Appendicitis vs. Diverticulitis Pain: A Comprehensive Clinical & Diagnostic Comparison
Understanding inflammation patterns improves care strategies and reduces complications.
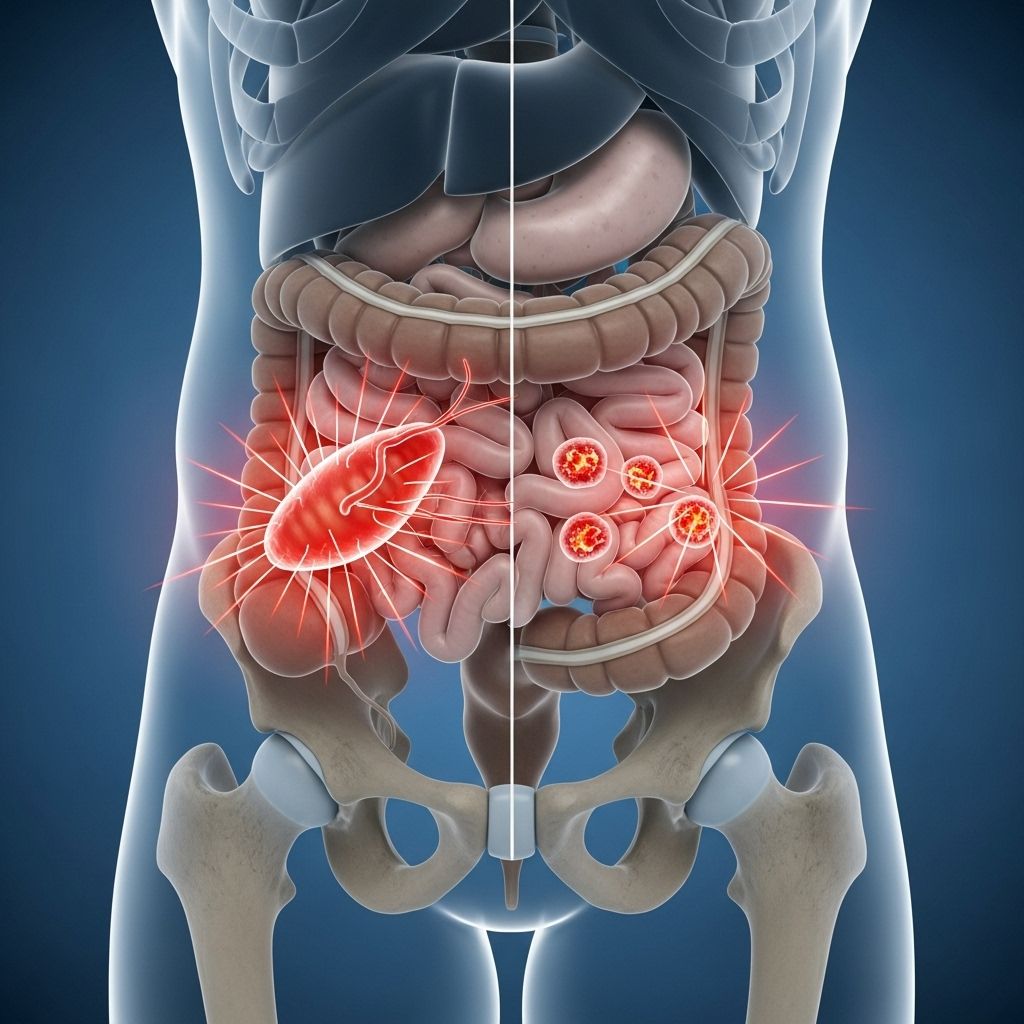
Abdominal pain is one of the most frequent and challenging complaints in emergency and gastroenterology settings. Two common culprits, appendicitis and diverticulitis, present overlapping symptoms but require distinct approaches to management. Differentiating between the pain profiles and associated features of these conditions is critical for timely, effective treatment, and improved patient outcomes.
Table of Contents
- Introduction
- Appendicitis and Diverticulitis: Key Definitions
- Causes and Risk Factors
- Comparative Pain Location and Onset
- Other Symptoms: Similarities and Differences
- Diagnostic Approaches
- Clinical Challenges and Misdiagnosis
- Treatment and Management
- When to Seek Medical Help
- Frequently Asked Questions (FAQs)
Introduction
Acute pain localized to the abdomen may signal many underlying problems. Among these, appendicitis and diverticulitis are two of the most serious, often requiring emergency intervention. Both conditions may mimic each other, and their pain characteristics overlap, particularly when diverticulitis arises on the right side of the colon, a phenomenon sometimes referred to as the “right-sided appendicitis”. Conversely, classic diverticulitis usually presents on the left, leading to its nickname: “the left side appendicitis”.
This comprehensive article examines the pain profiles, distinguishing clinical features, diagnostic strategies, and treatment implications for appendicitis and diverticulitis, guiding clinicians and informed patients in the recognition and management of these important conditions.
