Blue Light Exposure and Its Impact on Dermal Capillary Function: Comprehensive Analysis of Cellular, Molecular, and Clinical Effects
High-energy visible rays may silently undermine skin healing and long-term resilience.
Blue Light Exposure & Dermal Capillary Function Analysis
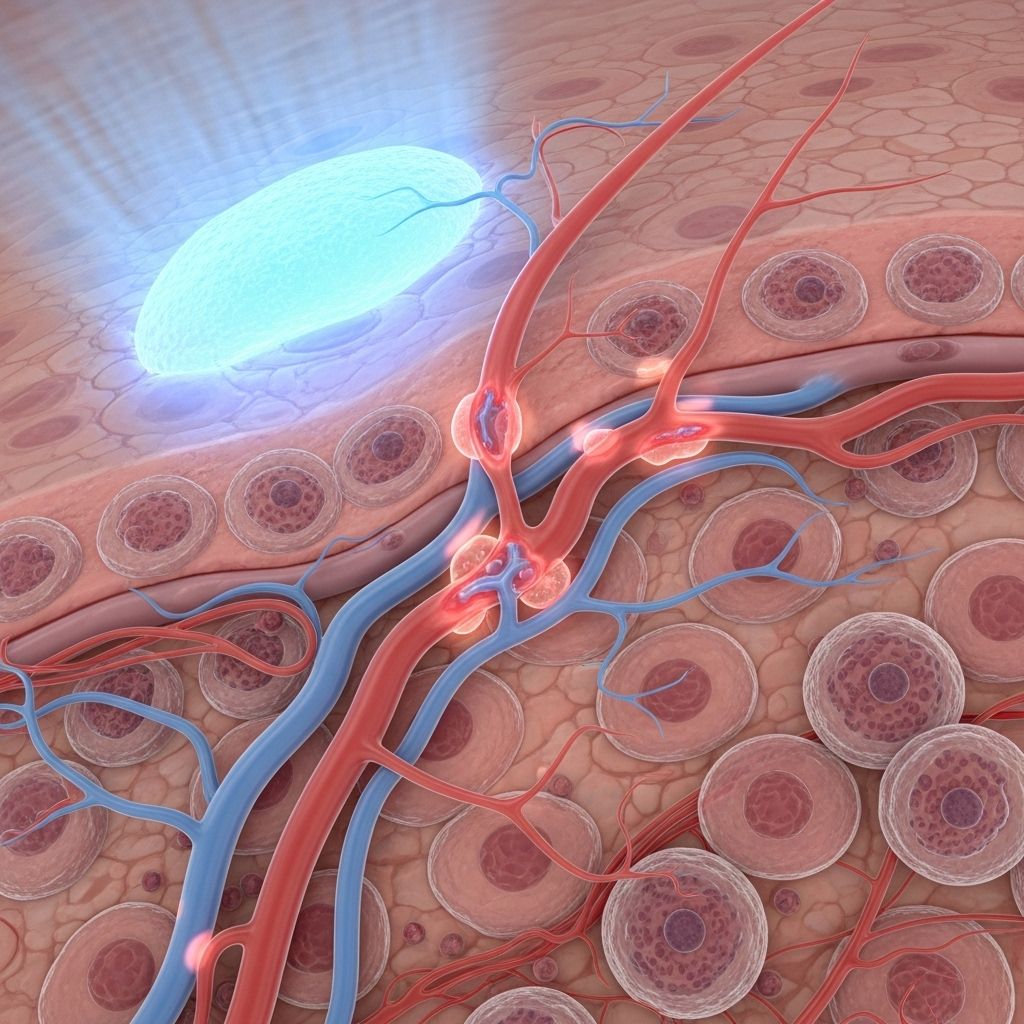
Modern lifestyles have dramatically increased human exposure to blue light through screens, artificial lighting, and medical applications. While the effects of ultraviolet (UV) radiation on skin health are well established, growing research implicates blue light as a significant modulator of skin physiology, particularly in dermal capillary function and microvascular health. This article provides an extensive analysis of how blue light interacts with the dermal capillary system, detailing cellular mechanisms, microvascular responses, clinical outcomes, and future research directions.
Table of Contents
- Introduction: Blue Light and Skin Health
- Blue Light in Skin Biology: Definition and Sources
- Dermal Capillary Structure and Function
- Mechanisms of Blue Light Interaction with Skin Cells
- Effects of Blue Light on Dermal Capillary and Microvasculature
- Molecular Pathways: ROS, Mitochondrial Dysfunction, and Inflammatory Signaling
- Skin Barrier Integrity, Photoaging, and Capillary Health
- Potential Clinical and Therapeutic Implications
- Frequently Asked Questions (FAQs)
- Conclusion and Future Directions
Introduction: Blue Light and Skin Health
The increase in environmental and artificial sources of visible blue light (wavelengths 400–490 nm) has prompted concerns regarding its impact on skin physiology and microvascular stability. Unlike UV, blue light penetrates to the dermis and acts on various resident cells, including keratinocytes and dermal fibroblasts. Recent evidence suggests blue light exposure affects not just the superficial layers of the skin but also alters the function and structure of dermal capillaries, with possible long-term consequences for skin health, wound healing, and aging.
