Blood Thinners & Skin Health: Weighing Benefits, Risks, and Dermatological Impact
Careful monitoring and tailored treatment ensure safe healing and reduced complications.
Blood Thinners & Skin Health: Benefits and Drawbacks
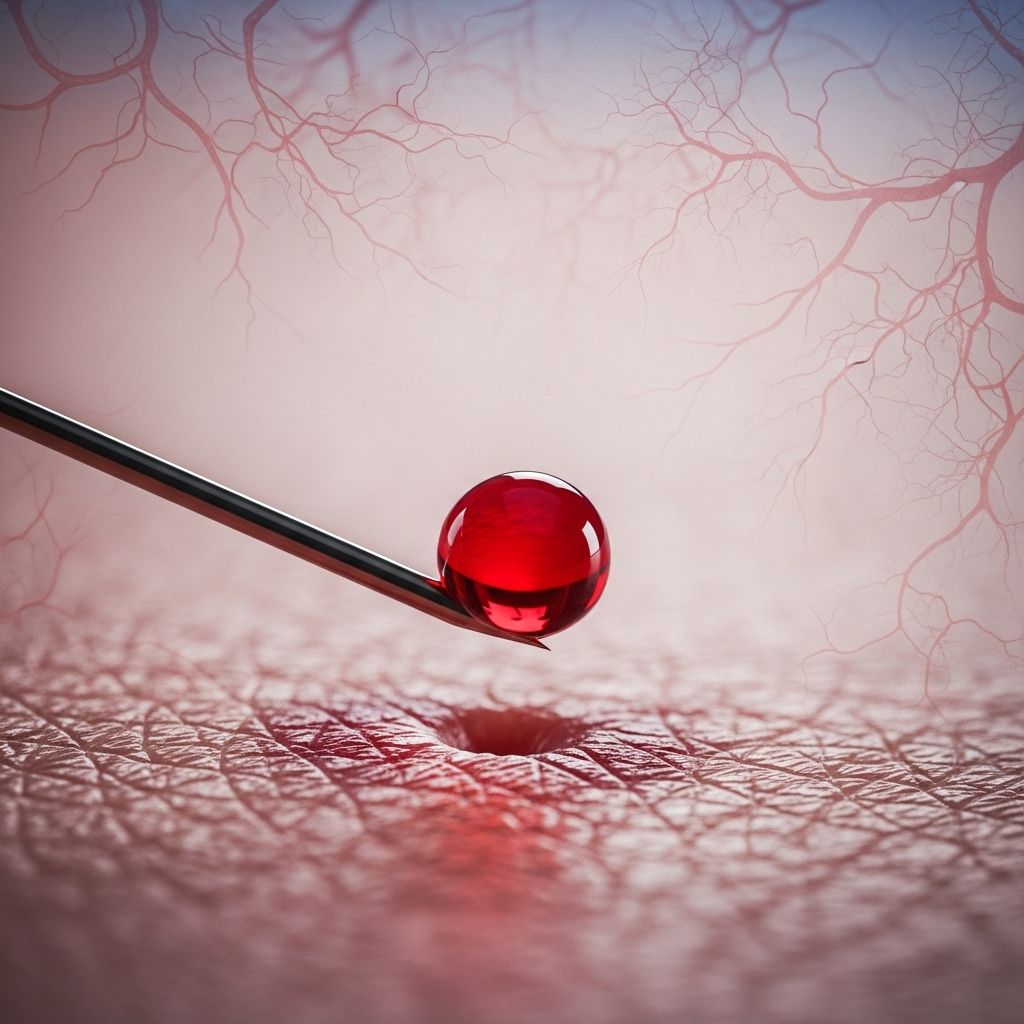
Blood thinners, also known as anticoagulants, are essential medications for preventing and treating dangerous blood clots. Their use has dramatically reduced the incidence of life-threatening conditions such as strokes, heart attacks, and deep vein thrombosis. Yet, their action on blood coagulation has profound implications for skin health — influencing wound healing, susceptibility to bruising, and, in rare cases, leading to skin necrosis or drug-induced rashes. This article explores the complex relationship between blood thinners and skin, offering an in-depth review for patients, clinicians, and caregivers.
