White Spot in the Eye: Causes, Symptoms, and Treatments
Learn what causes white spots in the eye, their symptoms, treatment options, and when to see a doctor for urgent eye health concerns.
White Spot in the Eye: Causes, Symptoms, Treatments, and More
Seeing a white spot in the eye can be concerning. While some causes are harmless and resolve quickly, others may signal a serious underlying condition requiring urgent medical care. The location, size, and associated symptoms are crucial for diagnosis and treatment. This article explores the various causes, symptoms, risk factors, and treatment options for white spots in the eye, as well as when you should seek immediate attention from an eye specialist.
What Is a White Spot in the Eye?
A white spot in the eye refers to a white area, patch, dot, or lesion that can appear on any visible part of the eye. Most often, these spots are noticed in the following areas:
- The clear outer layer (the cornea) covering the iris and pupil
- The sclera, or the white of the eye
- The pupil (the dark center) or the lens just behind it
The spot might be tiny, flat, raised, painless, or accompanied by other symptoms such as redness, pain, or vision changes. The potential causes are varied—some pose little risk, while others can quickly threaten your sight.
Causes of White Spots in the Eye
There are several conditions that may cause a white spot in the eye. Below are the main causes, grouped by where the white spot most commonly appears:
Corneal Ulcer
A corneal ulcer refers to an open sore on the cornea, the clear front surface of your eye. A corneal ulcer typically appears as a visible white or grayish spot on the cornea.
- Common Causes: Infections (bacterial, viral, fungal, or parasitic), eye injury, long-term contact lens wear, dry eye, or autoimmune diseases.
- Symptoms: Eye pain, redness, tearing, blurry vision, light sensitivity, and a sensation of something in the eye.
Corneal ulcers are considered an eye emergency and require prompt medical attention to avoid permanent vision loss.
Pinguecula
Pinguecula refers to a benign, yellowish-white raised bump or patch that appears on the conjunctiva—the clear membrane covering the sclera. This spot is usually near the nose or the side of the eye most exposed to sunlight.
- Risk Factors: UV light exposure, frequent irritation from wind or dust, and age.
- Symptoms: Typically painless, though it can cause a feeling of dryness or grittiness.
Pingueculae are non-cancerous and usually harmless, but they can sometimes progress into pterygium, which may affect vision if left unchecked.
Pterygium
Pterygium is a fleshy, wedge-like growth that may start as a pinguecula on the conjunctiva and eventually extend onto the cornea.
- Appearance: White, cream, or yellow growth on the inner or outer corner of the eye, moving towards the center.
- Symptoms: Blurred vision, eye irritation, foreign body sensation, and redness.
If the growth covers the cornea, it can cause astigmatism or significant vision problems, sometimes requiring surgery.
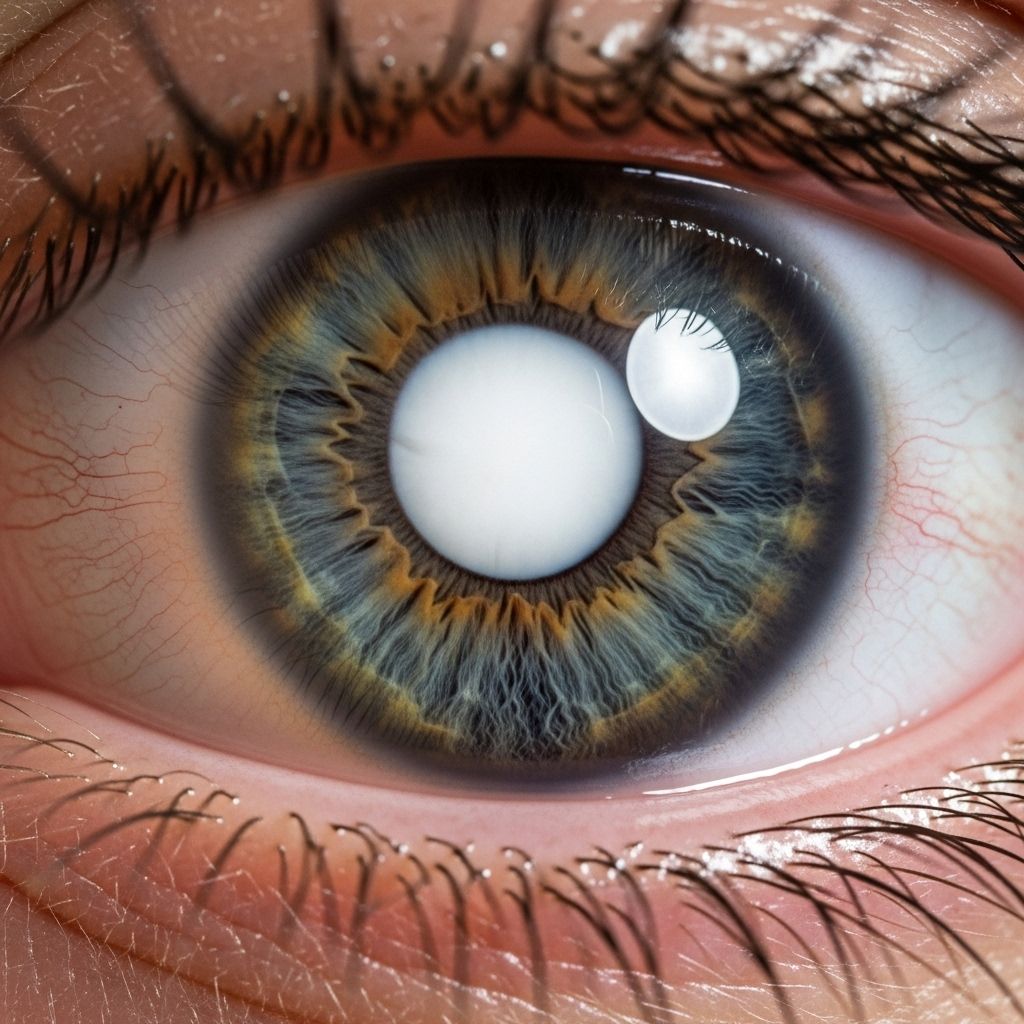
Cataracts
Cataracts cause clouding of the eye’s lens, which lies behind the pupil. In advanced cases, cataracts can make the pupil or lens appear milky white.
- Symptoms: Gradual, painless vision loss (becoming cloudy or foggy), glare, difficulty seeing at night, and double vision.
- Risk Groups: Most common in older adults, but congenital cataracts may occur in infants.
