Understanding Atherosclerosis: Plaque Build-up and the Impact on Arteries
Balanced diet, regular exercise, and stress reduction help preserve blood vessel vitality.
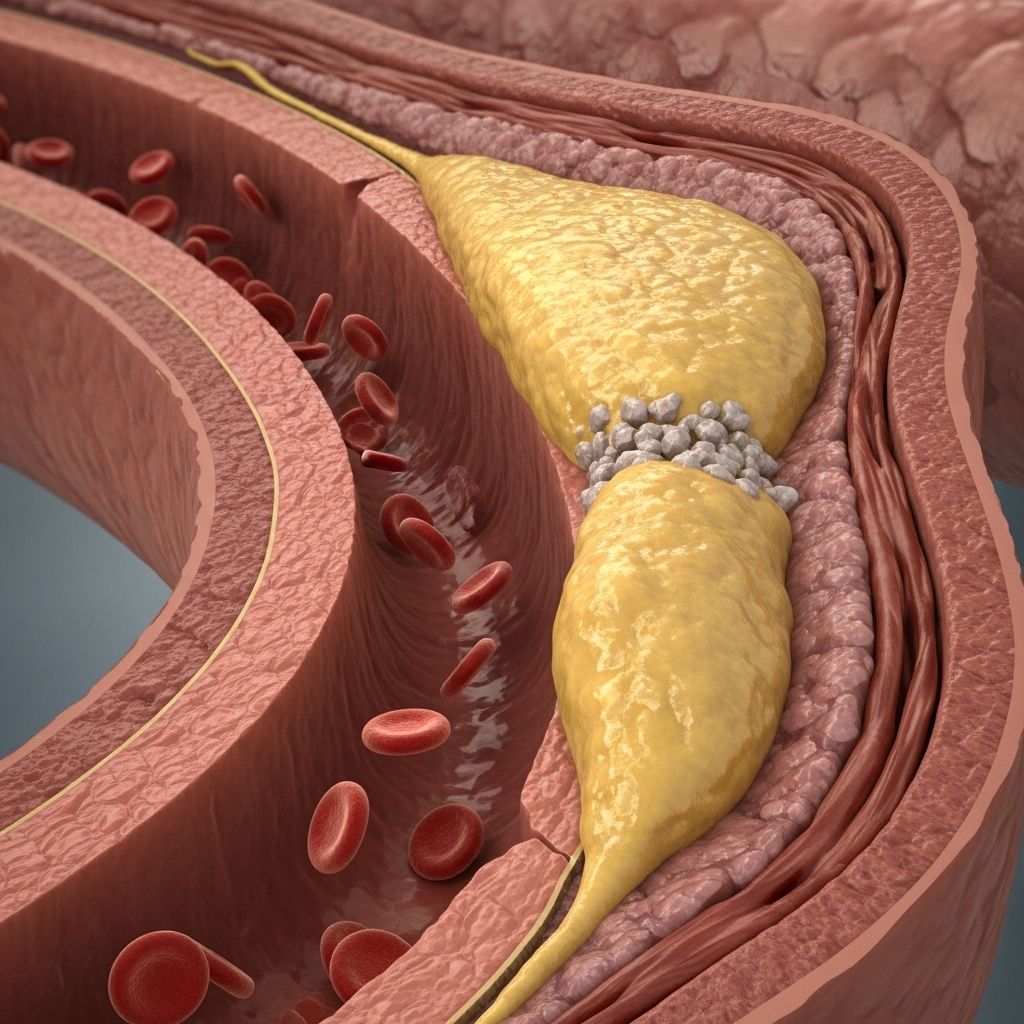
Atherosclerosis is a fundamental disease process that underlies many of the most common and deadly forms of cardiovascular disease. It involves the build-up of fatty deposits, known as plaque, inside the arteries, ultimately narrowing them and restricting blood flow. Over time, this narrowing can trigger life-threatening complications, including heart attack, stroke, and peripheral artery disease. This comprehensive guide explores the mechanisms, causes, risk factors, symptoms, diagnostic approaches, consequences, prevention strategies, and frequently asked questions associated with atherosclerosis.
Table of Contents
- What Is Atherosclerosis?
- How Does Plaque Develop?
