Allergens and Increased Susceptibility to Colds: Understanding the Connection Between Allergies and Viral Infections
Persistent nasal inflammation can compromise your airway’s antiviral defenses.
The interaction between allergens and the body’s immune system is complex, especially in the context of increased susceptibility to colds. Millions experience allergic rhinitis or other allergic conditions, often reporting more frequent or severe colds. This article delves deeply into the scientific understanding of this relationship, exploring mechanisms, risk factors, symptoms, prevention, and practical guidance for managing respiratory health.
Table of Contents
- Introduction: What Are Allergens and Colds?
- How Do Colds Affect the Immune System?
- Allergens, Allergies, and the Immune Response
- How Allergens Increase Vulnerability to Colds
- Clinical Evidence: Allergic Rhinitis and Cold Susceptibility
- Symptom Overlap: Allergies vs. Colds
- Who Is Most at Risk?
- Prevention and Management Strategies
- Common Myths About Allergies and Colds
- Frequently Asked Questions (FAQs)
- Conclusion
Introduction: What Are Allergens and Colds?
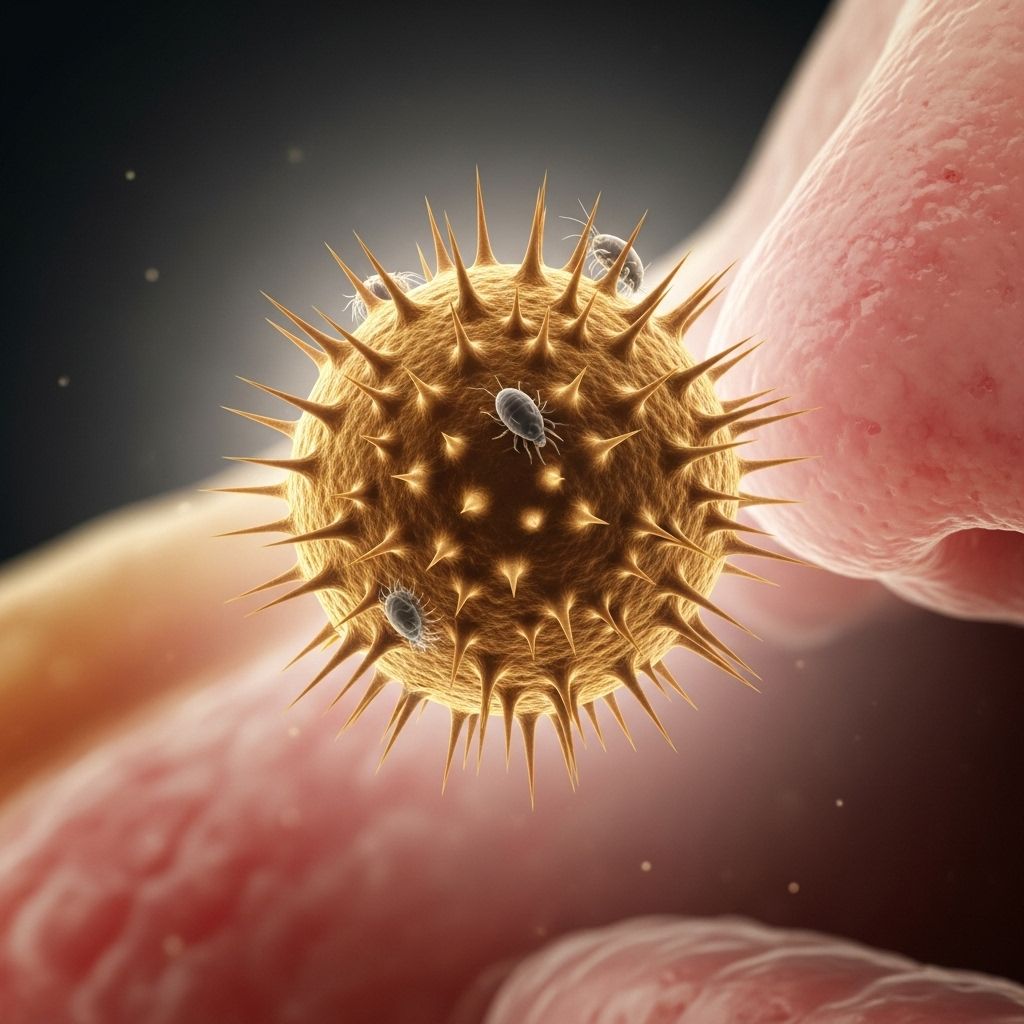
Allergens are substances that provoke an immune response in susceptible individuals, leading to symptoms of allergy. Typical airborne allergens include pollen, dust mites, animal dander, and mold spores. In contrast, the common cold is a viral infection—most often caused by rhinoviruses—that primarily affects the upper respiratory tract. While colds are usually mild and self-limiting, people with allergies often report more frequent or severe colds, suggesting an immunological link.
