Biofeedback Therapy for Fecal Incontinence: Clinical Principles, Efficacy, and Future Prospects
Structured feedback training rebuilds sphincter strength and restores confidence in life.
Fecal incontinence (FI), the involuntary loss of stool, affects millions of individuals worldwide, impacting both quality of life and psychological well-being. Biofeedback therapy has emerged as a central non-surgical treatment for managing this condition, offering structured retraining of pelvic floor and anal sphincter muscles using real-time physiological feedback and operant conditioning principles. This article presents an in-depth overview of biofeedback’s therapeutic use for fecal incontinence, including evidence-based techniques, clinical efficacy, patient selection, protocol variations, integration with other therapies, and perspectives on future development.
Table of Contents
- Introduction to Biofeedback Therapy
- Understanding Fecal Incontinence: Etiology and Impact
- Principles and Mechanisms of Biofeedback Therapy
- Core Clinical Protocols in Biofeedback for Fecal Incontinence
- Patient Selection and Assessment
- Clinical Evidence and Efficacy
- Comparison with Other Therapies
- Limitations, Challenges, and Future Directions
- Frequently Asked Questions (FAQs)
Introduction to Biofeedback Therapy
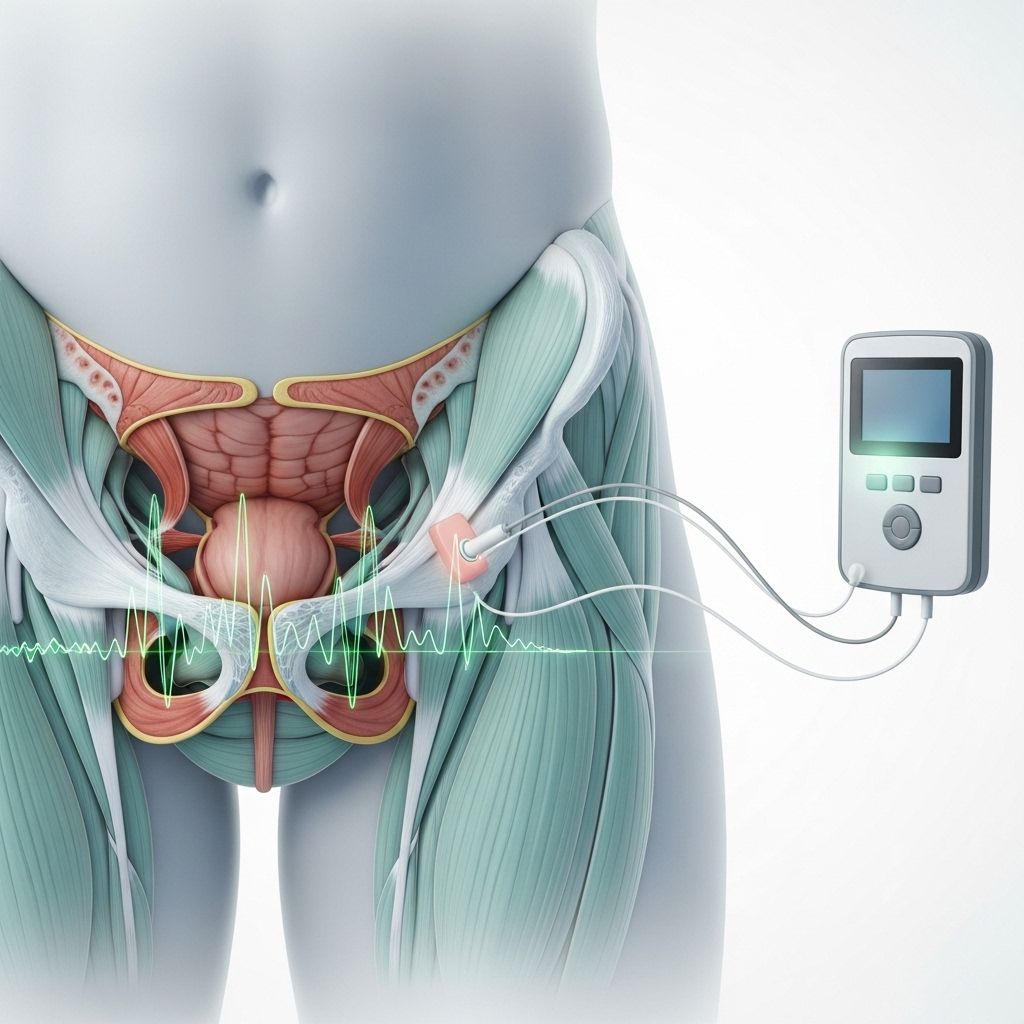
Biofeedback therapy for fecal incontinence employs instrumental monitoring to help patients gain voluntary control over specific pelvic floor and anal sphincter functions. It leverages instant, objective feedback to train users to optimize contraction, relaxation, and coordination, thereby addressing the neuromuscular deficits underlying many forms of FI.
