Acid Reflux 101: Causes, Symptoms, and Treatments Explained in Detail
Discover simple strategies to manage heartburn and support healthy digestion daily.
Acid Reflux 101: Causes, Symptoms, and Treatments Explained
Acid reflux is a widespread digestive issue that affects millions globally, manifesting as uncomfortable heartburn, regurgitation, and a host of related symptoms. Understanding the basics of acid reflux, its causes, the signs to watch for, and evidence-based treatments can empower individuals to manage and prevent this condition effectively. This guide provides a comprehensive look at acid reflux from causes to prevention, backed by medical research and clinical guidance.
Table of Contents
- What is Acid Reflux?
- Causes of Acid Reflux
- Who is at Risk?
- Common Symptoms of Acid Reflux
- How Acid Reflux is Diagnosed
- Lifestyle Changes for Acid Reflux Relief
- Medical Treatments for Acid Reflux
- Tips for Preventing Acid Reflux
- Possible Complications if Acid Reflux is Unmanaged
- Frequently Asked Questions
What is Acid Reflux?
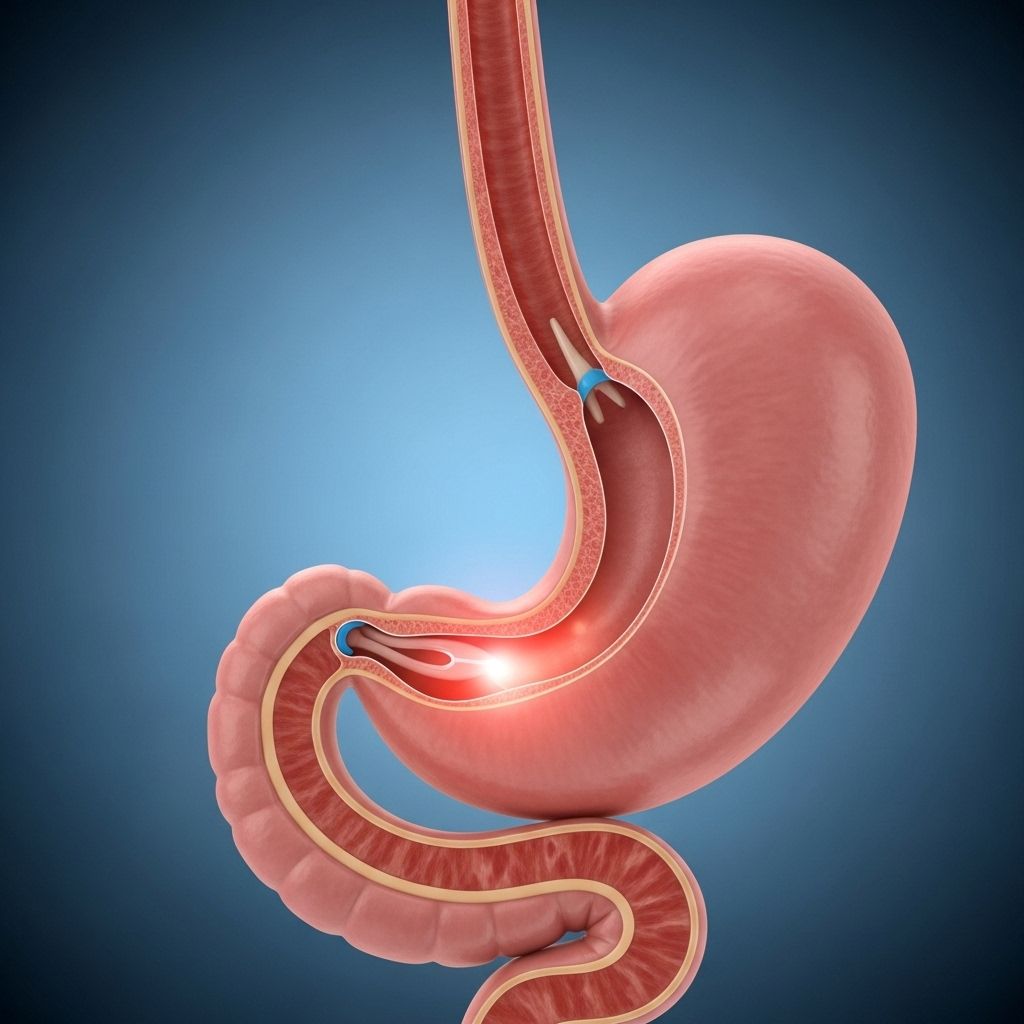
Acid reflux, medically known as gastroesophageal reflux (GER), is a condition where stomach acid flows backwards into the esophagus (the tube connecting the throat and the stomach). This backward movement, called reflux, can irritate the lining of your esophagus, leading to discomfort or pain commonly referred to as heartburn. While occasional reflux is harmless, chronic or severe episodes are classified as gastroesophageal reflux disease (GERD), a longer-term disorder that may require ongoing management and medical evaluation.
