Butyrate Enemas for Localized Rectal Barrier Support: Mechanisms, Evidence, and Clinical Perspectives
A focused method using gut-derived fatty acids to strengthen mucosal integrity.
Colonic health relies heavily on the intricate interplay between the gut microbiota, intestinal epithelial cells, and metabolic byproducts. One molecular group at the center of this interplay is short-chain fatty acids (SCFAs), notably butyrate, a critical energy source for colonic epithelial cells and a powerful signaling molecule. Localized delivery of butyrate via enemas has been investigated as a tool to therapeutically support, repair, or enhance the rectal epithelial barrier, especially in disorders characterized by mucosal damage. This article reviews the science, evidence, and clinical considerations surrounding butyrate enemas for localized rectal barrier support.
- Table of Contents
- Introduction
- Mechanisms of Butyrate Action in Colonic Health
- Molecular Effects of Butyrate on the Rectal Barrier
- Clinical Evidence for Butyrate Enemas
- Indications and Clinical Uses
- Dosage and Administration
- Safety Considerations and Adverse Effects
- Reservations, Limitations, and Controversies
- Future Directions in Butyrate Research
- Frequently Asked Questions (FAQs)
- Key References
Table of Contents
- Introduction
- Mechanisms of Butyrate Action in Colonic Health
- Molecular Effects of Butyrate on the Rectal Barrier
- Clinical Evidence for Butyrate Enemas
- Indications and Clinical Uses
- Dosage and Administration
- Safety Considerations and Adverse Effects
- Reservations, Limitations, and Controversies
- Future Directions in Butyrate Research
- Frequently Asked Questions (FAQs)
- Key References
Introduction
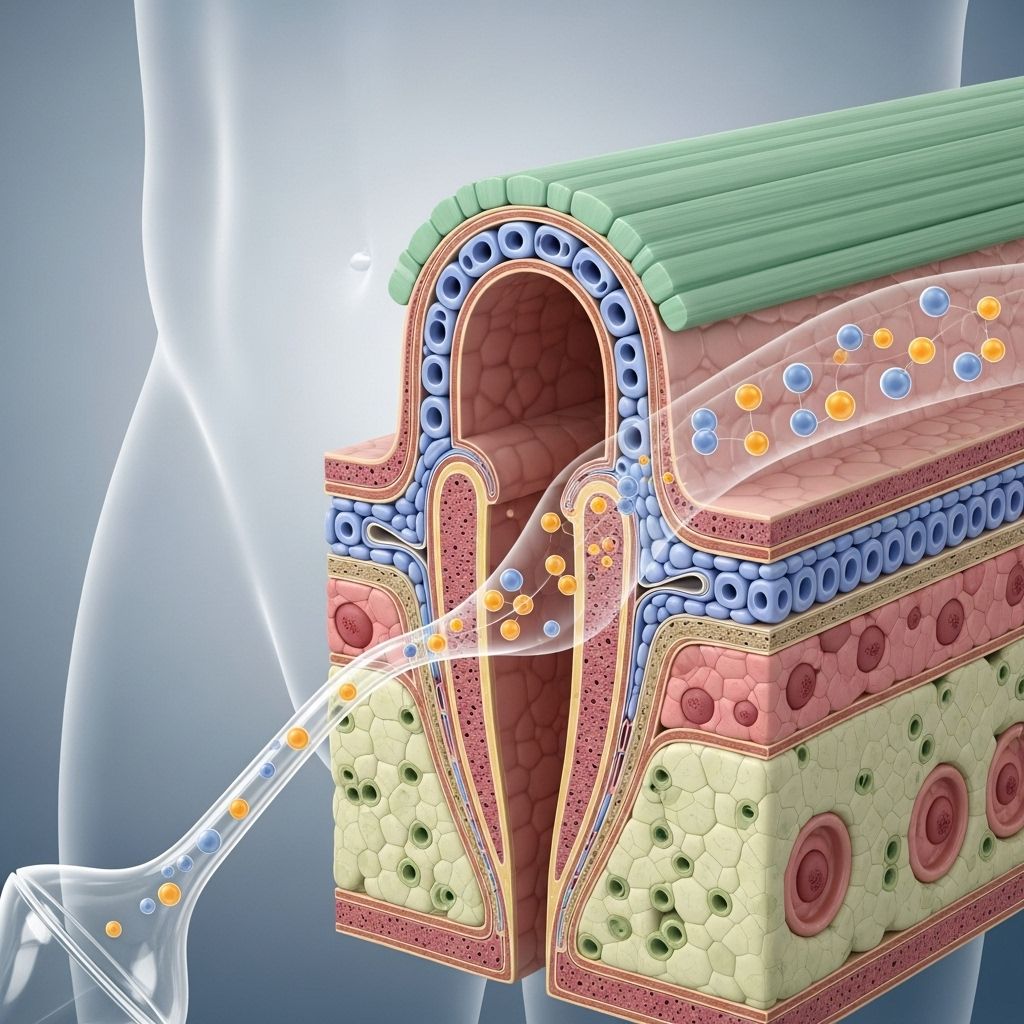
The colonic mucosal barrier is vital for maintaining gut health, regulating immune responses, and preventing translocation of pathogens and toxins. A well-functioning barrier depends, in part, on microbial fermentation of dietary fibers into SCFAs such as acetate, propionate, and butyrate. Among these, butyrate plays a particularly important role due to its effects on epithelial integrity, anti-inflammatory actions, and support for cellular energy metabolism.