Appendicitis and Diverticulitis: Key Definitions
| Condition | Definition | Usual Pain Location | Typical Affected Age Group |
|---|---|---|---|
| Appendicitis | Inflammation of the vermiform appendix, often due to obstruction. | Right lower quadrant (RLQ), near McBurney’s point | Children, teenagers, young adults, but can occur at any age |
| Diverticulitis | Inflammation or infection of diverticula (small intestine or colon pouches). | Most commonly left lower quadrant (LLQ; sigmoid colon); but can be right-sided (cecal) and mimic appendicitis | Older adults; prevalence increases with age |
Causes and Risk Factors
Appendicitis
- Cause: Blockage of the appendix lumen (fecalith, inflammation, foreign body) leading to infection and swelling.
- Other factors: Genetic predisposition, recent gastrointestinal infection, lymphoid hyperplasia.
- Common after viral illnesses: In children, post-infectious lymphoid swelling may obstruct the appendix.
- Peak Incidence: Teens and young adults, but anyone can develop appendicitis.
Diverticulitis
- Cause: Infection or inflammation of one or more diverticula, often due to micro-perforation or impaction of fecal material.
- Main risk factor: Aging; prevalence rises with age due to weakening of colonic wall.
- Additional risk factors: Low-fiber diet, obesity, chronic constipation, sedentary lifestyle, genetics.
- Location matters: In Western countries, diverticulitis is most often sigmoid (LLQ); in Asian populations, cecal (RLQ) diverticulitis is frequent and may mimic appendicitis.
Comparative Pain Location and Onset
Appendicitis Pain
- Classically begins as vague, poorly localized peri-umbilical discomfort, then migrates to the right lower quadrant (RLQ) within 24 hours.
- Sharp, steady pain develops at McBurney’s point (one-third the distance from the anterior superior iliac spine to the navel).
- Typical progression: Onset over 12-24 hours, worsening steadily; may be accompanied by rebound tenderness and guarding.
- Aggravated by movement, coughing, or pressure.
Diverticulitis Pain
- Usually starts as constant, aching pain in the lower abdomen.
- Left-sided, over the sigmoid colon, is most typical in Western patients (“the left side appendicitis”).
- Right-sided symptoms may occur (particularly in Asian or younger populations) and commonly lead to confusion with appendicitis.
- Onset is more gradual and insidious, often developing over several days.
- Pain is generally less likely to sharply localize at McBurney’s point, and may feel more diffuse or lateral in the lower abdomen.
- Associated with feelings of fullness or bloating; pain may intensify with eating or after meals.
Key Comparative Point
- If pain is maximal lateral to McBurney’s point or lacks classic migratory pattern, or if there is no clear prodrome, right-sided diverticulitis should be considered, especially in older patients.
- Left lower quadrant pain that is new and severe in a middle-aged or older patient is most often diverticulitis, unless proven otherwise.
Other Symptoms: Similarities and Differences
| Symptom | Appendicitis | Diverticulitis |
|---|---|---|
| Fever | Common, develops after pain | Common, may be mild; higher if severe |
| Nausea/Vomiting | Very common (often follows pain onset) | Possible, but less pronounced |
| Altered bowel habits | Mild constipation or diarrhea | More frequent – constipation, diarrhea, or both |
| Urinary symptoms | Occasional urinary frequency if inflamed appendix irritates the bladder | Possible, especially if pelvic colon involved |
| Rebound tenderness | Classic, focused at McBurney’s point | Less well-localized, mild or absent in many cases |
| General malaise | Common in acute phase | Common; more pronounced with severe infection |
| Bloody stool | Uncommon | Rare, but possible if diverticula bleed |
Diagnostic Approaches
Because the clinical presentation often overlaps — especially with right-sided diverticulitis — precise diagnosis requires careful evaluation and the use of imaging or laboratory testing.
1. Clinical Examination
- Appendicitis: Classic McBurney’s point tenderness, rebound, and localized guarding. Rovsing’s, psoas, and obturator signs may be present.
- Diverticulitis: Lower quadrant tenderness (LLQ or RLQ), may be less well demarcated; less rebound, often more diffuse discomfort.
2. Laboratory Findings
- Appendicitis: Elevated white blood cell count (WBC)—especially with increased “segmented” neutrophils.
- Diverticulitis: WBC may be raised, but less dramatically than in appendicitis (lower median WBC and a higher relative lymphocyte fraction).
- Blood cultures if severe or sepsis is suspected.
3. Imaging Studies
- Ultrasound: First-line for suspected appendicitis in children, pregnant women.
- Computed Tomography (CT): Gold standard for both, shows inflamed appendix or diverticula, abscess, or perforation. Key for differentiating right-sided diverticulitis from appendicitis but is imperfect — up to 80% of right-sided diverticulitis may initially be misdiagnosed as appendicitis.