Table of Contents
- Introduction to Blood Thinners and Skin Health
- Types of Blood Thinners
- How Anticoagulants Interact with Skin
- Benefits for Skin Health
- Drawbacks and Adverse Skin Reactions
- Risk Factors for Cutaneous Complications
- Patients with Pre-Existing Skin Conditions
- Monitoring and Managing Skin Side Effects
- Balancing Benefits and Risks
- Frequently Asked Questions (FAQs)
- Key Takeaways
Introduction to Blood Thinners and Skin Health
Blood thinners (anticoagulants and antiplatelets) are widely used to manage conditions where unwanted blood clots threaten patient health, especially cardiovascular and thromboembolic disorders. These medications work by interrupting different stages in the body’s clotting process. While effective at preventing clots, their effects extend to blood vessels within the skin and influence healing, trauma response, and even immune reactions.
Types of Blood Thinners
Blood thinners fall into two main categories, each with different mechanisms:
- Anticoagulants: These interfere with the action of clotting factors. Examples include warfarin, heparin, apixaban (Eliquis), dabigatran, and rivaroxaban.
- Antiplatelet agents: These stop platelets from clumping together. Examples are aspirin and clopidogrel.
Anticoagulants (like warfarin and heparin) are more strongly associated with unique skin reactions due to their deeper interaction with the coagulation cascade.
How Anticoagulants Interact with Skin
The skin is a highly vascular organ, relying on an intricate network of blood vessels to supply nutrients, remove wastes, and heal injuries. Blood thinners slow clot formation, which means:
- Broken blood vessels under the skin (from trauma, friction, or other causes) leak blood for longer.
- Delayed clotting can slow wound closure and healing, especially after surgery or injury.
- The immune and inflammatory response in the skin may be altered, influencing rashes and hypersensitivity reactions.
Benefits for Skin Health
While the main benefits of blood thinners are in preventing major cardiovascular events, they can yield direct and indirect benefits for skin health:
- Prevention of thrombosis-related skin disorders: By minimizing the risk of blood clots, blood thinners help prevent pain, swelling, and skin discoloration (such as livedo reticularis or venous stasis changes) that may arise from poor venous drainage.
- Avoidance of tissue ischemia: Clots that block blood supply to areas of the skin can cause ischemia (lack of oxygen), which would otherwise lead to ulcers or necrosis.
- Cosmetic and reconstructive procedures: Proper anticoagulation can support healthy healing after skin grafts and cosmetic procedures in select patients (with careful consideration of bleeding risk).
However, these benefits frequently depend upon correct dosing and vigilant monitoring to avoid adverse reactions.
Drawbacks and Adverse Skin Reactions
Blood thinners are associated with several skin-specific side effects, ranging from common and minor to rare but serious:
Bruising
- Easy Bruising: Blood thinners hinder the body’s ability to form clots quickly after trauma, so even minor skin bumps can cause visible bruising.
- Worse Bruises: Capillaries under the skin may leak blood for longer, resulting in larger, more intense discoloration with slower resolution.
Delayed Wound Healing
- Chronic Wounds: Elderly or medically complex patients may find wounds or skin tears heal more slowly and are more prone to bleeding.
- Excessive Bleeding: Even small cuts may require more time and attention to control bleeding and reduce infection risk.
Skin Necrosis
- Warfarin-Induced Skin Necrosis: A rare but severe condition where paradoxical blood clotting blocks vessels and leads to tissue death — often in areas with high fat content, such as thighs, abdomen, or breasts.
- Heparin-Induced Skin Necrosis: Similar complications have been described with heparin use.
Necrosis is life-threatening and requires immediate clinical attention.
Drug-Induced Rashes and Hypersensitivity
- Hypersensitivity Rashes: Direct oral anticoagulants like apixaban can cause pruritic erythematous rashes, sometimes exacerbated in patients with pre-existing skin diseases.
- Maculopapular, Purpuric, or Vesicular Lesions: A range of eruptions have been attributed to anticoagulants, usually requiring withdrawal of the offending drug.
Risk Factors for Cutaneous Complications
Some individuals are more likely to experience skin-related adverse effects:
- Age: Older adults have thinner, less elastic skin and may bruise or heal less efficiently.
- Comorbidities: Conditions like diabetes, renal impairment, or vascular disorders heighten risk.