Causes of Acid Reflux
The root cause of acid reflux is typically a malfunction of the lower esophageal sphincter (LES). This ring of muscle at the junction of the esophagus and stomach acts as a one-way valve—closing tightly to keep stomach contents from rising. When the LES weakens or relaxes inappropriately, acid escapes into the esophagus. Several factors contribute to or trigger this malfunction:
- Dietary Triggers: Foods and drinks that relax the LES or increase acid production. Key culprits include:
- Spicy foods (chili peppers, hot sauces)
- Acidic foods (tomatoes, citrus fruits, vinegar-based dishes)
- Fatty or fried foods (slower digestion increases LES pressure)
- Caffeinated beverages (coffee, tea, soda, energy drinks)
- Alcohol (weakens LES muscle)
- Chocolate and peppermint
- Poor Eating Habits:
- Eating large or fatty meals
- Lying down or reclining soon after eating
- Late-night snacking
- Not chewing food thoroughly
- Obesity: Excess abdominal weight increases stomach pressure, driving acid into the esophagus.
- Hiatal Hernia: A structural abnormality where part of the stomach pushes up through the diaphragm, making acid reflux more likely.
- Pregnancy: Hormonal changes and pressure from the growing uterus elevate the risk of reflux, especially in the third trimester.
- Smoking: Damages LES muscle and increases stomach acid secretion.
- Certain Medications: Such as some asthma drugs, antihistamines, painkillers, sedatives, and antidepressants can relax the LES.
- Genetic and age-related factors: With age, the LES may naturally weaken, and some individuals may have a genetic predisposition to reflux or GERD.
Who is at Risk?
While acid reflux can affect anyone, certain populations have a higher risk:
- Those with obesity or significant abdominal weight
- Pregnant women
- Smokers
- People who consume diets high in fatty, spicy, or acidic foods
- Individuals with a family history of reflux or hiatal hernia
Common Symptoms of Acid Reflux
The symptoms of acid reflux can range from mild to severe, and may present differently depending on the individual. Recognizing these symptoms is key to seeking proper management:
- Heartburn: A burning sensation in the chest, usually after eating or at night
- Regurgitation: Sour or bitter-tasting acid backing up into the throat or mouth
- Difficulty swallowing (dysphagia): The feeling that food is stuck in your throat
- Chronic cough or throat irritation
- Hoarseness or sore throat
- Chest pain, especially when lying down
- Sensation of a lump in the throat (globus sensation)
- Worsening symptoms at night, causing sleep disturbances
If these symptoms occur more than twice a week, or if they are severe, chronic acid reflux or GERD is likely and medical consultation is recommended.
How Acid Reflux is Diagnosed
Diagnosis often begins with your doctor taking a detailed history of your symptoms and may involve physical examination. Depending on severity and persistence of symptoms, further investigations include:
- Trial of medication: Your doctor may prescribe antacids or acid-suppressing medicines. If symptoms improve, reflux is likely.
- Endoscopy: A thin tube with a camera is passed into your esophagus and stomach to look for inflammation or damage.
- pH monitoring: Measures acid levels in your esophagus over 24 hours to confirm reflux.
- Esophageal manometry: Assesses the muscle function of your esophagus and LES.
- Barium swallow X-ray: Evaluates swallowing and looks for anatomical issues.
Lifestyle Changes for Acid Reflux Relief
Most mild to moderate cases of acid reflux can be managed by simple lifestyle changes:
- Eat Smaller, More Frequent Meals: Helps prevent overwhelming the LES and stomach.
- Adjust Your Diet:
- Avoid offending foods and drinks (see above)
- Incorporate higher-fiber foods like vegetables, fruits, and whole grains
- Choose lean proteins—chicken, turkey, fish, eggs, beans
- Use lower fat foods and cooking methods (grilling, baking, steaming)
- Do Not Eat Before Bedtime: Leave at least 2–3 hours between your last meal/snack and lying down to sleep.
- Elevate the Head of Your Bed: Raise the head of the bed 6–8 inches or use a wedge pillow to reduce nighttime reflux.
- Lose Weight if Overweight or Obese: Even modest weight loss can significantly improve symptoms.
- Quit Smoking: Smoking cessation improves LES function and overall digestive health.
- Wear Loose Clothing: Tight belts and waistbands can increase stomach pressure and push acid upward.
- Stay Upright After Eating: Sitting or standing for at least 3 hours post-meal aids digestion.
