What to Avoid If You Have Mitral Valve Prolapse
Managing mitral valve prolapse: lifestyle cautions, dietary tips, and risk avoidance for healthier heart outcomes.
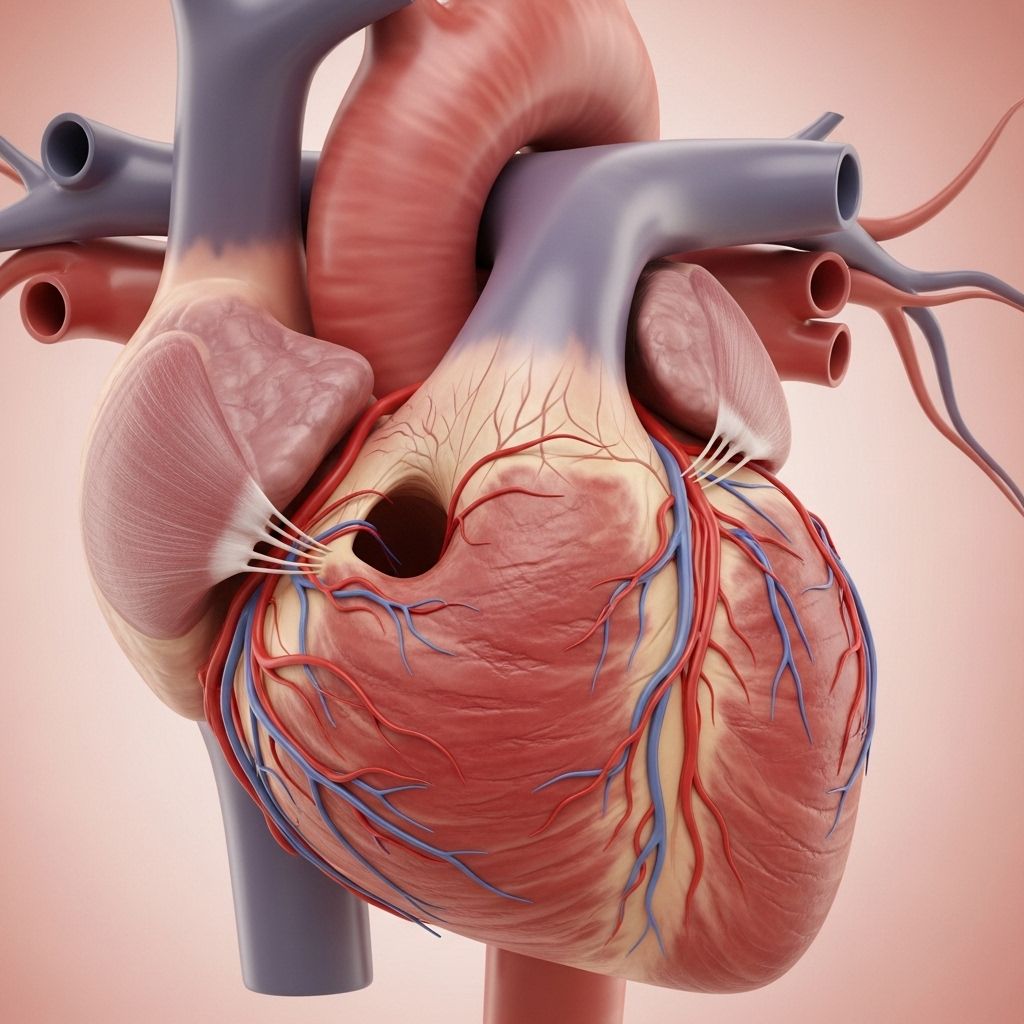
Mitral valve prolapse (MVP) is a common heart condition in which the mitral valve’s leaflets bulge (prolapse) into the left atrium during contraction, sometimes allowing blood to leak backward—a process called regurgitation. While often benign, MVP can cause symptoms and complications that require specific lifestyle modifications. Understanding what to avoid can help minimize risks and enhance quality of life.
Overview: Mitral Valve Prolapse
MVP affects the mitral valve separating the left heart chambers. Most individuals with MVP are symptom-free, but some experience chest pain, palpitations, fatigue, or anxiety. In rare cases, severe mitral regurgitation can lead to significant complications like arrhythmias, stroke, or heart failure.
- Common Symptoms: Palpitations, chest discomfort, dizziness, fatigue, occasional shortness of breath.
- Risk Factors: Family history, connective tissue disorders (Marfan syndrome), female sex, scoliosis, adult polycystic kidney disease.
Dietary Choices to Avoid
Diet plays a significant role in heart health. For those with MVP, avoiding foods and substances that can trigger symptoms or aggravate heart workload is advised.
Limit Caffeine
Caffeine, found in coffee, tea, sodas, energy drinks, and chocolate, can increase heart rate and provoke palpitations or arrhythmias. Individuals with MVP-sensitive symptoms often benefit from limiting or avoiding caffeine.
- Coffee and espresso-based beverages
- Cola, energy drinks
- Chocolate and certain teas
Avoid Excess Sugar and Processed Foods
High sugar intake can exacerbate energy fluctuations and increase heart stress. Processed foods, which may contain preservatives, unhealthy fats, and additives, should be minimized.
- Sugary cereals, pastries, cakes
- Sodas and sweetened beverages
- Packaged snacks and canned goods with high salt/sugar content
Reduce Sodium Intake
High sodium diets promote fluid retention and may increase blood pressure, which can stress the heart and worsen symptoms. Monitor labels for sodium content.
- Salted snacks (pretzels, chips)
- Canned soups
- Processed meats (sausages, deli meats)
Limit Alcohol
Alcohol can precipitate arrhythmias and cause dehydration, which may intensify MVP symptoms. Best practice is moderation or avoidance, especially if symptoms worsen after consumption.
