Altitude Training’s Impact on Intestinal Barrier Function: Physiological Mechanisms, Risks, and Adaptations
Workouts in thin air can strain the digestive lining, making recovery support essential.
Altitude training, a cornerstone of athletic conditioning and a necessity for many occupational groups, is well known for facilitating hematologic and respiratory adaptations. However, less appreciated—and increasingly recognized—is its impact on the gastrointestinal system, especially the intestinal barrier function. This article provides a comprehensive examination of how high-altitude exposure, when combined with physical exertion, may compromise or alter the intestinal barrier, the underlying mechanisms involved, the role of gut microbiota, risks of systemic inflammation, and potential adaptation and prevention strategies.
Table of Contents
- Introduction
- Understanding the Intestinal Barrier
- Altitude Training: Overview and Physiological Effects
- How Altitude Training Affects the Intestinal Barrier
- Mechanisms Behind Barrier Impairment
- Altitude, Exercise, and Gut Microbiota Balance
- Inflammatory Responses and Systemic Implications
- Populations at Risk
- Adaptation and Protection Strategies
- Current Gaps and Future Research
- Frequently Asked Questions (FAQs)
Introduction
Altitude training involves physical training at elevations typically above 2,000 meters, harnessing the body’s response to reduced oxygen pressure (hypoxia) to improve sports performance or operational capability. While widely studied for its effects on endurance, concerns about its impact on gastrointestinal health—and specifically the integrity of the intestinal barrier—have emerged in recent years. Symptoms such as nausea, diarrhea, and vomiting are frequently reported at high altitudes, sometimes grouped as ‘high altitude gastrointestinal stress syndrome’.
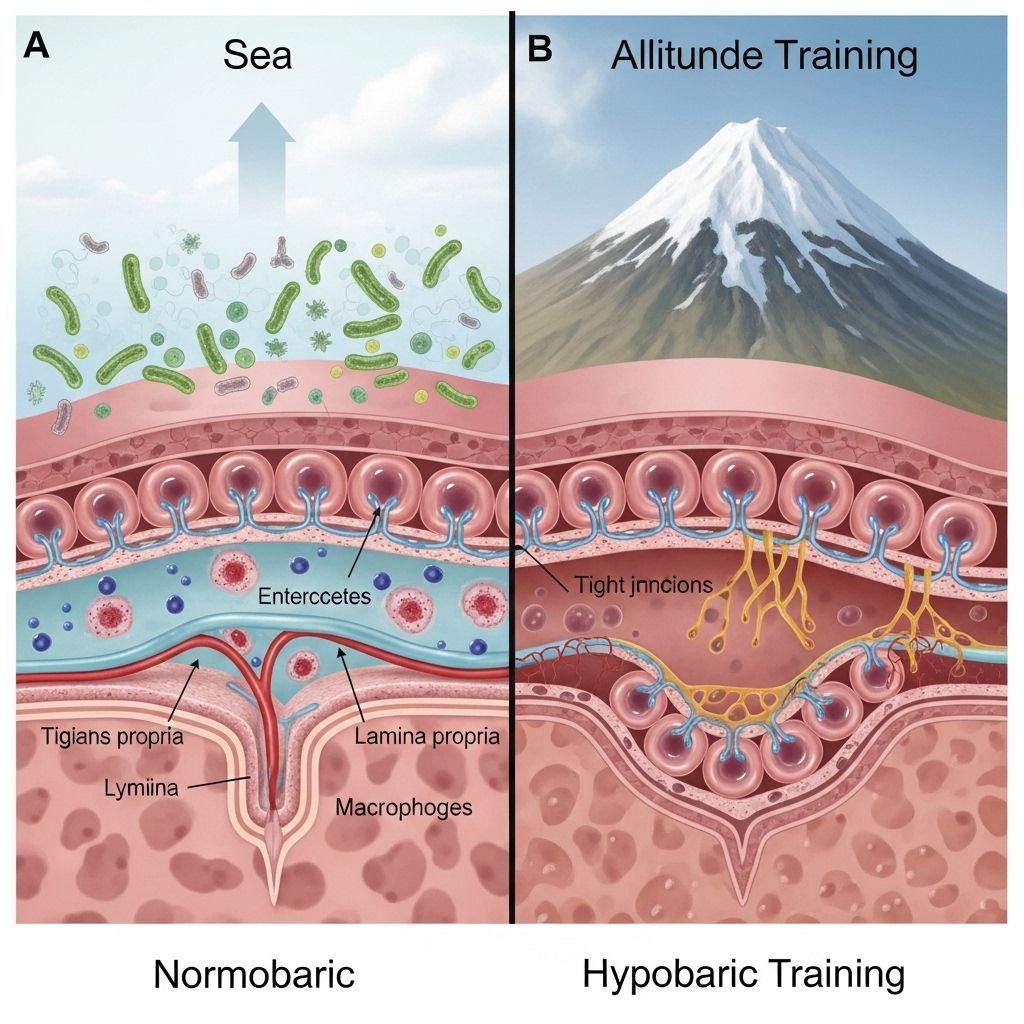
Understanding the Intestinal Barrier
The intestinal barrier is a complex, multi-layered system composed of:
- Epithelial cells and tight junctions, which physically restrict the passage of harmful substances.
