Wet AMD Treatments: Current Options, Innovations, and Outlook
Explore the latest wet AMD treatments, from anti-VEGF injections to innovative delivery systems, and learn what to expect for future vision care.
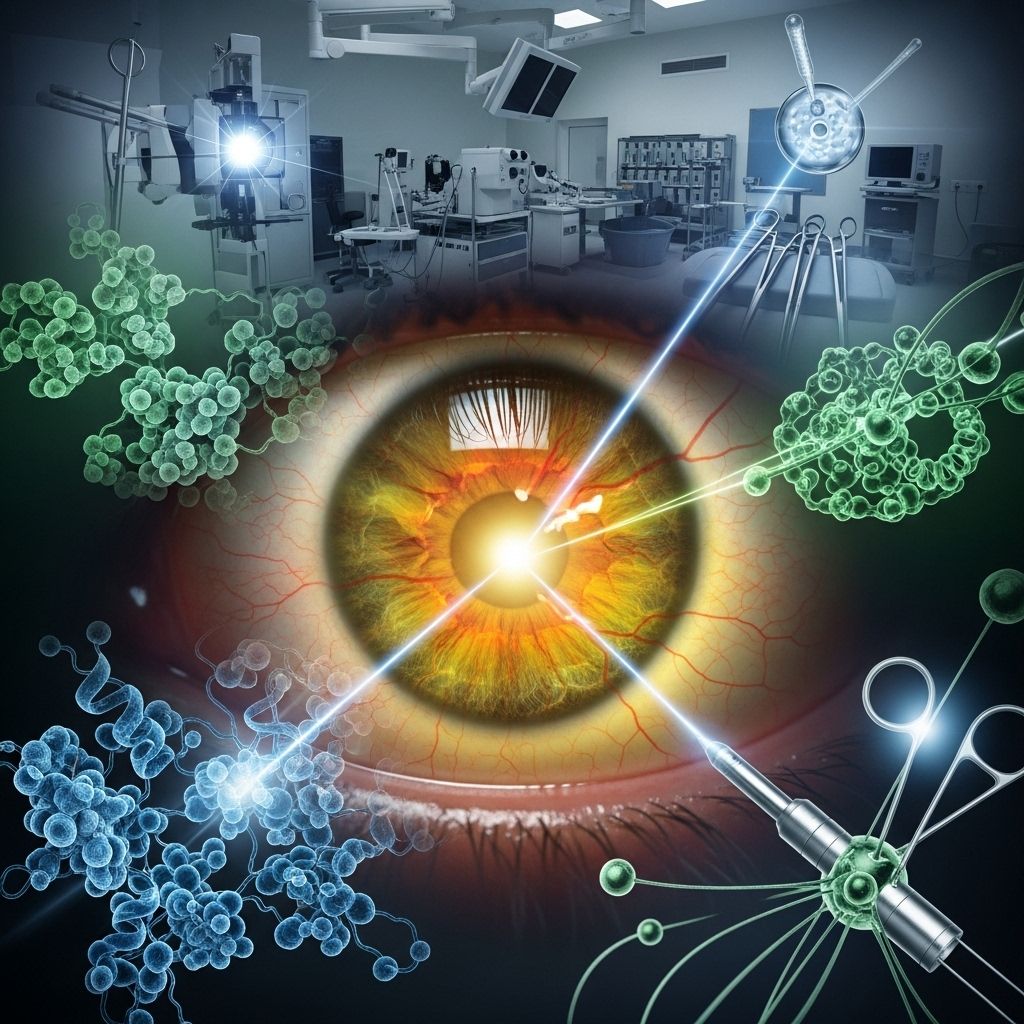
Wet Age-Related Macular Degeneration Treatments: Outlook, Advances, and More
Wet age-related macular degeneration (wet AMD) is a serious condition that can cause permanent loss of central vision if left untreated. As research advances, so do the treatment options available to help slow down or stop vision loss. This article explores standard and emerging treatments for wet AMD, what each involves, their potential side effects, and the outlook for people diagnosed with this retinal disease.
What Is Wet AMD?
