What Does a Diverticulitis Attack Feel Like? Symptoms, Triggers, and Recovery
Understanding the pain, warning signs, psychological effects, and recovery process of diverticulitis for better digestive health.
What Does a Diverticulitis Attack Feel Like?
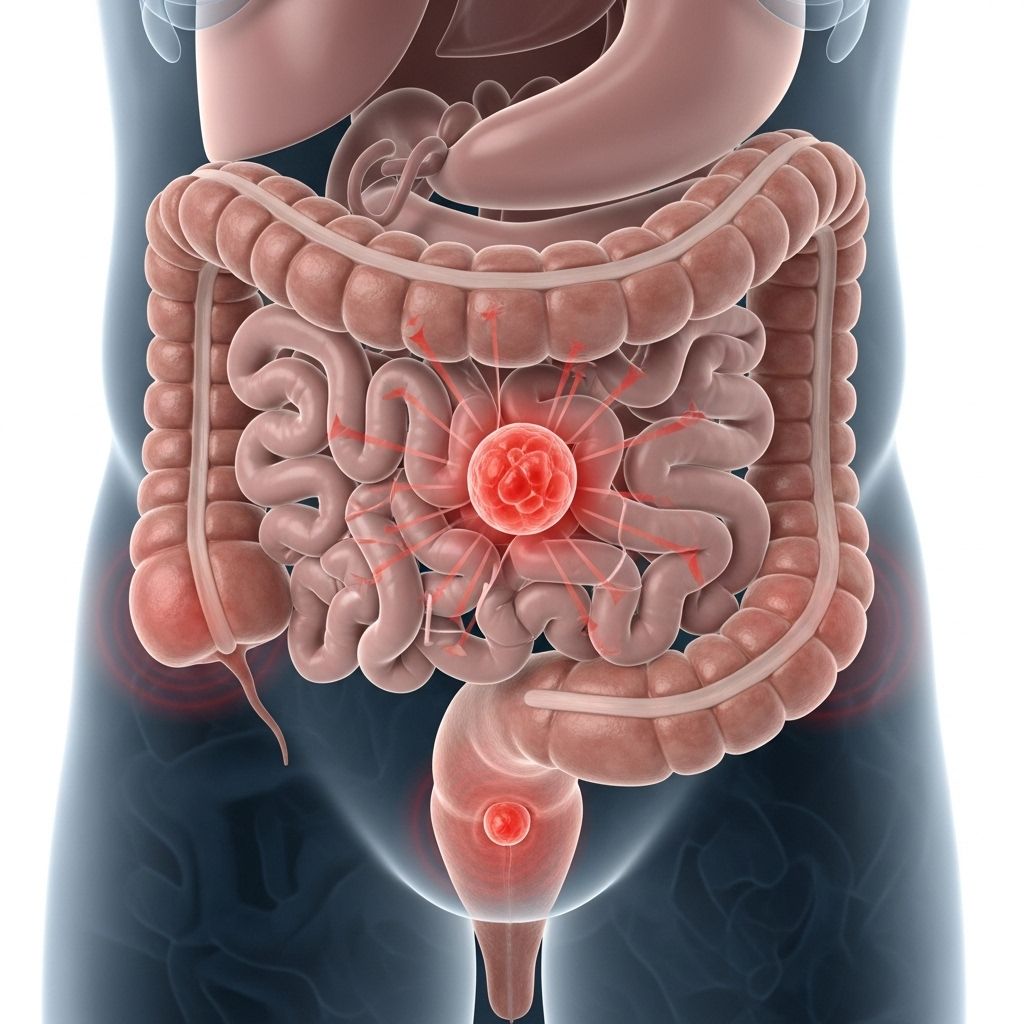
Diverticulitis occurs when small bulging pouches (diverticula) form in the walls of the colon and become inflamed or infected. The sensations during a diverticulitis attack can range from mild discomfort to severe, debilitating pain, with symptoms that may linger or intensify and impact a person’s quality of life in both the short and long term.
What Is Diverticulitis?
