Understanding Heart Block: Causes, Types, Symptoms, and Treatments
Get a comprehensive overview of heart block, including its causes, symptoms, types, risk factors, and essential treatments.
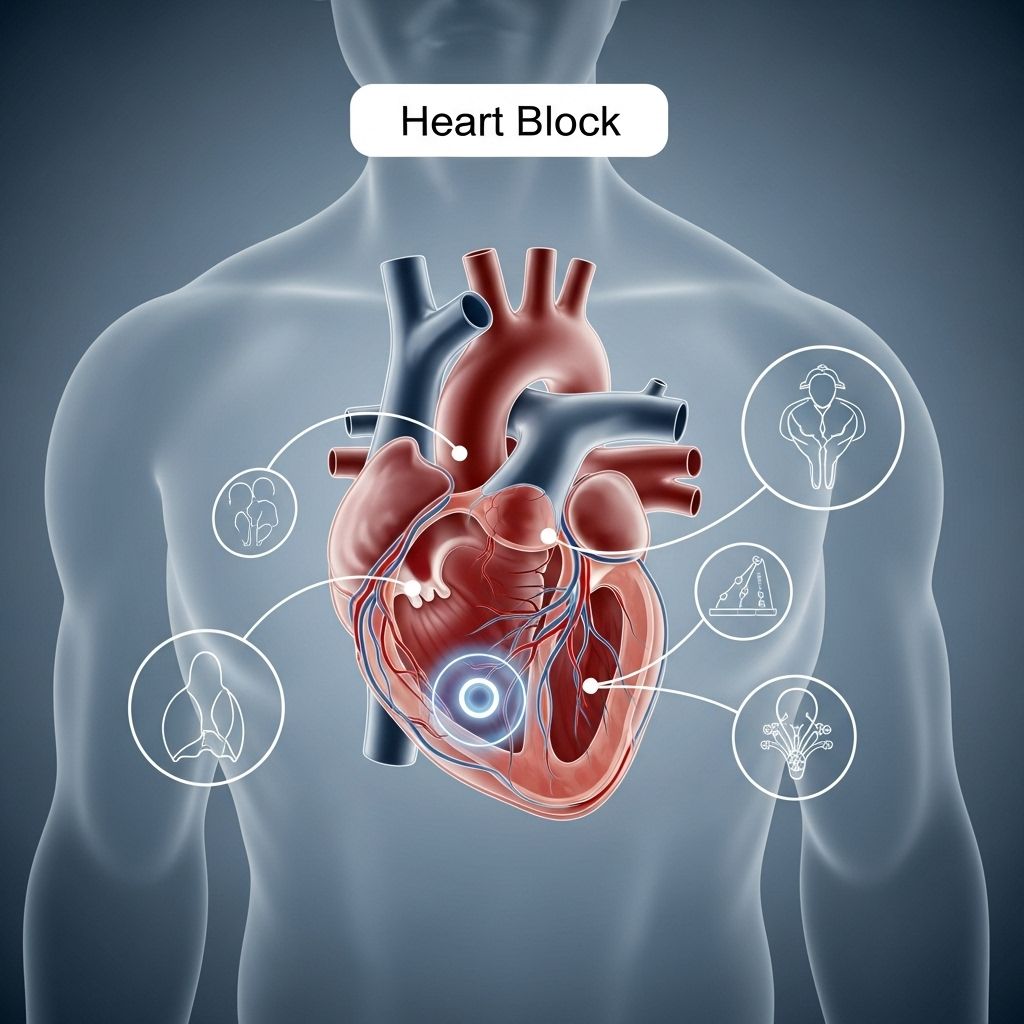
What Is Heart Block?
Heart block, also known as an atrioventricular (AV) block, is a disorder affecting the heart’s electrical conduction system. This condition disrupts or slows the signal that controls the heartbeat, leading to irregular, slow, or even missed heartbeats. In severe instances, heart block can cause fainting, chest pain, or cardiac arrest, requiring immediate medical attention.
How Does a Healthy Heart Beat?
The heart’s rhythm is governed by intricate electrical signals. These begin in the sinoatrial (SA) node, the heart’s natural pacemaker, located in the upper right chamber (right atrium). The signals travel across the atria, causing them to contract and pump blood into the lower chambers (ventricles). They then reach the atrioventricular (AV) node, which relays the impulse into the ventricles, prompting them to contract and distribute blood to the lungs and rest of the body. This perfectly timed sequence ensures efficient blood circulation.
What Happens in Heart Block?