- Wine, beer, spirits
- Cocktails with added caffeine/sugar
Watch Out for Unhealthy Fats
Trans fats and saturated fats, common in fried foods, pastries, and certain processed items, can contribute to cardiovascular problems. Focus on heart-healthy fats instead.
- Fried fast foods
- Margarine and some baked goods
- Cream-heavy desserts
Activities, Habits, and Substances to Avoid
Managing MVP goes beyond diet—certain activities and habits may pose additional risk or worsen symptoms.
Dehydration and Overexertion
Being well-hydrated helps maintain healthy blood volume and heart function. Avoid excessive physical activity that leads to dehydration, and monitor exercise intensity.
- Intense, prolonged workouts without adequate fluids
- Saunas/hot yoga that cause excessive sweating
Stimulant Medications and Drugs
Some over-the-counter medicines (decongestants, diet pills) and recreational drugs (amphetamines, cocaine) can trigger arrhythmias, palpitations, and dangerous increases in heart rate/blood pressure. Always consult your physician before using any new medication.
- Nasal decongestants (pseudoephedrine)
- Diet pills containing stimulants
- Illicit stimulants (methamphetamine, cocaine)
Excessive Stress and Poor Sleep
Stress and lack of restful sleep may elevate blood pressure and heart rate, worsening symptoms. Stress management and regular sleep routines are essential.
Dental and Surgical Procedures: Precautions
Although MVP rarely leads to endocarditis (infection of the heart valve), preventative antibiotics may be recommended for certain individuals during dental or surgical procedures. Always inform your dentist or surgeon about your MVP diagnosis.
- Discuss antibiotic need prior to dental work.
- Never skip prescribed antibiotics if advised.
Medication Risks and Management
Some medications can aggravate MVP symptoms or interact with conditions associated with the disorder. Coordination with your healthcare provider is vital for medication safety.
- Avoid self-medicating with stimulants.
- Review all current drugs with your cardiologist, including supplements and herbal remedies.
- Use blood thinners only as prescribed (for those with arrhythmias or elevated stroke risk).
When to Seek Medical Care
Not everyone with MVP requires treatment, but symptoms may dictate closer medical monitoring or intervention. Severe mitral regurgitation or the development of arrhythmias may require medical or surgical management.
- Notify your doctor if new or worsening symptoms occur.
- Seek immediate help for chest pain, severe shortness of breath, fainting, or stroke symptoms (sudden numbness, vision changes, difficulty speaking).
Lifestyle Tips for MVP Management
In addition to avoiding certain foods and substances, adopting positive lifestyle behaviors can help reduce symptom frequency and severity.
- Regular Exercise: Moderate physical activity can improve cardiovascular conditioning but should be tailored to your ability and doctor’s recommendations.
- Stress Reduction: Incorporate stress-management techniques like yoga, meditation, or breathing exercises.
- Healthy Diet: Prioritize fresh vegetables, fruits, whole grains, lean proteins, and heart-healthy fats.
- Hydration: Drink adequate water daily.
- Monitoring: Keep track of symptoms and share them with your healthcare team.
Complications Linked to Mitral Valve Prolapse
While most with MVP live normal lives, monitor for the following potential complications:
| Complication | Symptoms | Prevention/Management |
|---|---|---|
| Mitral Regurgitation | Shortness of breath, fatigue, palpitations | Follow-up imaging, medications, surgery (severe cases) |
| Arrhythmias | Rapid heartbeat, dizziness, fainting | Medications, ablation, lifestyle changes |
| Endocarditis | Fever, chills, heart murmurs | Antibiotics before certain procedures |
| Stroke | Sudden weakness/numbness, speech or vision changes | Blood thinners (if indicated), manage arrhythmias |
Frequently Asked Questions (FAQs)
Q: Is mitral valve prolapse life-threatening?
A: For most people, MVP is benign and not life-threatening. Serious complications are rare but can occur when mitral regurgitation becomes severe or arrhythmias develop.
Q: Should people with MVP avoid exercise?
A: Not necessarily. Moderate exercise is usually safe and healthy. Avoid extreme exertion or dehydration; always discuss with your cardiologist.
Q: Do I need antibiotic prophylaxis for dental procedures?
A: Only select individuals—those with MVP plus certain complications—need antibiotics for dental/surgical work. Confirm with your cardiologist.
Q: Can I drink coffee with MVP?
A: If caffeine triggers palpitations or other symptoms, avoid or limit intake. Select decaffeinated options as appropriate.
Q: Are over-the-counter cold medicines safe?
A: Some contain stimulants that may trigger arrhythmias. Always consult your healthcare provider before taking OTC products.
Practical Tips for Living Well with MVP
- Keep regular checkups and report new symptoms promptly.
- Choose a balanced, low-sodium, heart-smart diet.
- Stay hydrated and limit stimulants like caffeine or certain medications.
- Practice stress-reduction and maintain good sleep hygiene.
- Involve your healthcare provider when contemplating dental or surgical procedures.
Mitral valve prolapse is often a manageable condition, with many people experiencing few or no disruptive symptoms. By understanding what to avoid—dietary triggers, certain medications, physical overexertion, and high-stress situations—and by following lifestyle recommendations, most individuals can live actively and safely while minimizing risks of MVP-related complications.
References
- https://medlineplus.gov/ency/article/000180.htm
- https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/problem-mitral-valve-prolapse
- https://www.healthline.com/health/mitral-valve-prolapse
- https://www.health.harvard.edu/heart-health/mitral-valve-prolapse-a-to-z
- https://www.healthline.com/health/mitral-valve-prolapse-symptoms
- https://www.ncbi.nlm.nih.gov/books/NBK470288/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5757046/
Read full bio of Sneha Tete