- Types of Affected Arteries
- Risk Factors for Atherosclerosis
- Causes of Atherosclerosis
- Symptoms of Atherosclerosis
- Disease Progression: Stages of Atherosclerosis
- Diagnosis and Assessment
- Complications of Atherosclerosis
- Prevention of Atherosclerosis
- Treatment Strategies
- Frequently Asked Questions
What Is Atherosclerosis?
Atherosclerosis is a chronic, progressive disease characterized by the hardening and narrowing of the arteries due to plaque build-up. The term comes from the Greek words ‘athero’ (gruel or paste) and ‘sclerosis’ (hardness), describing the fatty deposits that stiffen arterial walls over time. Unlike arteriosclerosis, a general term for arterial stiffening, atherosclerosis specifically refers to the gradual accumulation of fatty, waxy substances on the inner lining of arteries.
The disease can affect any artery in the body, but it most commonly impacts the coronary arteries supplying the heart, carotid arteries supplying the brain, and peripheral arteries serving the limbs. Reduced arterial flexibility and narrowing after plaque formation can severely impede blood flow, depriving organs and tissues of oxygen and essential nutrients.
Key Facts about Atherosclerosis
- Process: Plaque accumulates on arterial walls, causing restriction or blockage of blood flow.
- Systemic Impact: Can affect arteries in the heart, brain, limbs, kidneys, and more.
- Main Outcome: Major risk factor for heart attack, stroke, peripheral artery disease.
How Does Plaque Develop?
Atherosclerosis begins with some form of damage to the endothelium, the fragile inner lining of the artery. This damage can be subtle and accumulate over the years due to modifiable and non-modifiable factors. Once the endothelium is compromised, low-density lipoprotein (LDL) cholesterol infiltrates the vessel wall. The immune system responds, leading to inflammation and further arterial wall damage.
Key Steps in Plaque Formation:
- Endothelial Damage: Factors like high blood pressure, toxins from smoking, or high blood sugar cause tiny injuries to arterial walls.
- LDL Cholesterol Penetration: LDL particles seep beneath the damaged endothelium.
- Immune System Response: White blood cells (macrophages) rush to the site, engulf LDL particles, and form foam cells.
- Inflammation: Chronic inflammation attracts more immune cells, perpetuating a cycle of damage.
- Plaque Formation: Over time, fatty streaks develop into larger plaques containing cholesterol, dead cells, calcium, and fibrous tissue.
- Arterial Narrowing and Hardening: The plaques stiffen the arteries and restrict blood flow.
- Plaque Rupture and Blood Clots: When plaques rupture, they expose their inner contents, triggering the formation of blood clots that can block the artery completely.
Types of Affected Arteries
The clinical consequences of atherosclerosis depend on which arteries are affected by plaque accumulation and narrowing.
| Artery Type | Associated Condition | Key Symptoms |
|---|---|---|
| Coronary arteries | Coronary artery disease (CAD), heart attack | Chest pain (angina), shortness of breath, arrhythmia |
| Carotid arteries | Carotid artery disease, stroke | Sudden numbness, weakness, difficulty speaking, vision changes, facial droop |
| Peripheral arteries (legs, arms) | Peripheral artery disease (PAD) | Leg pain while walking (claudication), cold feet, sores on feet, numbness |
| Renal (kidney) arteries | Chronic kidney disease, hypertension | High blood pressure, kidney dysfunction |
| Mesenteric arteries (intestines) | Mesenteric ischemia | Severe abdominal pain after meals, weight loss |
Risk Factors for Atherosclerosis
The precise cause of atherosclerosis is complex and multifactorial. However, certain risk factors significantly increase susceptibility to plaque build-up. These can be categorized as non-modifiable and modifiable:
- Increasing Age: Risk accelerates after age 45 in men and 55 in women.
- Family History: Genetic predisposition to heart disease or high cholesterol.
- Sex: Males are at higher risk earlier in life; risk for women rises after menopause.