- Pre-existing skin diseases: Autoimmune conditions (e.g., pemphigus, eczema) may worsen with blood thinners, especially those prone to rashes.
- High initial doses or rapid loading: Especially with warfarin — this increases the chance of necrosis.
- Absence of concurrent heparin therapy: Starting warfarin without bridging heparin can trigger paradoxical clotting and necrosis.
Blood Thinners in Patients with Pre-Existing Skin Conditions
Careful assessment is critical in patients with chronic skin diseases requiring anticoagulation:
- Autoimmune conditions: People with disorders like pemphigus vulgaris may experience drug-triggered flares or more severe hypersensitivity reactions.
- Chronic wounds or ulcers: Management must balance the risk of excessive bleeding with the importance of preventing clot-driven ischemia that impedes healing.
- Inflammatory skin diseases: Blood thinners may sometimes alter the severity or course of these conditions, though data is limited.
Modification of therapy or drug choice may be necessary if adverse reactions are problematic.
Monitoring and Managing Skin Side Effects
Proactive monitoring and management are vital for safe anticoagulation and optimal skin health. Key steps include:
- Regular dermatological checks: Periodic assessments for rashes, bruising, and wound complications.
- Prompt attention to skin changes: Any new lesions, severe bruising, or slow healing should be discussed with a clinician.
- Patient education: Inform patients about expected changes in skin appearance and what warrants medical review.
- Adjusting therapy: Dose adjustments or switching anticoagulant types may be needed for significant skin reactions.
- Supportive care: For rashes and wounds, topical medications, wound care, and infection prevention may be necessary.
Most minor skin issues are manageable, but prompt recognition of severe complications is crucial.
Balancing Benefits and Risks
Deciding on optimal anticoagulant therapy involves weighing the life-saving benefits against the risk of skin complications. This decision should factor in:
- The underlying medical indication for blood thinners
- Patient age, skin condition, and overall health
- Previous history of skin reactions to similar drugs
- The capacity for close monitoring and quick response to side effects
For many, the prevention of strokes, heart attacks, or pulmonary embolism far outweighs the inconvenience of mild bruising or slowed healing. Nonetheless, all severe or unusual reactions demand medical evaluation.
Frequently Asked Questions (FAQs)
Q: Why do blood thinners cause more bruising?
A: By slowing clot formation, blood thinners allow more blood to seep from injured capillaries under the skin, resulting in larger, darker bruises that take longer to fade.
Q: Can blood thinners delay wound healing?
A: Yes. Patients may notice wounds bleeding longer and healing more slowly, especially the elderly or those with chronic illness.
Q: What is skin necrosis, and how common is it?
A: Skin necrosis is the death of tissue due to blocked blood supply. It is a rare but serious complication, most often associated with warfarin, typically occurring within days of starting therapy or due to specific patient factors.
Q: What should I do if I develop a skin rash while on blood thinners?
A: Notify your healthcare provider promptly. Some rashes may signal allergic reactions requiring medication changes; early intervention leads to better outcomes.
Q: Are all blood thinners equally likely to cause skin issues?
A: Some, like warfarin and heparin, have a higher association with severe skin complications like necrosis, while newer agents (direct oral anticoagulants) may be more linked to hypersensitivity rashes.
Key Takeaways
- Blood thinners are essential for preventing life-threatening blood clots but can alter skin health in significant ways.
- Most individuals experience manageable side effects like bruising and slower wound healing; rare but serious complications include skin necrosis and drug-induced rashes.
- Proper monitoring, patient education, and prompt response to adverse reactions are key to balancing therapy benefits with dermatological risk.
- Clinicians should always weigh individual risk factors, especially in those with chronic wounds or pre-existing skin diseases.
References
- https://jamanetwork.com/journals/jamadermatology/fullarticle/530689
- https://oncallwoundcare.com/how-anticoagulants-can-affect-the-healing-of-your-wounds/
- https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/ask-the-experts/bruises-from-blood-thinners
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10775822/
- https://dermnetnz.org/topics/warfarin-induced-skin-necrosis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4319805/
- https://www.nhs.uk/medicines/anticoagulants/side-effects/
- https://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/in-depth/warfarin-side-effects/art-20047592
- https://www.stoptheclot.org/living-your-best-life-while-taking-blood-thinners/
Read full bio of Sneha Tete