- Findings: Saccular protrusions in diverticulitis, localized inflammation, possible peri-colonic fluid for both. Appendiceal wall thickening and fluid for appendicitis.
Clinical Challenges and Misdiagnosis
- Overlap in symptoms: Both can cause right lower quadrant pain, fever, and gastrointestinal symptoms.
- Right-sided diverticulitis masquerades as appendicitis and is often only diagnosed during surgery. Studies show only 3–6% of patients with right-sided diverticulitis are correctly diagnosed preoperatively.
- Radiological limitations: CT scan sensitivity for appendiceal diverticulitis is variable (24–86%), so clinical judgment remains crucial.
- Repetition: Diverticulitis is more likely to present in older patients with repeated, similar episodes of pain, while appendicitis usually presents acutely and singularly.
Treatment and Management
Appendicitis
- Uncomplicated: Early cases may occasionally be managed with antibiotics, but appendectomy (surgical removal of the appendix) remains standard.
- Complicated (perforation, abscess): May require hospitalization, intravenous antibiotics, drainage of abscesses, surgery.
Diverticulitis
- Mild cases: Treated with oral antibiotics, clear liquid diet, and rest; resolve without invasive intervention in most individuals.
- Moderate/severe/complicated (abscess, perforation): Hospitalization, IV antibiotics, potential for surgery if not responsive or with recurrent episodes.
- Dietary modulations, increased fiber (once acute phase resolved), hydration to decrease future attacks.
Recurrent Pain Management
- Recurrent diverticulitis: May consider surgery after multiple or complicated episodes.
- Recurrent “appendicitis”: Unusual; residual or chronic appendicitis can sometimes occur and warrants thorough evaluation.
When to Seek Medical Help
- Sudden, severe, or progressively worsening lower abdominal pain.
- Pain accompanied by fever, inability to eat or drink, vomiting, or signs of shock (weakness, fainting, confusion).
- History of diverticulosis with new severe pain—especially if it does not resolve or is associated with sepsis or peritonitis signs.
- Any suspicion of appendicitis—delaying can result in perforation or sepsis, both potentially life-threatening.
Frequently Asked Questions (FAQs)
Q: Can diverticulitis pain be mistaken for appendicitis?
Yes. Especially in cases of right-sided diverticulitis, the pain can closely mimic appendicitis, leading to potential misdiagnosis. Clinical exam and imaging are crucial for differentiation.
Q: Where is appendicitis pain usually felt, and how does it begin?
Typically, appendicitis pain starts as a vague discomfort around the navel (peri-umbilical region) and migrates over several hours to the right lower quadrant (McBurney’s point), where it becomes more intense and localized.
Q: Is fever always present in appendicitis or diverticulitis?
Not always. Mild fever is common in both but may be absent in early disease. High fever or signs of severe infection suggest possible perforation or complications and require urgent attention.
Q: How is the diagnosis confirmed?
A combination of careful history, focused physical exam, laboratory tests (WBC count), and most importantly, imaging (abdominal ultrasound or CT scan) confirms the diagnosis and rules out other emergencies.
Q: How does pain from diverticulitis differ from appendicitis?
Diverticulitis pain tends to be more constant and is usually felt in the left lower abdomen (unless right-sided). It often develops more gradually. Appendicitis pain typically starts as vague mid-abdominal discomfort and becomes sharp, localized, and severe in the right lower quadrant within hours.
Q: What is the risk of complications?
Both conditions can lead to abscesses, perforation, and peritonitis if untreated. Perforation risk is particularly high in appendiceal diverticulitis, which can have a fourfold greater risk than typical appendicitis.
Q: How likely is it for diverticulitis to recur?
Many people with an initial episode of diverticulitis have no recurrence, but repeated or severe attacks increase risk for future events and may prompt surgical consideration.
Q: Can lifestyle changes help prevent diverticulitis?
Yes. Maintaining a high-fiber diet, staying active, and adequate hydration support colon health and reduce the risk of diverticulosis progressing to diverticulitis.
Q: When should surgery be considered?
Surgery is indicated for appendicitis (standard of care) and for patients with diverticulitis who have complications such as perforation, abscess, or recurrent, severe episodes.
Conclusion
Discerning appendicitis from diverticulitis hinges on pain location, nature of onset, associated symptoms, and risk factors. However, given the substantial clinical overlap, especially with right-sided diverticulitis, imaging and lab evaluation remain essential. Prompt, accurate diagnosis ensures appropriate and effective treatment, minimizing risk of serious complications. If you or someone you know is experiencing new, severe lower abdominal pain, seek medical evaluation without delay.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2628084/
- https://www.facs.org/for-medical-professionals/news-publications/journals/case-reviews/issues/v4n1/liu-appendiceal-diverticulitis/
- https://www.youtube.com/watch?v=Lg4jWE4VinQ
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9292704/
- https://onlinelibrary.wiley.com/doi/10.1155/2020/4947192
Read full bio of medha deb