- High LDL Cholesterol (“bad” cholesterol)
- Low HDL Cholesterol (“good” cholesterol)
- High Triglycerides
- High Blood Pressure (Hypertension)
- Smoking or Tobacco Use
- Diabetes or Insulin Resistance
- Obesity, Especially Abdominal Obesity
- Physical Inactivity
- Unhealthy Diet (high in saturated fat, low in fruits/vegetables)
- Chronic Inflammation (autoimmune conditions, chronic infections)
- Excess Alcohol Consumption
- Sleep Apnea
- High C-reactive protein (CRP)
- Chronic Stress
Causes of Atherosclerosis
The development of atherosclerosis starts with arterial wall injury. This damage may result from:
- Unhealthy Lifestyle Choices: High-fat diet, smoking, excessive alcohol use, lack of exercise.
- Medical Conditions: High blood pressure, high cholesterol, diabetes, metabolic syndrome, autoimmune and inflammatory diseases.
- Genetics: A family history of early cardiovascular disease increases risk.
- Other Factors: Age-related changes, chronic stress, and infections may also contribute.
Plaque formation may begin in childhood and progress silently for decades before causing noticeable problems.
Symptoms of Atherosclerosis
Early atherosclerosis is typically silent and develops gradually. Symptoms usually appear when an artery is critically narrowed or blocked. The nature of the symptoms depends on which arteries are involved:
- Coronary arteries: Chest pain/pressure (angina), arrhythmia, shortness of breath, heart attack.
- Carotid arteries: Sudden numbness or weakness (especially on one side of the body), trouble with speech or understanding, facial muscle droop, paralysis, loss of vision in one or both eyes, severe headache.
- Peripheral arteries (legs, arms): Pain while walking (intermittent claudication), numbness, leg/calf cramps, cold feet, non-healing sores.
- Renal arteries: High blood pressure, kidney dysfunction or failure.
- Mesenteric arteries (intestines): Severe abdominal pain after meals, weight loss, diarrhea.
- Men: Erectile dysfunction can be an early sign due to reduced blood flow to the pelvic area.
Early recognition of these signs is crucial, as significant artery blockage and permanent damage can occur before symptoms develop.
Disease Progression: Stages of Atherosclerosis
Atherosclerosis develops over a series of stages that reflect increasing arterial damage:
- 1. Endothelial Injury: Initial microscopic damage to the inner layer of the artery, often from high blood pressure, toxins, or high blood sugar.
- 2. Fatty Streak Formation: White blood cells ingest cholesterol, forming streaks of fatty material on the artery walls.
- 3. Fibrous Plaque Development: Smooth muscle cells and more lipids are added, creating a fibrous cap and further narrowing the artery.
- 4. Complicated Lesion (Plaque Rupture): An unstable plaque ruptures, exposing inflammatory material, which can trigger a blood clot and sudden blockage of the artery, leading to critical events like heart attack or stroke.
Diagnosis and Assessment
Diagnosing atherosclerosis involves a combination of clinical history, risk assessment, physical examination, and specialized tests, including:
- Blood Tests: Measure cholesterol, triglycerides, blood sugar, C-reactive protein (marker of inflammation).
- Blood Pressure Monitoring: Hypertension is a common finding and risk factor.
- Imaging Studies:
- Ultrasound: Identifies plaque in carotid or peripheral arteries.
- CT Angiography: Visualizes vessels and detects plaque/calcification.
- Coronary Angiography: X-ray test with dye to view blockages in coronary arteries.
- Ankle-brachial index: Compares blood pressure in the ankle and arm to screen for peripheral artery disease.
- Electrocardiogram (ECG or EKG): Detects prior heart damage or arrhythmias.
- Stress Tests: Evaluate heart function under controlled exercise or with medications.
Complications of Atherosclerosis
If left untreated, atherosclerosis can progress unnoticed until it triggers severe, sometimes fatal, complications:
- Heart Attack (Myocardial Infarction): Plaque rupture in a coronary artery leads to a blood clot that stops blood flow to the heart muscle.
- Stroke: Blockage or rupture of a carotid artery cuts off blood supply to brain tissue.
- Peripheral Artery Disease (PAD): Reduced blood flow to limbs causes pain, non-healing sores, and in severe cases, tissue death (gangrene).
- Chronic Kidney Disease: Plaque in renal arteries impairs kidney function.
- Aneurysm: Weakening of the arterial wall can lead to dangerous bulges or ruptures, especially in the aorta.
- Sudden Cardiac Death: Often a result of arrhythmia following a massive heart attack.