Blue Light in Skin Biology: Definition and Sources
Blue light refers to electromagnetic radiation in the 400–490 nm wavelength range, making it part of the visible spectrum between ultraviolet (UV) and green light. It is ubiquitous in daily life from sources such as:
- Natural sunlight (a significant portion of visible light)
- LED screens (smartphones, tablets, laptops, TVs)
- Fluorescent and LED lighting
- Medical and cosmetic devices (used in phototherapy and photodynamic therapy)
Given its prevalence, understanding blue light’s biological actions on the skin—particularly at the microvascular level—is essential for formulating preventive and therapeutic measures.
Dermal Capillary Structure and Function
Dermal capillaries constitute a crucial network within the papillary and reticular dermis. Their main roles include:
- Supplying oxygen and nutrients to skin cells
- Regulating local temperature and fluid balance
- Supporting immune surveillance by facilitating leukocyte migration
- Participating in wound healing and angiogenesis
These capillaries are lined by endothelial cells, surrounded by pericytes and embedded in a matrix rich in collagen, elastin, and glycosaminoglycans. Capillary function is tightly regulated by local mediators, growth factors (such as VEGF-A, FGF-2), and signaling cascades—a balance which can be perturbed by external stressors, including blue light exposure.
Mechanisms of Blue Light Interaction with Skin Cells
Upon skin exposure, blue light induces photochemical responses in cutaneous cells, notably keratinocytes and fibroblasts. Critical mechanisms include:
- Photoactivation of Chromophores: Flavins, porphyrins, and other photoacceptor molecules absorb blue photons, initiating downstream cellular events.
- Production of Reactive Oxygen Species (ROS): Blue light triggers photooxidation reactions in chromophores, generating free radicals and hydrogen peroxide, which induce oxidative stress in cells.
- Mitochondrial Dysfunction: Blue light damages mitochondrial DNA (mtDNA) and impairs respiration, reducing ATP production and increasing oxidative stress.
- Modulation of Signaling Pathways: Exposure alters expression of genes related to proliferation, differentiation, and inflammation, including the p-STAT3-VEGF-A/FGF-2/Mcp-1 axis, central in capillary and skin homeostasis.
These cellular perturbations disrupt tissue repair and microvascular stability, with visible and latent consequences for skin health.
Effects of Blue Light on Dermal Capillary and Microvasculature
Blue light affects dermal capillary function through multiple, often dose-dependent, biological pathways:
- Reduced Cell Viability and Proliferation: Blue light diminishes fibroblast and keratinocyte viability, impeding the renewal of cells vital for vessel repair and maintenance.
- Capillary Permeability and Vascular Tone: Excessive ROS can disrupt endothelial integrity, increasing capillary permeability and risk of edema or local inflammation.
- Altered Angiogenic Factor Production: Blue light inhibits growth factors essential for angiogenesis, such as VEGF-A and FGF-2.
- Impaired Wound Healing: Disrupted microcirculation delays tissue oxygenation and nutrient delivery, resulting in suboptimal healing and increased risk for scarring.
- Immune Microenvironment Alteration: Modulation of chemokines (e.g., Mcp-1) can influence leukocyte recruitment and immune responses at the capillary level.
| Effect | Contribution to Capillary Dysfunction | Evidence |
|---|---|---|
| Reduced Cell Viability/Proliferation | Impaired capillary repair, slow vessel regeneration | |
| ROS Production | Oxidative damage to endothelium, increased permeability | |
| Downregulation of Angiogenic Factors | Reduced vessel growth and maintenance | |
| Altered Immune Signaling | Disrupted leukocyte transmigration, chronic inflammation | |
| Mitochondrial Dysfunction | Reduced ATP, impaired cellular metabolism |
Molecular Pathways: ROS, Mitochondrial Dysfunction, and Inflammatory Signaling
At the molecular level, blue light exposure disrupts fundamental pathways central to capillary health:
- CYP450-Dependent Mitochondrial Pathways: Blue light activates mitochondrial cytochromes (Cyp1b1, Cyp1a1), leading to increased ROS production. Inhibiting these enzymes reduces ROS accumulation.
- p-STAT3-VEGF-A/FGF-2/Mcp-1 Axis: Blue light exposure inhibits the activation of this axis, as opposed to red light that enhances it. Downregulation of VEGF-A and FGF-2 reduces new capillary formation, impairing skin healing and microvascular function.
- Mitochondrial DNA damage: Dose-dependent mtDNA strand breaks and dysfunction in oxygen consumption rate (OCR) are observed in human dermal fibroblasts after blue light exposure. This leads to decreased ATP synthesis and increased apoptosis or necrosis in skin cells.