When oral or dietary approaches to increasing butyrate production are inadequate, butyrate enemas offer a method for direct, localized delivery of this SCFA to the rectal and distal colonic mucosa. This approach has attracted interest for conditions characterized by epithelial damage or increased barrier permeability—such as ulcerative colitis, radiation proctitis, diversion colitis, and possibly irritable bowel syndrome (IBS) and pouchitis.
Mechanisms of Butyrate Action in Colonic Health
- Energy Source: Butyrate is the main energy substrate for colonocytes, supporting their function, regeneration, and barrier integrity.
- Epigenetic Regulation: It acts as a histone deacetylase (HDAC) inhibitor, modulating gene transcription to reduce inflammation and support barrier genes.
- Immune Modulation: Butyrate influences T-cell activation, decreases pro-inflammatory cytokine production, and supports immune tolerance.
- Barrier Enhancement: Key for tight junction protein expression (e.g., occludin, claudins), limiting paracellular permeability and pathogen invasion.
- Apoptosis/Cell Proliferation: Regulates cell turnover in the colonic mucosa, promoting homeostasis and recovery after injury.
- Antioxidant Activity: Upregulates genes in antioxidant pathways, limiting oxidative stress and further protecting the mucosa.
Molecular Effects of Butyrate on the Rectal Barrier
Systematic research has shown that butyrate enemas can induce profound molecular and cellular changes in the colonic mucosa. Major findings include:
- Gene Expression: Administration of butyrate enemas for two weeks upregulates hundreds of genes in the human colonic mucosa, especially those involved in fatty acid oxidation, electron transport, and oxidative stress pathways.
- Tight Junctions and Epithelial Integrity: Butyrate modulates gene networks associated with epithelial integrity and tight junction formation, promoting a less permeable, more robust mucosal barrier.
- Cellular Energy Metabolism: Butyrate boosts mitochondrial function by increasing transcription of enzymes involved in the TCA cycle and the respiratory chain, optimizing ATP production for barrier repair.
- Reduction of Immune Activation: Direct butyrate exposure suppresses pro-inflammatory signals, such as IL-12 production, which in turn modulates immune cell activation in the mucosa.
- Modulation of Cell Death and Turnover: Butyrate induces both proliferative and anti-apoptotic signals that are essential for epithelial repair and homeostasis after insult or injury.
Table: Selected Butyrate-Induced Effects Relevant to Rectal Barrier Support
| Effect | Molecular Basis | Resulting Benefit |
|---|---|---|
| Enhancement of tight junction proteins | Gene upregulation of occludin, claudin family | Reduced barrier permeability, improved defense |
| HDAC inhibition | Epigenetic modulation of inflammation-related genes | Suppressed pro-inflammatory gene expression |
| Increase of mitochondrial enzymes | Upregulation of TCA cycle, oxidative phosphorylation genes | Enhanced energy supply for mucosal repair |
| Promotion of cell proliferation & apoptosis regulation | Differential gene modulation in epithelial renewal pathways | Efficient turnover and healing of mucosal injuries |
Clinical Evidence for Butyrate Enemas
The translation of butyrate’s molecular promise into clinical benefit—especially using enemas to deliver high, controlled concentrations directly to the rectal mucosa—has been explored in both healthy individuals and patients with gastrointestinal disorders. The evidence base highlights several key points:
Key Findings in Healthy Subjects
- Visceral Sensitivity Reduction: In randomized controlled trials, physiologically relevant concentrations of butyrate delivered via enema have shown a dose-dependent reduction in rectal pain, urgency, and discomfort upon distension. At higher pressures, pain scores were reduced by over 40% compared to placebo, and discomfort was similarly diminished.
- Enhanced Barrier Function: Objective measures indicate improved mucosal resilience, as well as possible mitigation of minor subclinical mucosal irritation in the healthy gut.
Evidence in Inflammatory Bowel Disease (IBD)
- Ulcerative Colitis: A systematic review of eight controlled studies involving 227 patients showed that butyrate enemas may have positive effects on some inflammatory parameters in mucosal biopsies.
- Limitations: Placebo-controlled data show inconsistent results, with only one study reporting significant differences in the disease activity index. Butyrate enemas generally had minimal effect on endoscopic or histological remission compared to placebo.
- Safety: No major safety concerns have been consistently reported, but patient tolerance and acceptability can vary.
- Crohn’s Disease: Clinical data are minimal and inconclusive regarding the efficacy of butyrate enemas.