Diverticulitis is an inflammatory condition resulting from infected or irritated diverticula—small pouches formed due to weaknesses in the colon wall. While many people develop these pouches (a condition called diverticulosis) in their lifetime, diverticulitis occurs when one or more become inflamed, sometimes leading to distressing symptoms and, in rare instances, serious complications.
- Typically associated with aging, low-fiber diets, obesity, and sedentary lifestyle.
- More than half of people who experience one diverticulitis attack are likely to have a recurrence.
- Pouches can exist without symptoms, only causing issues once inflamed or infected.
How Does a Diverticulitis Attack Feel?
A diverticulitis attack often strikes suddenly, with pain being the hallmark symptom. Many patients describe the pain as steady, sharp, and sometimes excruciating—so significant that everyday activities can be disrupted.
- Most frequently felt in the lower left abdomen, though it can occur elsewhere.
- Pain may be constant or worsen with movement or pressure.
- The intensity ranges from mild to severe, sometimes requiring urgent medical intervention.
- Other physical sensations:
- Bloating and abdominal fullness.
- Diarrhea or constipation – changes in bowel habits are common.
- Nausea and vomiting, especially if the attack is severe.
Common Symptoms of a Diverticulitis Attack
| Symptom | Description & Frequency |
|---|---|
| Abdominal pain | Sudden, constant, usually lower left side; most prominent symptom. |
| Bloating/cramping | Feeling of fullness, abdominal distension. |
| Fever | Low-grade or persistent; may indicate infection. |
| Nausea/vomiting | Frequent in moderate or severe attacks. |
| Changes in stool | Diarrhea (up to 25%), constipation (up to 50%), or incomplete evacuation. |
| Loss of appetite | Due to discomfort and ongoing pain. |
| Urinary issues | Urgency, frequency, or discomfort; occurs in ~10–15% of cases. |
| Bloody stools | Less common; seek medical attention if present. |
When to Seek Medical Attention
Although mild cases may resolve on their own, medical evaluation is crucial if:
- Pain is increasing or not improving within a few days.
- You develop a fever or persistent nausea and vomiting.
- Symptoms include bloody stools, severe bloating, or inability to pass gas/stool.
- You feel very unwell, weak, or unable to eat/drink.
Timely diagnosis and treatment can help prevent complications, such as abscesses, perforation, or peritonitis.
Long-Term Psychological and Physical Impact
The consequences of a diverticulitis attack can last beyond the initial flare, affecting both physical and psychological well-being:
- Many patients report ongoing abdominal discomfort, bloating, and stool changes even after recovery.
- Persistent symptoms: Incomplete stool evacuation, watery stools.
- Heightened anxiety and fear about future attacks or the unpredictability of symptoms.
- Social withdrawal and reluctance to travel due to fear of a recurrence or stigma.
- Feelings of depression and isolation—especially if symptoms linger long term.
Recent research has identified the need for doctors to pay close attention to these quality-of-life effects and to use tools or questionnaires to better assess patient experience after diverticulitis.
Causes and Risk Factors of Diverticulitis
- Diverticulosis is the root condition—pouches formed due to pressure on weak colon sections.
- Risk factors for inflammation/infection include:
- Low-fiber diet, leading to harder stools and increased colon pressure.
- Aging, with high prevalence in adults over 50.
- Obesity and sedentary lifestyle.
- Previous diverticulitis flare-ups.
- Smoking and some medications.
Complications of Diverticulitis
Although most attacks are uncomplicated, a small subset may develop serious complications:
- Abscess: Localized pus collection requiring drainage.
- Perforation: Tear in the colon wall, leading to peritonitis (potentially life-threatening).
- Fistula: Abnormal communication between colon and organs like the bladder.
- Obstruction: Blockage due to swelling or scar tissue.
How Is Diverticulitis Diagnosed?
A healthcare provider evaluates symptoms, medical history, and may order:
- Physical exam, focusing on abdominal tenderness.
- Blood tests to check for infection/inflammation.
- CT scan for confirmation and assessment of severity/complications.
Treatment Options for Diverticulitis
Uncomplicated Diverticulitis
- Treated at home with prescribed oral antibiotics.