- A mucosal layer that provides the first line of defense against pathogens.
- Local immune cells that respond to invaders breaching the barrier.
- Resident gut microbiota that interact with and maintain the barrier’s integrity.
When intact, this barrier prevents pathogens and toxins from entering the circulation. When compromised, increased intestinal permeability (“leaky gut”) allows for translocation of bacteria and inflammatory molecules, potentially leading to local and systemic illness.
Altitude Training: Overview and Physiological Effects
Altitude training exposes the body to hypobaric hypoxia—lower oxygen levels due to reduced atmospheric pressure. Key physiological effects include:
- Increased red blood cell (RBC) count and hematocrit (HCT), improving oxygen-carrying capacity.
- Enhanced ventilatory response (increased breathing rate).
- Redistribution of blood flow, including possible reductions in splanchnic (intestinal) circulation.
While beneficial for endurance performance, these changes can inadvertently compromise gastrointestinal perfusion, especially under added exercise stress, making the intestinal barrier vulnerable to hypoxic injury.
How Altitude Training Affects the Intestinal Barrier
Research demonstrates that both simulated and real altitude training can:
- Damage the small intestinal mucosa, the inner lining critical to barrier function.
- Increase growth of pathogenic bacteria within the small intestine.
- Heighten intestinal permeability, enabling bacteria and inflammatory molecules to cross into the bloodstream.
- Trigger gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal discomfort, especially in the first days at altitude.
Evidence from Animal and Human Studies
Studies using animal models (e.g., rats trained at simulated altitude) reveal significant injuries to the mucosal barrier after even brief exposures, with increased levels of key inflammatory molecules like IL-6 and TNF-α. In human studies, ascent to >2,500 m is associated with increased biomarkers of intestinal barrier dysfunction and gastrointestinal complaints.
Mechanisms Behind Barrier Impairment
The injury to the intestinal barrier at altitude is the result of several converging mechanisms:
- Hypoxia-Induced Stress: Low oxygen tension directly injures epithelial cells and disrupts tight junction proteins.
- Reduced Splanchnic Perfusion: Blood flow is diverted away from the gut to prioritize vital organs, compounding hypoxic injury.
- Inflammatory Cytokine Cascade: Hypoxic and mechanical (exercise) stresses activate transcription factors like NF-κB, promoting the production of inflammatory cytokines (IL-6, TNF-α). These, in turn, loosen tight junctions, increasing permeability.
- Microbial Translocation: Barrier impairment allows bacteria and endotoxins to permeate, further amplifying systemic inflammation.
| Mechanism | Description |
|---|---|
| Hypoxia | Reduces oxygen supply to epithelial cells; increases oxidative stress |
| Splanchnic hypoperfusion | Decreases blood flow to the gut during exercise and altitude exposure |
| Inflammatory cytokines | Enhance intestinal permeability; disrupt tight junctions |
| Microbiota imbalance | Reduces beneficial bacteria, increases pathogens |
Altitude, Exercise, and Gut Microbiota Balance
Gut microbiota play a crucial role in preserving intestinal barrier integrity. Altitude and hypoxia have now been shown to profoundly impact microbial communities:
- Acute high-altitude exposures typically reduce microbiota diversity, favoring potentially pathogenic bacteria.
- Exercise at altitude may exacerbate negative shifts in gut flora.
- Imbalanced microbiota further weaken the mucosal barrier and promote inflammatory responses.