- Principally targets muscle retraining, sensory awareness, and coordination.
- Delivered through devices offering real-time visual, auditory, or tactile cues.
- Combines patient education, counseling, and rigorous practice over multiple sessions.
- Safe, non-invasive, and shown to have durable effects for selected populations.
Understanding Fecal Incontinence: Etiology and Impact
To appreciate biofeedback’s therapeutic value, it is essential to understand the multifactorial nature of fecal incontinence:
- Neuromuscular damage (e.g., from obstetric trauma or nerve injury)
- Sphincter or pelvic floor weakness
- Rectal sensory dysfunction (hyposensitivity or hypersensitivity)
- Colorectal diseases or post-surgical states
- Functional defecation disorders, including dyssynergic defecation
Fecal incontinence leads to substantial psychological distress, reduced mobility, workplace challenges, and social isolation for affected individuals, affecting both older adults and younger patients with acquired or congenital defects.
Principles and Mechanisms of Biofeedback Therapy
Biofeedback therapy is grounded in the concepts of operant conditioning and neuroplasticity:
- Utilizes instrumentation (e.g., EMG, manometry, pressure sensors) to provide immediate feedback about muscle activity or physiologic responses.
- Feedback modalities enable the patient to recognize their efforts and adjust performance accordingly.
- This results in strengthening or re-educating the involved neuromuscular units, improving reflexive control, and refining sensory discrimination.
| Biofeedback Component | Mechanism | Impact on FI |
|---|---|---|
| Muscle strengthening | Reinforces voluntary sphincter and pelvic floor contractions | Improves continence and pressure control |
| Sensory training | Guides recognition of rectal filling and urge | Prevents accidents by increasing awareness and timely response |
| Coordination training | Synchronizes abdominal and pelvic floor action during defecation | Restores normal evacuation and continence reflexes |
Instrumentation Commonly Used in Biofeedback
- Electromyography (EMG): External or intrarectal sensors track muscle activity.
- Anorectal manometry: Measures pressures within the rectum and anal canal.
- Pressure balloons: Enable rectal sensory threshold and capacity assessments.
Core Clinical Protocols in Biofeedback for Fecal Incontinence
Biofeedback programs are customized for each patient’s underlying deficits but generally include three main components:
1. Strength Training
- Focuses on maximizing anal sphincter strength and improving timing and duration of voluntary contractions.
- Patients contract the external anal sphincter while receiving feedback about performance, promoting isolation and control of the correct muscle groups.
- Repeated exercises emphasize both maximal effort and sustained holds, with relaxation of abdominal muscles to avoid compensatory patterns.
2. Rectal Sensory Training
- Aims to normalize rectal sensation thresholds through graded balloon distension.
- Treats both hyposensitivity (failure to sense rectal filling) and hypersensitivity (urgency at low volumes).
- Patients learn to discriminate filling at smaller/greater volumes, improving timely initiation of sphincter contractions.
3. Coordination (Response) Training
- Enhances the voluntary anal contraction in response to rectal filling, reinforcing counteraction of involuntary relaxation reflexes.
- Focus on synchronization and sustained contraction during simulated challenges, such as rectal balloon inflation.
Additional Biofeedback Elements
- Education on anatomy, defecation mechanisms, and lifestyle adaptation.
- Guided behavioral training, including urge suppression and timed toileting.
- Occasional inclusion of diaphragmatic breathing or abdominal wall training.
Patient Selection and Assessment
Biofeedback is not uniformly effective for all patients with fecal incontinence. Careful selection increases the likelihood of benefit:
- Ideal for motivated patients who can participate in repeated sessions and follow instructions.
- Especially useful in those with functional sphincter or coordination deficits and intact cognitive abilities.
- Lesser benefit in patients with complete anatomic sphincter disruption or severe neurological impairment.
Comprehensive assessment includes:
- Detailed incontinence history and symptom scoring.