Cataracts do not usually cause painful symptoms, but if vision becomes severely impaired, surgery may be necessary.
Retinoblastoma
Retinoblastoma is a rare but serious cancer of the retina—usually affecting children. A common sign is a white reflection or white spot (known as leukocoria) visible in the pupil, often picked up in photographs.
- Symptoms: White spot in the pupil, eye redness, crossing or misalignment of the eyes, vision loss.
- Urgency: Retinoblastoma is a medical emergency. Early detection and treatment are crucial for preserving vision and life.
Corneal Dystrophies
Corneal dystrophies are a group of inherited disorders where cloudy material accumulates in the cornea, causing white or grayish opacity.
- Symptoms: Mild to moderate vision impairment, recurrent discomfort, glare, and halos around lights.
- Progression: Some remain stable, while others may worsen over time and require surgery (including corneal transplant).
Toxocariasis
Ocular toxocariasis is an eye infection caused by the Toxocara parasite, more common in children exposed to contaminated soil or animal feces.
- Symptoms: White spots in the eye, redness, eye pain, swelling, and possible decreased vision.
- Complications: Untreated, it can cause retinal inflammation or permanent vision loss.
| Condition | Location / Appearance | Additional Symptoms |
|---|---|---|
| Corneal Ulcer | White spot on cornea | Pain, redness, vision changes |
| Pinguecula | Yellow-white spot on sclera | Dryness, irritation |
| Pterygium | Fleshy growth crossing onto cornea | Blurriness, discomfort |
| Cataract | White pupil (advanced stage) | Painless visual clouding |
| Retinoblastoma | White pupil (leukocoria) | Redness, vision loss, squint |
| Corneal Dystrophy | Cloudy/white areas on cornea | Glare, halos, mild discomfort |
| Toxocariasis | White spots in retina / cornea | Pain, swelling, vision loss |
Symptoms Associated with White Spots in the Eye
The symptoms you experience depend on the underlying cause. Watch for the following symptoms, and take note if they appear rapidly or worsen:
- Eye pain or discomfort
- Sensitivity to light (photophobia)
- Redness or swelling
- Blurred or reduced vision
- Discharge from the eye
- Sensation of something in the eye
- Visible changes in the appearance of the cornea or pupil
If a white spot is accompanied by sudden vision loss, intense pain, redness, or swelling, seek immediate medical evaluation.
Risk Factors for White Spots in the Eye
- Wearing contact lenses (especially with improper hygiene or overnight use)
- Exposure to sunlight/UV rays without protective eyewear
- Older age (for cataracts or degenerative conditions)
- History of eye injuries or surgery
- Immune system disorders
- Poor hygiene, especially in children playing in contaminated areas
Diagnosis: How Doctors Find the Cause
If you or your child develops a white spot in the eye, an eye doctor (ophthalmologist or optometrist) will use the following steps to determine the cause:
- Thorough medical history, including onset and progression of symptoms
- Physical examination with a slit lamp (microscope) for detailed eye inspection
- Vision testing, checking for visual acuity and field loss
- Fluorescein dye to highlight ulcers or injuries on the cornea
- Pupil dilation to examine the retina and inner parts of the eye
- Blood tests, eye cultures, or imaging (rare but possible in complex cases)
Early diagnosis is key to preventing complications or permanent vision loss.