Age-related macular degeneration is a leading cause of central vision loss in older adults. There are two types: dry AMD and wet AMD. Wet AMD is the more severe form and progresses faster than dry AMD. It occurs when abnormal blood vessels grow beneath the macula (the central part of the retina responsible for sharp vision), leaking fluid or blood that damages retinal cells.
- Cause: Abnormal blood vessels triggered by vascular endothelial growth factor (VEGF)
- Symptoms: Blurred or distorted central vision, dark spots, rapid vision loss
- Wet AMD almost always begins as dry AMD before progressing
Current Standard Treatments for Wet AMD
The cornerstone of wet AMD management is stopping the growth of abnormal blood vessels and minimizing fluid leakage in the retina. The two main treatment categories are:
- Anti-VEGF Injections (mainstay and most common)
- Photodynamic Therapy (PDT) (less common, used in select cases)
Anti-VEGF (Vascular Endothelial Growth Factor) Injections
Anti-VEGF medications are injected directly into the eye to block the action of VEGF, a protein that stimulates abnormal blood vessel growth. By inhibiting VEGF, these medications help reduce leakage and suppress new vessel formation.
- Frequency: Most people require injections every 4 to 8 weeks initially, then possibly less frequently depending on response
- Procedure: The eye is numbed, cleaned, and the medication is injected with a very fine needle
- Outcomes: Many patients experience stabilized or improved vision, but regular injections are needed to maintain benefits
Types of Anti-VEGF Medications
| Medication Name | Key Features | Typical Frequency |
|---|---|---|
| Bevacizumab (Avastin) | Originally a cancer drug; used ‘off label’ for AMD, safe and effective | Every 4 weeks |
| Ranibizumab (Lucentis) | First anti-VEGF specifically for eye use | Every 4 weeks |
| Aflibercept (Eylea) | Longer lasting, possible to extend dosing interval | Every 8 weeks (after initial monthly injections) |
| Brolucizumab (Beovu) | May allow up to 12 weeks between injections | Every 8–12 weeks |
| Faricimab (Vabysmo) | Newest; first dual action on VEGF and Ang-2 pathways; potentially even less frequent injections | Every 12–16 weeks |
Not all patients respond equally to every medication; doctors tailor treatment to the individual’s needs and drug response.
Photodynamic Therapy (PDT)
PDT uses a light-activated drug called verteporfin, which is injected into a vein in the patient’s arm. The drug accumulates in the abnormal blood vessels in the retina. A special cold laser is then shone into the eye to activate the drug, selectively destroying abnormal vessels without damaging surrounding healthy tissue.
- PDT is now much less common, reserved for specific cases where anti-VEGF injections are not sufficient or not suitable
- May be used in combination with anti-VEGF for better results in some patients
Recent and Emerging Treatment Options
Researchers continue to seek longer-acting, less burdensome therapies for wet AMD. The goal is to reduce the treatment frequency and improve long-term outcomes. Notable recent advances include:
Implantable Drug Delivery Systems
Until recently, most patients had to visit their doctor every 4–8 weeks for eye injections. The introduction of sustained-release implants represents a major step forward. A leading example is the SUSVIMO port delivery system:
- What is it? A tiny, rice-sized implant surgically placed in the eye
- How it works: Continuously releases ranibizumab (anti-VEGF agent) over 6 months or longer
- Benefits:
- Fewer office visits (as few as 2 a year)
- Consistent medication levels in the eye
- Surgical procedure takes about 30 minutes
The implant can be refilled in the office as needed. Not all patients are suitable candidates; discuss options with your ophthalmologist.
Next-Generation Medications
- Vabysmo (Faricimab): Targets both VEGF and Angiopoietin-2 (Ang-2), two key factors in abnormal vessel growth. This dual-action mechanism allows for possible extended dosing to every 16 weeks in some patients.
- Beovu (Brolucizumab): Designed for longer-lasting effects, potentially reducing injection frequency, but some concerns about rare inflammatory side effects require careful monitoring.
- High-dose Aflibercept: Higher dosages under investigation to allow for longer intervals between treatments (8–16 weeks).
Other Approaches Under Investigation
- Gene Therapy: Experimental approaches aim to introduce genetic material that helps the eye produce its own anti-VEGF-like effects, potentially offering long-term control from a single procedure.