- Inflammatory Cascade Activation: Blue light-induced oxidative stress upregulates matrix metalloproteinases (MMPs), chemokines, and inflammatory cytokines, impacting capillary permeability and endothelial health.
Skin Barrier Integrity, Photoaging, and Capillary Health
Beyond immediate capillary responses, blue light exposure contributes to broader skin barrier and aging processes:
- Photoaging: Mechanistic studies link blue light–induced ROS production to increased skin cell senescence, collagen degradation, and elastosis, all of which reduce dermal elasticity and compromise the capillary bed.
- Barrier Breakdown: Oxidative stress weakens tight junctions and the extracellular matrix, increasing trans-epidermal water loss and facilitating entry of irritants, which in turn can provoke microvascular inflammation.
- Delayed Wound Healing and Scar Formation: Research shows that scar models subjected to blue light display slow healing and chronic inflammation, unlike those treated with red light, which promotes angiogenesis and scar reduction.
- Potential Risk for Vascular Skin Disorders: Chronic alteration of dermal capillary responses may predispose to disorders like telangiectasia or exacerbate inflammatory dermatoses.
Potential Clinical and Therapeutic Implications
The dual nature of blue light—being both a risk factor and a selective therapeutic agent—has important ramifications:
- Positive Applications:
- Blue light (particularly in specific windows and controlled doses) demonstrates antibacterial properties and shows clinical promise for treating superficial infections or targeted hyperproliferative lesions.
- It can modulate fibroblast proliferation in conditions prone to fibrotic scarring with tailored protocols.
- Negative Outcomes:
- Unshielded, repeated, or high-dose blue light exposure may accelerate dermal aging, impair wound healing, and compromise capillary structure and function.
- Particularly relevant in individuals with high environmental or occupational exposure.
- Protective Strategies:
- Development of topical antioxidants to scavenge blue light–induced ROS.
- Barrier creams with blue light–blocking pigments or minerals (e.g., iron oxides, titanium dioxide).
- Behavioral modifications such as screen filters and reduced exposure duration.
- Research Gaps: There is ongoing need for studies assessing the chronic effects of real-world blue light exposures on capillary structure and repair, and the efficacy of countermeasures.
Frequently Asked Questions (FAQs)
Q: How does blue light generate reactive oxygen species in the skin?
A: Blue light stimulates mitochondrial photoacceptors and flavoproteins in skin cells, leading to an electron leakage that generates superoxide and hydrogen peroxide, rapidly converting to other ROS that damage DNA, proteins, and lipids.
Q: What are the visible signs of blue light–induced microvascular dysfunction?
A: Over time, chronic blue light exposure may manifest as delayed wound healing, increased skin fragility, fine telangiectasia (visible capillaries), and exacerbated redness or edema due to increased capillary permeability.
Q: Is blue light as dangerous as UV for the skin?
A: Blue light does not cause the same acute DNA mutations as UV, but it induces oxidative stress, inflammation, and cellular dysfunction, particularly at the mitochondrial level, leading to premature aging and impaired microvascular repair.
Q: Can blue light have positive therapeutic effects on dermal conditions?
A: Yes, when applied in controlled doses and contexts, blue light can inhibit unwanted fibroblast proliferation (helpful in scarring disorders) and has antimicrobial effects. The clinical benefit depends on precise dosing and indication.
Q: How can one protect their skin’s microvasculature from excessive blue light?
A: Use broad-spectrum sunscreens with iron oxides, apply topical antioxidants, limit digital device time, and consider physical screen protectors that filter high-energy visible light.
Conclusion and Future Directions
As artificial blue light exposure steadily rises, awareness of its effects on dermal microvasculature—capillary integrity, healing, and homeostasis—becomes increasingly vital. Evidence highlights blue light’s propensity to induce oxidative stress, interfere with key vascular growth factors, and impede healing, while also holding therapeutic promise when harnessed judiciously. Future research should elucidate safe exposure thresholds, effective protective strategies, and long-term clinical outcomes in diverse populations. Integrating molecular, cellular, and clinical data will optimize strategies for promoting skin health in a blue light–saturated world.
References
- https://www.nature.com/articles/s42003-024-06973-1
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12107506/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9965217/
- https://thedermdigest.com/blues-clues-research-explores-how-blue-light-affects-skin/
- https://dermatologyseattle.com/blue-light-and-your-skin/
- https://impact.africacdc.org/sites/default/files/public_files/2025-10/EagleEyeX20variation-rbAGeqH.pdf
- https://ouci.dntb.gov.ua/en/works/7WwQR257/
- https://www.dovepress.com/dosimetry-assessment-of-potential-hazard-from-visible-light-especially-peer-reviewed-fulltext-article-CCID
Read full bio of Sneha Tete