Understanding why this happens requires a closer look at the immune processes involved with both allergies and viral infections, particularly in the airway mucosa.
How Do Colds Affect the Immune System?
When a virus invades the upper respiratory tract, it triggers the innate immune response. Epithelial cells detect viral genetic material (DNA or RNA) through Pattern Recognition Receptors (PRRs). Activation of these receptors leads to the release of signaling proteins, such as:
- Interleukins (e.g., IL-6, IL-8) and interferons
- Tumor necrosis factor-alpha (TNF-α)
This release drives both systemic and local symptoms. Systemic symptoms (fever, malaise, muscle aches) are mediated by circulating cytokines, whereas local symptoms (nasal congestion, sore throat) result from inflammatory mediators like bradykinin and prostaglandins, which increase vascular dilation and nerve stimulation in the mucosa.
Allergens, Allergies, and the Immune Response
Individuals with allergic rhinitis or similar conditions experience an exaggerated immune response on exposure to allergens:
- Allergens trigger IgE production, priming mast cells and basophils to release histamine and other mediators on subsequent exposures.
- This cascade leads to classic symptoms such as sneezing, itching, rhinorrhea (runny nose), and congestion.
- The nasal mucosa in allergic individuals often exhibits chronic inflammation, increased eosinophils, and disrupted epithelial barriers compared to non-allergic controls.
This inflammation primes the airway for exaggerated responses to further irritants, including respiratory viruses.
How Allergens Increase Vulnerability to Colds
Several mechanisms may explain why allergic individuals are more susceptible to colds or experience worse symptoms:
- Compromised epithelial barrier: Allergic inflammation damages the integrity of the nasal lining, facilitating viral entry.
- Altered immune cell profiles: In allergic rhinitis, elevated eosinophils and altered numbers of mast cells and T-cells may disrupt normal antiviral defenses.
- Enhanced vascular permeability: Chronically inflamed mucosa is more prone to fluid leakage and swelling, increasing susceptibility to infection and more severe local symptoms.
- Impaired mucociliary clearance: Allergy-related mucus changes can reduce the airway’s ability to clear pathogens efficiently.
- Heightened responsiveness: Exposure to both allergens and viruses can produce a synergistic effect, exaggerating symptoms and possibly prolonging illness duration.
These mechanisms are supported by clinical observations: during the acute phase of colds, allergy sufferers display more pronounced inflammatory cell infiltration in the mucosa compared to non-allergic controls.
Clinical Evidence: Allergic Rhinitis and Cold Susceptibility
Several studies provide direct evidence for increased susceptibility or worse outcomes among individuals with allergic disorders:
- Research comparing patients with allergic rhinitis, those predisposed to sinusitis, and healthy controls found similar viral-induced increases in mucosal immune cells, but allergic individuals had higher eosinophil counts in the acute phase of infection, suggesting greater inflammation.
- The same studies showed thicker reticular basement membranes in allergic patients during colds, indicating ongoing remodeling and inflammation in the nasal tissues.
- Sinusitis-prone patients exhibited decreased mast cell and cytotoxic T cell numbers after infection, which may increase vulnerability to bacterial complications.
- Healthy controls displayed faster post-infection mucosal recovery, while allergic or sinusitis-prone individuals had lingering immune changes even after symptoms resolved.
In summary, allergy sufferers are not necessarily more likely to contract a cold, but their immune responses make the course of the illness more severe and recovery slower than in non-allergic peers.
Symptom Overlap: Allergies vs. Colds
Differentiating between allergies and the common cold can be challenging due to significant symptom overlap:
| Symptom | Allergies | Colds |
|---|---|---|
| Sneezing | Frequent, intense | Common, usually less intense |
| Runny nose | Clear, watery | Clear at first, may become thicker or yellow/green |
| Nasal congestion | Common | Common |
| Sore throat | Sometimes | Common |
| Itchy eyes/nose | Very common | Rare |
| Fever | Never | Sometimes (especially in children) |
| Duration | Weeks to months | Typically 7–10 days |
When new symptoms develop or pre-existing symptoms worsen, it can signal the onset of a viral infection in someone with allergies.