- Radiation Therapy: In combination with injections, low-dose targeted radiation may help suppress abnormal vessel growth, but more studies are needed.
Supplements and Lifestyle Recommendations
While dietary supplements do not treat wet AMD directly, certain vitamins and minerals may help slow the progression from intermediate to late AMD. The main formula studied is known as AREDS2, which typically includes:
- Vitamin C
- Vitamin E
- Zinc
- Copper
- Lutein and zeaxanthin
Consult your doctor before starting supplements. They are most beneficial for people with intermediate AMD, not for those with only early changes or with advanced wet AMD in both eyes.
Risks, Side Effects, and Considerations
No treatment is without risks. Understanding potential side effects and complications helps patients make informed choices.
Anti-VEGF Injections
- Redness, soreness at injection site (usually mild and temporary)
- Rare: Infection (endophthalmitis), retinal detachment, increased eye pressure
- Careful cleaning and numbing of the eye help minimize risks
Implants and Surgeries
- Minor surgical risks (bleeding, infection, implant movement)
- Not suitable for all patients
Photodynamic Therapy
- May cause temporary visual disturbances or sensitivity to light
Living with Wet AMD: What to Expect
With early and ongoing treatment, many people with wet AMD can maintain functional central vision and an active lifestyle. However, response varies. Important considerations include:
- Early diagnosis leads to the best visual outcomes
- Continuous monitoring ensures treatment is effective and adapted as needed
- Low vision supports (magnifiers, electronic readers, special lighting) can help maximize the use of remaining vision
- Regular checkups with an ophthalmologist are essential
What Is the Outlook for Wet AMD?
- Many people stabilize or even improve vision with treatment
- Vision loss can recur if therapy is stopped
- Treatment is often lifelong, but new options are easing the burden
- Ongoing research continues to bring hope for improved therapies and even longer intervals between treatments
Frequently Asked Questions (FAQs)
Q: Is there a cure for wet AMD?
A: There is currently no cure for wet age-related macular degeneration, but effective treatments can slow or stop further vision loss and, in some cases, improve vision if started promptly.
Q: How often do anti-VEGF injections need to be given?
A: Most people require injections every 4–8 weeks at first; some newer medications and delivery systems aim to extend dosing intervals to 12–16 weeks or beyond for suitable patients.
Q: What happens if I miss a treatment?
A: Missing injections or delaying treatment can lead to recurrence of abnormal blood vessel activity and vision loss. Notify your doctor if you need to reschedule to keep your treatment on track.
Q: Can supplements or diet reverse wet AMD?
A: Supplements may help slow progression at earlier stages of the disease but do not cure or reverse existing advanced wet AMD. A healthy diet rich in leafy greens, colored vegetables, and fish supports general eye health.
Q: What’s new in wet AMD treatment research?
A: Exciting advances include sustained-release implants like SUSVIMO, dual-action drugs like Vabysmo (faricimab), gene therapy trials, and higher-dose medications for longer protection between treatments. Ask your eye specialist about clinical trials and new developments for which you may be eligible.
Key Takeaways
- Early treatment dramatically improves prognosis for wet AMD
- Anti-VEGF injections are the gold standard, but newer drugs and delivery systems are extending intervals between treatments
- Vision stabilization or improvement is possible, but ongoing management and regular eye exams are essential
- Researchers are exploring gene therapy, sustained-release devices, and combination regimens to further reduce treatment burden in the future
If you experience sudden changes in central vision—such as distortion, blurriness, or dark spots—contact your eye doctor immediately. Early intervention remains the key to preserving sight and quality of life.
References
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration/treatments-wet-amd-advanced-neovascular-amd
- https://pubmed.ncbi.nlm.nih.gov/24555421/
- https://www.goodeyes.com/services/retina/macular-degeneration/
- https://www.macularsociety.org/diagnosis-treatment/treatments/
- https://www.nhs.uk/conditions/age-related-macular-degeneration-amd/treatment/
- https://my.clevelandclinic.org/health/diseases/wet-macular-degeneration
- https://my.clevelandclinic.org/health/diseases/15246-macular-degeneration
- https://www.ajmc.com/view/overview-of-wet-age-related-macular-degeneration
Read full bio of medha deb