Medical Treatments for Acid Reflux
If lifestyle adjustments are not enough, several medications and, in rare cases, surgery are available to control acid reflux and prevent complications:
- Antacids: Quickly neutralize stomach acid and relieve mild symptoms. Not suitable for long-term use as the primary therapy.
- H2 blockers: Reduce acid production (e.g., ranitidine, famotidine).
- Proton pump inhibitors (PPIs): Stronger acid reducers (e.g., omeprazole, lansoprazole, esomeprazole). PPIs are the mainstay for frequent symptoms or esophageal inflammation.
- Prokinetic agents: Help strengthen the LES and encourage stomach emptying. Used less commonly due to side effects.
- Surgery: Reserved for severe, treatment-resistant cases. The most common procedure is fundoplication, where the upper stomach is wrapped around the LES to reinforce its closure.
| Treatment | Primary Use | Benefits | Limitations |
|---|---|---|---|
| Antacids | Occasional, mild symptoms | Fast relief | Short duration; not for regular use |
| H2 Blockers | Frequent, mild-to-moderate symptoms | Longer acting than antacids | May lose effectiveness with prolonged use |
| PPIs | Frequent, moderate-to-severe symptoms | Best long-term acid suppression | Potential side effects with extended use |
| Prokinetics | Motility-related symptoms | Addresses delayed gastric emptying | Side effects limit usability |
| Surgery | Refractory or complicated GERD | May cure or dramatically reduce symptoms | Risks from surgery; not always successful |
Tips for Preventing Acid Reflux
Prevention is often the best defense against acid reflux. Simple steps to lower your risk include:
- Maintain regular, balanced meals rich in fiber, lean protein, and vegetables
- Stay hydrated (but avoid excessive fluids with meals)
- Avoid high-fat and high-sugar foods
- Exercise regularly—avoid strenuous activity soon after eating
- Recognize and avoid your personal food triggers
- Manage stress with relaxation techniques
- Regularly monitor weight
Possible Complications if Acid Reflux is Unmanaged
Persistent, untreated acid reflux can have serious consequences, including:
- Esophagitis: Inflammation or ulceration of the esophageal lining
- Esophageal strictures: Narrowing of the esophagus due to scar tissue
- Barrett’s esophagus: Precancerous changes in the esophageal cells, increasing the risk of esophageal cancer
- Chronic cough, asthma, or laryngitis: Acid can irritate the upper airways and lungs
Seek medical help urgently if you experience unexplained weight loss, difficulty swallowing, vomiting blood, or black/tarry stools.
Frequently Asked Questions (FAQs)
Q: What lifestyle changes help most with acid reflux?
A: Key strategies include eating smaller meals, avoiding trigger foods, not lying down after eating, elevating the head of your bed, losing excess weight, quitting smoking, and wearing loose clothing.
Q: When should I see a doctor about my heartburn?
A: If you have symptoms twice a week or more, experience trouble swallowing, persistent hoarseness, unexplained weight loss, blood in vomit or stool, or symptoms unresponsive to over-the-counter remedies, see a healthcare provider promptly.
Q: Are there any foods that help prevent or soothe reflux?
A: Foods likely to be less irritating include bananas, melons, oatmeal, whole grains, lean poultry, and non-citrus fruits. However, individual triggers vary—reintroduce foods cautiously to find what works for you.
Q: Is long-term use of acid reflux medications safe?
A: While medications such as PPIs are generally safe under medical supervision, prolonged use may carry risks including vitamin and mineral deficiencies or gut infections. Always use medication as directed by your doctor.
Q: Can acid reflux be cured?
A: Occasional reflux is normal and often resolves with lifestyle modifications. Chronic GERD, however, may require ongoing management. In rare cases, surgery may provide lasting relief.
This article aims to provide comprehensive educational resources on acid reflux for patients and the general public. For individualized advice and diagnosis, always consult a qualified healthcare provider.
References
- https://bgapc.com/common-causes-of-acid-reflux-and-how-to-manage-it/
- https://www.drsantosh.com.au/reflux
- https://www.albertahealthservices.ca/assets/info/nutrition/if-nfs-managing-acid-reflux.pdf
- https://my.clevelandclinic.org/health/diseases/17019-acid-reflux-gerd
- https://www.asge.org/docs/default-source/about-asge/newsroom/doc-gerd_infographic_final.pdf
- https://gi.org/topics/acid-reflux/
- https://www.mayoclinic.org/diseases-conditions/gerd/diagnosis-treatment/drc-20361959
- https://www.nhs.uk/conditions/heartburn-and-acid-reflux/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8754510/
Read full bio of Sneha Tete