- Bowel rest via clear liquid or low-fiber diet (10 to 15 grams per day)—allowing inflammation to subside.
- Pain management as needed; typically patients feel improvement in ~3 days.
- Gradual return to regular diet once symptoms improve.
Severe or Complicated Diverticulitis
- Hospitalization for intravenous antibiotics.
- Potential need for surgical intervention in case of perforation, abscess, or ongoing obstruction.
- Hospital admission more likely for those over 65 or with chronic medical conditions.
Living with Diverticulitis: Coping Strategies and Lifestyle Adjustments
Managing Flare-Ups
- Monitor symptoms closely and consult a doctor if they worsen or linger.
- Maintain hydration—especially if experiencing vomiting/diarrhea.
- Follow dietary advice: temporarily eat clear liquids (broth, gelatin, water) then slowly introduce low-fiber foods.
- Use medications as instructed; do not take any without doctor advice.
Preventing Future Attacks
- Increase dietary fiber after initial recovery (whole grains, fruits, vegetables).
- Exercise regularly; maintain a healthy BMI.
- Avoid smoking and manage chronic health conditions.
- Stay aware of triggers and learn personal warning signs.
Addressing the Emotional Impact
- Seek support from healthcare providers, counselors, or support groups if you experience fear, anxiety, or isolation.
- Communicate openly about ongoing symptoms, especially those affecting daily life or mental health.
- Keep a log or diary of attacks to help track patterns and triggers.
Frequently Asked Questions (FAQs)
- Q: What triggers a diverticulitis attack?
A: Common triggers include low-fiber diets, dehydration, aging, obesity, physical inactivity, and sometimes certain medications. - Q: Should I avoid all seeds, nuts, or popcorn?
A: Despite prior medical advice, most studies show these foods aren’t linked to attacks for most patients; always follow your doctor’s recommendations. - Q: How soon should I see a doctor if I suspect diverticulitis?
A: Seek medical care if pain is severe, persistent, or accompanied by fever, vomiting, or blood in the stool. - Q: Can diverticulitis be permanently cured?
A: While attacks can be treated, the underlying diverticula remain; lifestyle changes help manage recurrences. Surgery may be an option for severe or frequent attacks. - Q: Will symptoms always be the same with each episode?
A: No, symptoms and severity can vary significantly between attacks and individuals. - Q: How long does it take to recover from a typical attack?
A: Most uncomplicated cases improve within a few days of antibiotics and bowel rest; total recovery may take 1–2 weeks.
Key Takeaways
- Abdominal pain—usually lower left—is the main symptom of a diverticulitis attack, with other signs such as fever, bowel changes, and nausea.
- Immediate medical assessment may be needed for severe or persistent symptoms.
- Physical and psychological aftereffects can be significant, sometimes impacting quality of life for months.
- Treatment differs based on severity; mild cases often resolve at home, while severe cases may require hospitalization.
- Dietary and lifestyle changes can help prevent recurrences.
Resources & Support
- Speak with your healthcare provider for individualized management and ongoing symptom assessment.
- Consider counseling or support groups for coping with anxiety or depression post-attack.
- Access reputable online sources for more information and community support.
References
- https://www.bswhealth.com/blog/diverticulitis-flare-up-strategies
- https://www.health.harvard.edu/blog/looking-out-for-diverticulitis-202108162572
- https://www.bswhealth.com/blog/surviving-diverticulitis
- https://www.uclahealth.org/news/release/diverticulitis-patients-reveal-psychological-and-physical-symptoms-long-after-acute-attacks
- https://www.hackensackmeridianhealth.org/en/healthu/2021/07/21/signs-your-diverticulitis-could-be-in-a-flare-up
- https://my.clevelandclinic.org/health/diseases/10352-diverticulitis
- https://utswmed.org/medblog/diverticulitis-symptoms-treatment/
- https://www.holycrosshealth.org/newsroom/stories/digestive-health/scotts-diverticulitis-story
Read full bio of Sneha Tete












