cell surveillance
- Microbial barrier: The gut microbiota competes with pathogens for resources and modulates immune function
When this barrier is compromised—a condition commonly termed leaky gut—microbial products, food antigens, and toxins gain access to systemic circulation, triggering immune responses and inflammation.
The Gut–Skin Axis: Bidirectional Influence
Research confirms a bidirectional connection between the gut and skin:
- Microbial metabolites (such as short-chain fatty acids) and immune signals travel between gut and skin
- Gut barrier dysfunction is implicated in inflammatory skin conditions, including eczema, psoriasis, acne, and rosacea
- Skin injury and inflammation can alter the intestinal microbiome and induce gut permeability in animal models
Understanding the gut–skin axis is crucial, as interventions targeting one barrier can exert effects on the other.
Primary Causes of Barrier Dysfunction
A range of factors may disrupt the skin and gut barrier, leading to compromised function and disease. These include:
- Microbiome imbalances (dysbiosis)
- Chronic inflammation
- Genetic predisposition
- Diet and nutrient deficiencies
- Environmental and lifestyle influences
Microbiome Imbalances (Dysbiosis)
Both the skin and gut harbor diverse communities of microorganisms that contribute to barrier integrity. Dysbiosis—a reduction in microbial diversity or an overgrowth of harmful species—can:
- Promote inflammation via immune activation
- Reduce production of protective metabolites (e.g., SCFAs)
- Lead to colonization by opportunistic pathogens
Clinical studies report that patients with eczema, psoriasis, or acne often exhibit gut dysbiosis, including increased abundance of Bacteroidetes, Enterobacteriaceae, and Clostridium perfringens, all linked to heightened inflammation and barrier compromise.
Chronic Inflammation and Immune Dysregulation
Persistent activation of immune responses damages barrier integrity. Causes include:
- Autoimmune disorders (e.g., atopic dermatitis, inflammatory bowel disease)
- Allergic reactions and mast cell activation
- Migrating inflammatory immune cells between skin and gut
Barrier compromise allows antigens to enter the body, perpetuating a vicious cycle of inflammation and tissue injury.
Genetic Predisposition
Genetic factors impact susceptibility to barrier disruption:
- Mutations in filaggrin (involved in skin barrier formation) increase eczema risk
- Polymorphisms affecting tight junction proteins in the gut raise leaky gut risk
Diet and Nutrient Deficiencies
The gut absorbs nutrients necessary for skin and barrier health. Poor diet and malabsorption can:
- Reduce levels of vitamins (A, D), minerals (zinc), and fatty acids
- Increase skin dryness and impair cell regeneration
- Trigger flare-ups after consumption of processed foods, sugar, or dairy
Environmental and Lifestyle Influences
- Exposure to environmental irritants, pollutants, and harsh skincare products
- Frequent antibiotic use disrupts both gut and skin microbial communities
- Chronic stress and sleep deprivation impact immune and barrier function
- Physical injury (scratching, trauma) increases permeability and microbial entry
Role of the Microbiome in Barrier Health
The skin and gut microbiome play protective and regulatory roles:
- Fermentation of dietary fibers in the gut yields short-chain fatty acids (SCFAs) with anti-inflammatory effects beneficial for skin and gut integrity.
- Commensal microbes help stimulate regulatory immune cells, limiting excessive inflammatory responses.
- Disruption of microbial balance leads to colonization by pathogenic species, increased inflammation, and barrier permeability.
Microbiome-targeted interventions—such as probiotics (Bifidobacterium, Lactobacillus), prebiotic fibers, and dietary changes—help restore barrier function in many skin and gut disorders.
Inflammation and Immune Dysregulation
Barrier compromise is both a cause and consequence of sustained inflammation. Mechanisms include:
- Release of cytokines (IL-4, IL-33) after skin injury, increasing gut permeability
- Activation of mast cells, leading to allergic reactions and worsening barrier integrity
- Migration of activated immune cells and inflammatory mediators between skin and gut, perpetuating disease
This systemic inflammatory loop explains why many chronic conditions exhibit both skin and gut symptoms.