In heart block, the electrical impulses may be delayed, slowed, or completely blocked as they move from the atria to the ventricles through the AV node. The result is a disruption of the normal rhythm, commonly resulting in a slower heart rate (bradycardia) and sometimes skipped or missed beats. The severity of symptoms varies according to the type and degree of heart block present.
Types of Heart Block
Heart block is categorized based on how much the electrical signal transmission from the atria to the ventricles is impaired. There are three primary types:
- First-Degree Heart Block: The mildest form. Electrical impulses are delayed but do reach the ventricles. It often causes no symptoms and is usually discovered incidentally during routine testing.
- Second-Degree Heart Block: Some impulses fail to reach the ventricles. This leads to dropped or skipped heartbeats, causing an irregular rhythm. It is further divided into two subtypes:
- Mobitz Type I (Wenckebach): The signal slows down more with each beat until one beat is missed.
- Mobitz Type II: Occasional and unpredictable skipped beats, often more serious and likely to progress to third-degree block.
- Third-Degree (Complete) Heart Block: The most severe form. No electrical signals reach the ventricles from the atria. The heart generates its own impulses in the ventricles, leading to a slow, unreliable heart rhythm, which may result in collapse or sudden cardiac arrest if not treated promptly.
Table: Heart Block Types and Characteristics
| Type | Electrical Impulse Effect | Symptoms | Severity |
|---|---|---|---|
| First-degree | Delayed | Often none | Mild |
| Second-degree (Mobitz I) | Progressively delayed, then dropped beat | May include dizziness, fainting | Moderate |
| Second-degree (Mobitz II) | Sudden dropped beats | Irregular rhythm, symptoms more likely | Serious |
| Third-degree | Complete block | Severe, often life-threatening | Most severe |
Symptoms of Heart Block
The symptoms of heart block depend on its type and severity. Some individuals, especially those with first-degree block, may not notice any issues. Others may experience:
- Dizziness and Lightheadedness: Especially with activity
- Fainting (Syncope): Sudden loss of consciousness can occur, particularly in severe blocks
- Fatigue: Ongoing tiredness or weakness
- Shortness of Breath: Difficulty breathing even with mild exertion
- Chest Pain: Tightness or discomfort
- Palpitations: Noticing irregular or skipped beats
- Slow Pulse: Often under 60 beats per minute (bradycardia)
Severe or sudden symptoms may indicate complete heart block and require immediate medical attention.
Causes of Heart Block
Heart block can develop due to a wide variety of factors affecting the heart’s electrical system. Causes include:
- Age-Related Degeneration: The most common cause, especially in older adults, as the heart’s electrical pathways break down or lose function over time.
- Heart Attack (Myocardial Infarction): Damage to the heart muscle can disrupt the electrical circuit.
- Heart Conditions: Other diseases such as coronary artery disease, cardiomyopathy, or heart failure.
- Congenital Heart Block: Present at birth, often linked to autoimmune diseases in the mother or structural heart defects.
- Heart Surgery: Scarring from previous surgeries can interrupt the conduction pathways.
- Medications: Drugs that slow the heart’s electrical system, including beta-blockers and calcium channel blockers.
- Other Health Conditions: Such as Lyme disease, diabetes, high blood pressure, or electrolyte imbalances (such as abnormal potassium or calcium levels).
- Infections: Like myocarditis or endocarditis, which can inflame or damage heart tissue.
Risk Factors
Certain factors increase the likelihood of developing heart block:
- Advanced age
- Existing heart disease or history of heart attack
- Congenital heart disease or genetic predisposition
- History of heart surgery
- Exposure to certain medications or toxins
- Autoimmune conditions (especially in pregnant women)
How Is Heart Block Diagnosed?
Diagnosing heart block involves identifying symptoms and confirming disrupted electrical conduction through medical testing. Common methods include:
- Electrocardiogram (ECG or EKG): The primary diagnostic test. It records the heart’s electrical activity, revealing the type and degree of block.
- Holter Monitor: A wearable device that records heart rhythms over 24–48 hours, useful for detecting intermittent episodes.
- Event Monitor: Similar to a Holter monitor, but used for longer periods when symptoms are infrequent.
- Echocardiogram: Ultrasound imaging examines heart structure and function to rule out other causes.
- Electrophysiological Testing: Specialized testing to assess the heart’s electrical system for more detailed information.
- Blood Tests: To check for causes like thyroid abnormalities or electrolyte imbalances.