Other Indications
- Radiation Proctitis & Diversion Colitis: Some case series and small trials suggest possible benefits, but large-scale evidence is lacking.
- Butyrate enemas are also being explored for functional bowel disorders and other forms of mucosal injury, although with less robust evidence.
Indications and Clinical Uses
Butyrate enemas are best suited for conditions involving localized mucosal damage or compromised epithelial barrier function in the rectum or distal colon. Commonly investigated or considered indications include:
- Ulcerative colitis (especially distal/left-sided disease)
- Diversion colitis (in patients with a non-functioning colonic segment)
- Radiation proctitis
- Pouchitis (inflammatory episodes in ileal pouches)
- Subclinical barrier dysfunction (being researched)
As research advances, the spectrum of uses may expand, particularly as formulation and delivery methods improve.
Dosage and Administration
- Dose: Clinical studies most commonly use enemas containing 50 to 100 mmol/L sodium butyrate, with volumes ranging from 60 to 100 ml per enema.
- Frequency: Typically, enemas are administered once daily—often in the evening before bedtime—for periods ranging from 1 to 4 weeks in clinical studies.
- Retention: For maximal effect, patients are encouraged to retain the solution for at least 30 minutes, although tolerance varies.
- Formulation: Butyrate may be delivered as sodium butyrate, or as ready-to-use compounded enema solutions prepared in a sterile setting.
Practical considerations include patient instruction on enema self-administration, maintaining privacy and comfort, and monitoring for local irritation or intolerance.
Safety Considerations and Adverse Effects
- Most clinical studies report excellent local and systemic safety, with no serious adverse events related to butyrate enemas.
- Common minor effects: transient rectal irritation, minor burning or cramping, urgency, and rarely, mild allergic reactions.
- Butyrate enemas are considered unlikely to cause systemic effects due to poor systemic absorption from the rectum.
- In patients with anal fissures, proctitis, or severe mucosal friability, caution and supervision are advised.
Reservations, Limitations, and Controversies
- Inconsistent Clinical Efficacy: Placebo-controlled trials, especially in ulcerative colitis, show mixed results with some reporting improvement in inflammation and others reporting negligible differences.
- Possible Publication Bias: Many early studies are small and positive, while larger studies show less robust effects.
- Subjective Outcomes: Some benefits (pain/urgency reduction) are more recognizable in healthy volunteers than in patients with active inflammation.
- Lack of Long-term Data: Few studies extend beyond four weeks of therapy, leaving long-term safety and efficacy unclear.
- Limited Data in Pediatric and Elderly Populations: Most research is in adult populations.
Future Directions in Butyrate Research
Ongoing and future research seeks to address several challenges and opportunities:
- Optimizing butyrate formulations for improved retention, palatability, and mucosal absorption.
- Identifying biomarkers predicting response to butyrate therapy.
- Comparing butyrate enemas to oral or dietary interventions aimed at boosting endogenous SCFA production.
- Exploring synergy with probiotics, prebiotics, or other anti-inflammatory agents.
- Clarifying butyrate’s role in preventing colorectal cancer or enhancing repair in post-surgical settings.
Understanding patient subgroups most likely to benefit from localized butyrate delivery remains an active area of research.
Frequently Asked Questions (FAQs)
Q1: What is butyrate?
Butyrate is a short-chain fatty acid produced by bacterial fermentation of dietary fiber in the colon. It provides energy for colonocytes and has numerous anti-inflammatory and barrier-enhancing effects.
Q2: How do butyrate enemes differ from oral butyrate or dietary fiber?
Butyrate enemas deliver concentrated butyrate directly to the rectal and distal colonic mucosa, bypassing the need for microbial fermentation. Oral butyrate (or increased fiber intake) generates SCFAs throughout the colonic lumen but may not achieve the same localized mucosal concentrations.
Q3: Are butyrate enemas safe to use?
Available evidence supports their safety when administered as described in clinical studies. Minor local irritation may occur, but serious adverse effects are rare.
Q4: Can butyrate enemas cure ulcerative colitis or other IBD forms?
Current clinical data do not support butyrate enemas as a stand-alone cure for IBD, although they may help support mucosal barrier function and reduce some symptoms in specific settings.
Q5: How quickly do patients feel the benefit?
Benefits such as reduced pain, urgency, or discomfort have been reported within 1 to 2 weeks in some studies. Mucosal healing may take longer and remains less predictable.
Key References
- Vanhoutvin SALW, et al. “Butyrate-Induced Transcriptional Changes in Human Colonic Mucosa.” PLOS ONE, 2009.
- A systematic review: Effect of Sodium Butyrate Enemas on IBD. Current Medical Research, 2022.
- Vanhoutvin SALW, et al. “The Effects of Butyrate Enemas on Visceral Perception in Healthy Volunteers.” Neurogastroenterol Motil, 2009.
- Review: The Role of Short Chain Fatty Acids in IBS. J Neurogastroenterol Motil, 2021.
References
Read full bio of Sneha Tete