Environmental and Lifestyle Factors
External challenges to barrier function include:
- Harsh cleansers, frequent bathing, and overuse of topical treatments stripping the skin’s protective lipids
- Pollutant and allergen exposure triggering immune activation
- Excessive antibiotic use depleting beneficial microbes (gut/skin dysbiosis)
- Psychological stress and poor sleep elevating systemic inflammation and reducing barrier resilience
- Dietary patterns rich in processed foods, sugar, and additives exacerbating gut permeability and skin flare-ups
Clinical Consequences of Barrier Compromise
When either barrier function is impaired, the risk for a spectrum of disorders increases:
| Barrier Compromised | Associated Conditions | Main Symptoms |
|---|---|---|
| Skin | Atopic dermatitis, eczema, psoriasis, acne, infections | Dryness, itching, redness, inflammation, increased sensitivity |
| Gut | Inflammatory bowel disease, celiac disease, food allergies, IBS | Bloating, abdominal pain, irregularity, fatigue, malabsorption |
Systemic manifestations are common when inflammation spreads, linking gut symptoms to skin outbreaks and vice versa.
Restoring Barrier Function: Interventions and Strategies
Strategies to repair and maintain barrier integrity target root causes:
- Dietary Modifications: Reducing processed foods, increasing fiber, fermented foods, omega-3 fatty acids
- Probiotics and Prebiotics: Supplementing beneficial microbial strains and fibers to nourish them
- Topical Therapies: Using ceramide-rich moisturizers and gentle cleansers for skin barrier repair
- Immune Modulation: Targeted therapies (e.g., biologics) to reduce chronic inflammation
- Stress Management & Sleep Hygiene: Mitigating psychological stress and optimizing sleep
- Judicious Antibiotic Use: Preserving microbiome diversity with targeted rather than broad-spectrum therapies
Emerging treatments focus on restoring microbial diversity and tight junction integrity, thereby reducing inflammation and promoting overall health.
Frequently Asked Questions (FAQ)
Q: What is barrier function, and why is it important?
Barrier function refers to the capacity of the skin and gut to selectively block harmful substances while permitting beneficial nutrients and water to pass. This prevents infections, regulates immunity, and maintains hydration.
Q: What is ‘leaky gut’?
Leaky gut describes a state of increased intestinal permeability, often due to tight junction disruption, allowing toxins, microbes, and food particles to enter the bloodstream.
Q: How does the gut microbiome impact skin health?
The gut microbiome generates metabolites (like SCFAs) and immune signals that support both gut and skin barrier integrity. Dysbiosis increases inflammation, contributing to skin conditions.
Q: What dietary habits damage barrier function?
Diets high in sugar, processed foods, and food allergens can increase inflammation, disrupt the gut microbiome, and reduce nutrient absorption, leading to compromised barrier function.
Q: Which interventions help restore barrier health?
Effective strategies include:
- Eating a diverse, fiber-rich diet
- Using probiotics and prebiotics
- Gentle, moisture-preserving skincare
- Reducing stress and getting adequate sleep
Q: Do antibiotics always damage barrier function?
Antibiotics can reduce microbial diversity in both the gut and skin, sometimes leading to flare-ups after a treatment course. However, when used precisely for infections, the risks are mitigated with proper microbiome support.
Q: Are some people genetically predisposed to barrier dysfunction?
Yes, mutations affecting barrier proteins like filaggrin (skin) or tight junctions (gut) increase the risk of conditions such as eczema and leaky gut.
Final Thoughts
Healthy skin and gut barriers underpin overall well-being. Their complex interplay means that dysfunction in one can echo throughout the body. By understanding and addressing the root causes—dysbiosis, inflammation, genetic factors, and lifestyle choices—we gain new pathways to restore resilience and reduce disease risk.
References
- https://vibrant-wellness.com/blog/gut-health-and-skin-disorders-addressing-the-root-cause-of-eczema-and-psoriasis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9654002/
- https://globalwellnessinstitute.org/global-wellness-institute-blog/2025/06/13/the-beauty-gut-connection-how-digestive-health-affects-skin-appearance/
- https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2024.1322205/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7916842/
- https://www.gutmicrobiotaforhealth.com/the-gut-skin-axis-feel-it-in-your-gut-wear-it-on-your-skin/
- https://thedermdigest.com/epithelia-under-attack-the-skin-gut-and-respiratory-barriers/
- https://www.nature.com/articles/s41385-022-00524-9
Read full bio of medha deb