- Anorectal manometry and EMG studies to classify dysfunction.
- Assessment of psychological and social factors affecting prognosis.
Clinical Evidence and Efficacy
Multiple studies and reviews support biofeedback’s efficacy for FI in appropriately selected individuals:
- Reported response rates in randomized controlled trials range from 70% to over 90% for improvement in symptoms with biofeedback therapy.
- Improvement includes both a reduction in leakage episodes and enhanced voluntary bowel control.
- Durable benefits are often sustained well beyond active treatment, especially when reinforced by ongoing home exercises.
- Clinical outcomes are measured by reductions in accident episodes, improvements in validated symptom scores, and patient quality of life indices.
- Combined therapy (biofeedback with medication such as loperamide) may further reduce stool leakage and increase continent days per week in certain patients.
However, some studies note no statistically significant difference between biofeedback and standard pelvic floor muscle exercises or patient education for some populations, highlighting the need for further standardization and patient-specific adaptation.
Comparison with Other Therapies
| Therapy | Description | Advantages | Limitations |
|---|---|---|---|
| Biofeedback | Structured neuromuscular retraining using feedback | Safe; non-invasive; patient-specific; durable effects | Requires sustained participation; not effective for severe anatomic injury |
| Medical management | Antidiarrheal/bulking agents; lifestyle changes | Accessible; can address mild symptoms | Limited for severe FI; no direct muscle re-education |
| Sphincteroplasty (surgery) | Reconstruction of the damaged anal sphincter | Potentially curative in select cases | Surgical risks; not suitable for all patients; possible recurrence |
Limitations, Challenges, and Future Directions
Despite clear benefits for selected patients, biofeedback therapy faces several limitations:
- Heterogeneous patient response linked to varied pathophysiological mechanisms.
- Lack of universal standardization in protocol—types of feedback, number, and length of sessions vary across centers.
- Limited access in some regions due to need for trained therapists and equipment.
- Ongoing debate over the relative value versus conventional pelvic floor muscle exercise, especially in patients with mild symptoms.
Future research areas include:
- Establishing robust, evidence-based protocols tailored to FI subtypes.
- Investigating long-term adherence strategies to maintain results.
- Integrating home-based systems and telehealth support to expand access.
- Further assessment of combination therapies (medication, neuromodulation, behavioral therapy) with biofeedback as a core component.
Frequently Asked Questions (FAQs)
Q: Who is the ideal candidate for biofeedback therapy in fecal incontinence?
A: Patients with mild to moderate FI, especially those exhibiting functional deficits in sphincter contraction, sensory perception, or pelvic coordination. It is less effective for those with complete sphincter tears or severe central nervous system injuries.
Q: How many sessions of biofeedback are typically required?
A: Most programs recommend about 6–10 structured sessions, spaced over several weeks. Maintenance and home practice improve durability of results. Some patients benefit from booster sessions as needed.
Q: Is biofeedback therapy safe?
A: Yes, biofeedback is considered a safe, non-invasive therapy with no systemic side effects; minor discomfort may occur from rectal sensors or probes during initial sessions.
Q: What are the main outcomes measured to determine success?
A: Key outcomes include reduction in the number of incontinence episodes, improved patient-reported continence and quality of life, and sometimes objective changes in anorectal pressures or EMG readings.
Q: Can biofeedback be combined with other treatments?
A: Yes, biofeedback is often integrated with dietary management, stool-bulking agents, antidiarrheal medications, and in some cases, surgical correction for optimum functional outcome.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3816189/
- https://jamanetwork.com/journals/jamasurgery/fullarticle/596907
- https://www.blueshieldca.com/content/dam/bsca/en/provider/docs/2024/February/PRV_Biofeedback_TX_Fecal_Incontinence_Constipation.pdf
- https://www.bladderandbowel.org/conservative-treatment/biofeedback/
- https://www.youtube.com/watch?v=Ysdaa_8x8H0
- https://www.jnmjournal.org/journal/view.html?volume=16&number=2&spage=177
- https://www.continence.org.au/news/biofeedback-therapy-bowel-continence
- https://www.bluecrossma.org/medical-policies/sites/g/files/csphws2091/files/acquiadam-assets/308%20Biofeedback%20as%20a%20Treatment%20of%20Fecal%20Incontinence%20or%20Constipation%20prn.pdf
Read full bio of medha deb