Who Is Most at Risk?
Not everyone with allergies experiences more frequent or severe colds, but the following factors can increase risk:
- Children and young adults: Immune systems are still developing and exposed to many respiratory viruses through schools and social interaction.
- Individuals with uncontrolled or moderate-to-severe allergic rhinitis
- People with asthma: Asthma often coexists with allergies and can further impair airway defenses.
- Sinusitis-prone individuals: Prone to secondary infections after a cold.
- People with chronic mucosal inflammation
Managing allergic inflammation is especially important for these higher-risk groups.
Prevention and Management Strategies
1. Allergen Avoidance and Control
- Keep windows closed during high pollen seasons.
- Use HEPA filters to reduce indoor allergen exposure.
- Wash bedding frequently and minimize soft furnishings in bedrooms.
2. Optimize Allergy Treatment
- Use prescribed antihistamines, nasal corticosteroids, or other controller medications to reduce chronic inflammation.
- Consider immunotherapy (allergy shots or sublingual tablets) for severe or persistent allergic rhinitis.
3. Support Mucosal Barrier Integrity
- Stay hydrated to keep mucus thin and improve mucociliary clearance.
- Use saline nasal rinses to reduce allergen and viral load on nasal surfaces.
4. General Cold Prevention
- Wash hands frequently, especially during cold season.
- Avoid close contact with individuals who are symptomatic.
- Maintain a balanced diet and adequate sleep to optimize immune response.
Important: For individuals with moderate-to-severe allergy symptoms or respiratory conditions, consult a healthcare provider for individualized management plans.
Common Myths About Allergies and Colds
- Myth: “You can always tell if it’s allergies or a cold.”
Fact: Many symptoms overlap, and only a healthcare provider can make a confident diagnosis in ambiguous cases. - Myth: “Colds are only caused by viruses, never by allergens.”
Fact: Allergens don’t cause colds, but they can increase susceptibility to viral infections. - Myth: “Antibiotics help if you have both allergies and a cold.”
Fact: Antibiotics do not treat viral infections or allergy symptoms; they are only useful for bacterial complications. - Myth: “People without allergies can’t get more colds.”
Fact: Anyone can catch a cold, but those with allergies may have a harder time with symptoms and recovery.
Frequently Asked Questions (FAQs)
Q: Can allergies directly cause a cold?
A: No. Colds are exclusively caused by viruses. Allergies can weaken mucosal defenses, making it easier for viruses to infect the airways.
Q: Why do I seem to get sick more often during allergy season?
A: During allergy season, chronically inflamed nasal passages may be more susceptible to viral infection, leading to more frequent or more severe colds.
Q: Is there any benefit to allergy immunotherapy in preventing colds?
A: While immunotherapy does not prevent viruses, reducing allergic inflammation may make the nasal mucosa more resilient and less likely to develop severe symptoms if infection occurs.
Q: What should I do if my allergy symptoms worsen during a cold?
A: Continue your prescribed allergy treatment and speak with your doctor. If symptoms are severe, or if you experience persistent high fever, severe headache, sinus pain, or shortness of breath, seek medical attention.
Q: How can I differentiate between a cold and allergy symptoms?
A: Allergy symptoms include itching and are generally worse with allergen exposure, while colds often include sore throat, cough, and systemic symptoms like mild fever and muscle aches. Consult a healthcare provider for a precise diagnosis if you are unsure.
Conclusion
The relationship between allergens and increased susceptibility to colds is rooted in immune system interactions and airway inflammation. Allergic individuals, especially those with uncontrolled rhinitis, can experience more severe symptoms and prolonged recoveries when infected with common cold viruses. Recognizing the overlap, managing allergies proactively, and adopting practical prevention strategies are essential to improving respiratory health and minimizing the impact of colds in those affected by allergies.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1809099/
- https://www.frontiersin.org/journals/allergy/articles/10.3389/falgy.2023.1224988/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10324571/
- https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/colds-allergies-sinusitis
- https://www.nature.com/articles/s41392-023-01344-4
Read full bio of Sneha Tete