Treatment Options for Heart Block
The treatment of heart block depends on its severity and underlying cause. Options range from observation to advanced interventions:
- Lifestyle Modifications & Observation: Mild first-degree block rarely requires active treatment but may be monitored regularly.
- Medication Review: Adjusting or discontinuing drugs that may cause or worsen the block, under medical guidance.
- Treatment of Underlying Causes: Correcting electrolyte imbalances, managing infections, or addressing other heart conditions.
- Pacemaker Installation: The most common treatment for advanced heart block. A pacemaker is a small device implanted under the skin to maintain a regular heart rhythm by delivering electrical impulses directly to the heart.
- Emergency Care: Acute heart block causing collapse or cardiac arrest needs immediate hospitalization and stabilization—often requiring emergency pacing, intravenous medications, and intensive monitoring.
Complications and Outlook
When diagnosed and treated promptly, most people with heart block, even those with severe forms, can lead normal, active lives. However, if untreated, heart block—especially third-degree block—can be life-threatening.
- Untreated Complete Heart Block: Can cause dangerously slow heart rate, impaired blood flow to brain and organs, and sudden cardiac arrest.
- With a Pacemaker: Most people can expect improved symptoms, normal activity, and increased survival.
- Ongoing Risks: Even treated, individuals may remain at higher risk for heart failure or other cardiac events, making regular cardiology follow-up essential.
Living with Heart Block or a Pacemaker
A diagnosis of heart block may require lifestyle adjustments and long-term medical collaboration:
- Regular check-ups with a cardiologist
- Adhering to prescribed medication regimens
- Reporting any new or worsening symptoms promptly
- Staying active within advised limits; pace yourself and avoid overexertion
- Understanding your pacemaker, if you have one—learning about device care and when to seek help
Prevention Tips
While some causes of heart block are unavoidable, especially age-related degeneration, many are preventable or manageable:
- Control high blood pressure, diabetes, and other chronic conditions
- Avoid excessive alcohol and recreational drug use
- Take medications only as directed, and inform your doctor about all drugs and supplements
- Address infections and other health issues quickly
Frequently Asked Questions (FAQs)
Q: How is heart block different from a heart attack?
A: Heart block affects the heart’s electrical system, disrupting rhythm. A heart attack involves blocked blood flow to the muscle, causing tissue damage. Heart attacks can sometimes trigger heart block, but they are different conditions.
Q: Can children get heart block?
A: Yes. Children can develop congenital heart block due to genetic heart defects or exposure during pregnancy to certain maternal conditions, such as autoimmune diseases.
Q: What are the signs of worsening heart block?
A: Symptoms like fainting, severe dizziness, chest pain, shortness of breath, and extreme fatigue may signal worsening heart block or complete block—call for emergency care immediately if these occur.
Q: How long does a pacemaker last?
A: Most modern pacemakers work effectively for 5–15 years before the battery or device must be replaced. Regular follow-up appointments help ensure optimal device function.
Q: Can heart block go away on its own?
A: Some temporary heart blocks, such as those caused by infections or medication effects, may resolve when the underlying issue is addressed. However, chronic or severe heart block rarely improves without intervention.
When to Seek Medical Help
Contact a healthcare provider if you experience symptoms of heart block, especially fainting, persistent dizziness, palpitations, chest pain, or unexplained fatigue. Seek emergency care if symptoms are severe or sudden, as these could signal a complete heart block or cardiac arrest.
Key Points to Remember
- Heart block disrupts the heart’s normal rhythm by slowing or stopping electrical signals between chambers.
- The condition varies in severity, with third-degree (complete) block being most dangerous and potentially fatal without prompt treatment.
- Symptoms range from mild or none to severe fainting, chest pain, and even cardiac arrest.
- Diagnosis relies on ECG and, if needed, more specialized testing.
- Pacemakers, medication management, and treatment of underlying causes can restore normal rhythm and quality of life.
References
- https://www.medicalnewstoday.com/articles/180986
- https://www.healthline.com/health/heart-disease/complete-heart-block
- https://www.heartandstroke.ca/heart-disease/conditions/heart-block
- https://my.clevelandclinic.org/health/diseases/17056-heart-block
- https://www.medicalnewstoday.com/articles/right-bundle-branch-block
- https://www.cedars-sinai.org/newsroom/healthline-therapy-vs-antidepressants–which-is-best-for-people-with-heart-disease/
- https://www.healthline.com/health/video/heart-health
- https://www.uc.edu/news/articles/legacy/healthnews/2006/12/h4100.html
Read full bio of medha deb