Prevention of Atherosclerosis
Although some risk factors cannot be modified (age, genetics), lifestyle choices play a key role in either increasing or reducing the risk of developing atherosclerosis. Preventive strategies include:
- Eat a heart-healthy diet: Rich in fruits, vegetables, whole grains, legumes, fish, and healthy fats (like olive oil). Limit saturated fats, trans fats, and processed foods.
- Exercise regularly: Aim for at least 150 minutes of moderate aerobic activity each week (such as brisk walking or cycling).
- Maintain a healthy weight: Obesity, especially in the abdominal area, is a major risk factor.
- Quit smoking and avoid tobacco: Even low levels of smoking accelerate atherosclerosis.
- Control blood pressure, cholesterol, and diabetes: Work with your healthcare provider to manage these conditions with medication if necessary.
- Limit alcohol intake: Excess drinking is linked to high blood pressure and elevated cholesterol.
- Manage stress: Long-term stress raises inflammatory markers and blood pressure.
- Get regular health screenings: Early detection and intervention can help halt progression.
Treatment Strategies
While atherosclerosis cannot be fully reversed, it can often be managed and its progression slowed, leading to substantially lower risk of life-threatening events. Treatment typically involves a combination of lifestyle changes and medications. In some cases, surgical procedures may be necessary.
Common Treatment Options:
- Lifestyle modifications (as above)
- Medications:
- Statins (to lower cholesterol)
- Blood pressure medications (ACE inhibitors, beta-blockers, ARBs)
- Antiplatelet agents (aspirin, clopidogrel) to reduce clot formation
- Medications for diabetes control
- Interventional or surgical procedures:
- Angioplasty and stenting: A catheter with a balloon opens the blocked artery; a small mesh tube (stent) is left in place to keep it open.
- Coronary artery bypass grafting (CABG): Uses healthy vessels to bypass narrowed or blocked coronary arteries.
- Endarterectomy: Surgical removal of plaque from an artery, most often in the carotid artery.
Frequently Asked Questions (FAQs)
What are six common symptoms of atherosclerosis?
Symptoms depend on artery location and may include:
- Chest pain or pressure (angina)
- Heart palpitations or arrhythmias
- Shortness of breath
- Problems with thinking or memory
- Leg pain while walking (intermittent claudication)
- Erectile dysfunction in men
What are the four stages of atherosclerosis?
- Endothelial injury
- Fatty streak formation
- Fibrous plaque development
- Complicated lesion (plaque rupture and thrombosis)
How is atherosclerosis diagnosed?
Diagnosis uses a combination of history/risk assessment, blood tests for cholesterol and inflammation, blood pressure measurements, imaging (ultrasound, CT, angiography), and functional tests (stress testing, ankle-brachial index).
What lifestyle changes help prevent or slow atherosclerosis?
- Eat a diet low in saturated and trans fats
- Increase fruits, vegetables, and fiber intake
- Exercise regularly
- Control blood sugar and cholesterol
- Quit smoking
- Maintain a healthy weight
Can atherosclerosis be reversed?
While extensive plaque build-up cannot be fully removed, aggressive lifestyle changes and medication can reduce the risk, slow plaque progression, and in some cases even shrink certain cholesterol-rich, non-calcified plaques.
What is the impact on life expectancy?
Without effective intervention, atherosclerosis reduces life expectancy—potentially by 10–16 years after heart attack or stroke. Healthy living and modern medications can significantly lengthen lifespan and quality of life.
Note: Speak to your healthcare provider for personalized advice and early detection, especially if you have risk factors or symptoms suggestive of atherosclerosis.
References
- https://www.webmd.com/heart-disease/what-is-atherosclerosis
- https://medlineplus.gov/atherosclerosis.html
- https://www.advocatehealth.com/health-services/advocate-heart-institute/conditions/vascular-disease/atherosclerosis
- https://www.mayoclinic.org/diseases-conditions/arteriosclerosis-atherosclerosis/symptoms-causes/syc-20350569
- https://my.clevelandclinic.org/health/diseases/16753-atherosclerosis-arterial-disease
- https://www.pennmedicine.org/conditions/atherosclerosis
- https://www.aurorahealthcare.org/services/heart-vascular/conditions/atherosclerosis
- https://www.nhlbi.nih.gov/health/atherosclerosis
Read full bio of Sneha Tete