Treatment Options for White Spots in the Eye
Treatment depends on the underlying cause. Some causes are mild and may resolve with conservative management, while others require urgent or ongoing care. Here is an overview of the most common treatment options:
Eye Drops
- Lubricating eye drops: Reduce dryness and irritation, especially for pinguecula or mild pterygium.
- Steroid or anti-inflammatory drops: Used for inflammation or autoimmune conditions affecting the cornea or conjunctiva.
Antimicrobial Medications
- Antibiotics: For bacterial corneal ulcers or conjunctivitis.
- Antivirals: For viral infections such as herpes simplex, varicella zoster, or cytomegalovirus.
- Antifungals or antiparasitics: Used when fungal or parasitic infection is identified.
Timely antibiotics or antivirals can often resolve infections and prevent permanent damage.
Cryotherapy
Cryotherapy uses extreme cold to destroy abnormal tissues or small tumors. It is sometimes utilized in treating retinoblastoma and surface cancers of the eye, as well as abnormal blood vessel growth in rare retinal diseases.
Laser Therapy
Laser therapy may be employed to shrink or destroy tumors (such as retinoblastoma), treat blood vessel abnormalities, or remove unwanted tissue growth (such as pterygium).
Surgical Treatment
- Corneal transplant (keratoplasty): For severe corneal damage (from ulcer, dystrophy, or injury), the damaged tissue is replaced with a donor cornea.
- Cataract surgery: Involves removing the clouded lens and replacing it with an artificial intraocular lens.
- Removal of growths or tumors: Surface growths like pterygium, pinguecula, or small tumors can be excised microsurgically if they threaten vision or cause significant discomfort.
Prevention Tips
Some white spots can’t be prevented, but you can reduce your risk with the following strategies:
- Practice good contact lens hygiene: wash hands before handling lenses, never sleep in lenses unless prescribed.
- Wear sunglasses or UV-blocking safety glasses outdoors.
- Avoid eye injuries by using protective eyewear during risky activities.
- Prevent infections by not touching or rubbing your eyes with unwashed hands.
- Have regular eye exams, especially if you have risk factors for cataracts or corneal diseases.
- Keep children away from potentially contaminated soil or animal feces to prevent parasitic infections.
When to See an Eye Doctor
Seek emergency care if you notice:
- Sudden onset of a white spot with pain, redness, or severe vision loss
- Growing or spreading white spot
- Eye trauma, especially if chemicals or a foreign object are involved
For less urgent symptoms or if a white spot has been present but isn’t worsening, arrange a routine visit with an ophthalmologist. Don’t ignore new or rapidly changing eye symptoms—early intervention can preserve vision.
Frequently Asked Questions (FAQ)
What should I do if I notice a white spot in my child’s eye?
If you notice a persistent or newly appearing white spot—especially in your child’s pupil—schedule an eye exam promptly. In infants or young children, a white pupil (leukocoria) can signal serious disease like retinoblastoma.
Is a white spot in the eye always serious?
No, not always. Some white spots, such as pinguecula or small pterygium, are harmless. However, any spot that appears suddenly, is associated with pain, or affects vision should be medically evaluated.
Do white spots in the eye go away on their own?
Some mild causes (such as pinguecula or minor irritation) may resolve without treatment. Infections or growths generally require medical intervention. Do not delay care if symptoms worsen.
Can cataracts be prevented?
Age-related cataracts cannot always be prevented, but wearing UV-protective eyewear and managing systemic diseases like diabetes can help lower risk.
How long does it take for a corneal ulcer to heal?
With prompt treatment, minor ulcers may begin to heal within days; severe or complicated ulcers may take weeks or require surgery. Quick treatment is essential to prevent vision loss.
Key Takeaways
- White spots in the eye can have benign or serious causes.
- Early diagnosis significantly improves the outcome for serious conditions like corneal ulcers or retinoblastoma.
- Practice good eye hygiene, wear protective eyewear, and schedule regular eye exams to safeguard your eye health.
References
- https://www.tuasaude.com/en/white-spots-on-the-eye/
- https://resources.healthgrades.com/right-care/eye-health/white-spot-on-eye
- https://www.healthline.com/health/eye-health/white-spot-in-eye
- https://my.clevelandclinic.org/health/diseases/23443-pinguecula
- https://www.milaneyecenter.com/eye-conditions/corneal-ulcer-white-spot-on-eye/
- https://my.clevelandclinic.org/health/diseases/22524-corneal-ulcer
- https://www.wheatoneye.com/eye-conditions/cornea-external-disease/pterygium-pinguecula/
- https://brobergeyecare.com/pinguecula/
Read full bio of Sneha Tete