For example, studies found altered proportions of Firmicutes and Bacteroidetes, as well as overgrowth of opportunistic pathogens, in both animal models and humans after altitude exposure. These changes correlate with worsened mucosal integrity and increased inflammation.
Inflammatory Responses and Systemic Implications
With the breach of intestinal barrier comes:
- Heightened inflammatory responses, including upregulation of IL-6, TNF-α, and NF-κB in gut tissue and circulation.
- Systemic endotoxemia due to translocation of bacteria (and bacterial products, like LPS) into the bloodstream.
- Possible contribution to acute mountain sickness (AMS) pathophysiology.
These responses heighten the risk for broader health consequences, including multi-organ inflammation and prolonged recovery.
Populations at Special Risk
Those especially vulnerable to hypoxia-induced intestinal barrier dysfunction include:
- Endurance athletes participating in high-altitude events or training camps
- Military personnel and rescue workers deployed rapidly to high elevation
- Mountaineers, trekkers, and wildland firefighters
- Populations living at chronic high altitude, particularly during acclimatization
The speed of ascent, exercise intensity, baseline gut health, and genetic predispositions all affect the degree of risk and severity of symptoms.
Adaptation and Protection Strategies
Although full mitigation of altitude-induced barrier dysfunction may not always be possible, several strategies are under investigation:
- Gradual acclimatization: Slower ascent allows adaptation, lessening hypoxic injury.
- Optimized hydration and nutrition: Diets rich in prebiotics, probiotics, and antioxidants may help stabilize the microbiome and mucosa.
- Pharmacological aids: Certain medications (e.g., NSAIDs, when properly managed) and dietary supplements are being studied for their ability to reduce inflammation and preserve barrier function.
- Controlled exercise prescription: Modulating intensity and duration may minimize additive stress on the gut.
Early data suggest that some interventions—especially those targeting the gut microbiota—may prevent or limit barrier dysfunction at high altitude.
Current Gaps and Future Research
- Human studies are limited: Most data come from small human cohorts or animal models. More robust clinical trials are needed.
- Individual susceptibility unexplored: Future research should investigate why some individuals experience severe GI symptoms or barrier disruption, while others are protected.
- Role of specific nutrients and probiotics: More data are required on which nutritional interventions may be most protective.
- Long-term consequences: The long-term health implications of repeated altitude exposure on gut health remain to be clarified.
Frequently Asked Questions (FAQs)
What is the intestinal barrier and why is it important?
The intestinal barrier consists of the gut lining, tight junctions, mucus, and microbiota that together regulate what passes from the intestines into the bloodstream, protecting against infection and systemic inflammation.
How does altitude training affect the gut?
Altitude training can compromise blood flow to the gut, decrease oxygen delivery, disrupt gut microbial balance, increase intestinal permeability, and trigger inflammation, causing gastrointestinal symptoms and potential health risks, especially during initial exposure or with intense exercise at altitude.
Are high-altitude gastrointestinal symptoms common?
Yes, symptoms like nausea, vomiting, and diarrhea are common upon quick ascent to elevations above 2,000 meters. These are often linked to barrier dysfunction and local inflammation.
Can these effects be prevented?
Prevention strategies include gradual acclimatization, proper hydration and nutrition, and potentially dietary supplements (e.g., probiotics, antioxidants). Some medications have been studied but more research is needed to confirm their benefits and safety at high altitude.
Who should be most concerned about these risks?
Athletes, military personnel, rescue workers, and anyone traveling or working at high elevations should be alert to these risks, particularly if rapidly ascending or engaging in strenuous exercise.
References and Further Reading
- Simulated altitude exercise training damages small intestinal mucosa barrier via elevated bacteria and inflammatory cytokines.
- High altitude exposures and intestinal barrier dysfunction: clinical and experimental evidence.
- Effects of high-altitude hypoxia and exercise on gut microbiota and barrier function.
- Unraveling the pathogenesis and prevention strategies for acute high-altitude illness with a focus on gastrointestinal complications.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6028221/
- https://digitalrepository.unm.edu/cgi/viewcontent.cgi?article=1147&context=educ_hess_etds
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10323920/
- https://www.nature.com/articles/s41522-025-00701-1
- https://febs.onlinelibrary.wiley.com/doi/10.1111/febs.16409
- https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1371247/full
Read full bio of Sneha Tete












