Vitreous Hemorrhage: Causes, Symptoms, Diagnosis, and Treatment
Explore vitreous hemorrhage, a serious eye condition marked by internal bleeding, outlining its symptoms, risk factors, causes, diagnosis, and available treatments.
Vitreous Hemorrhage: Understanding Bleeding Inside the Eye
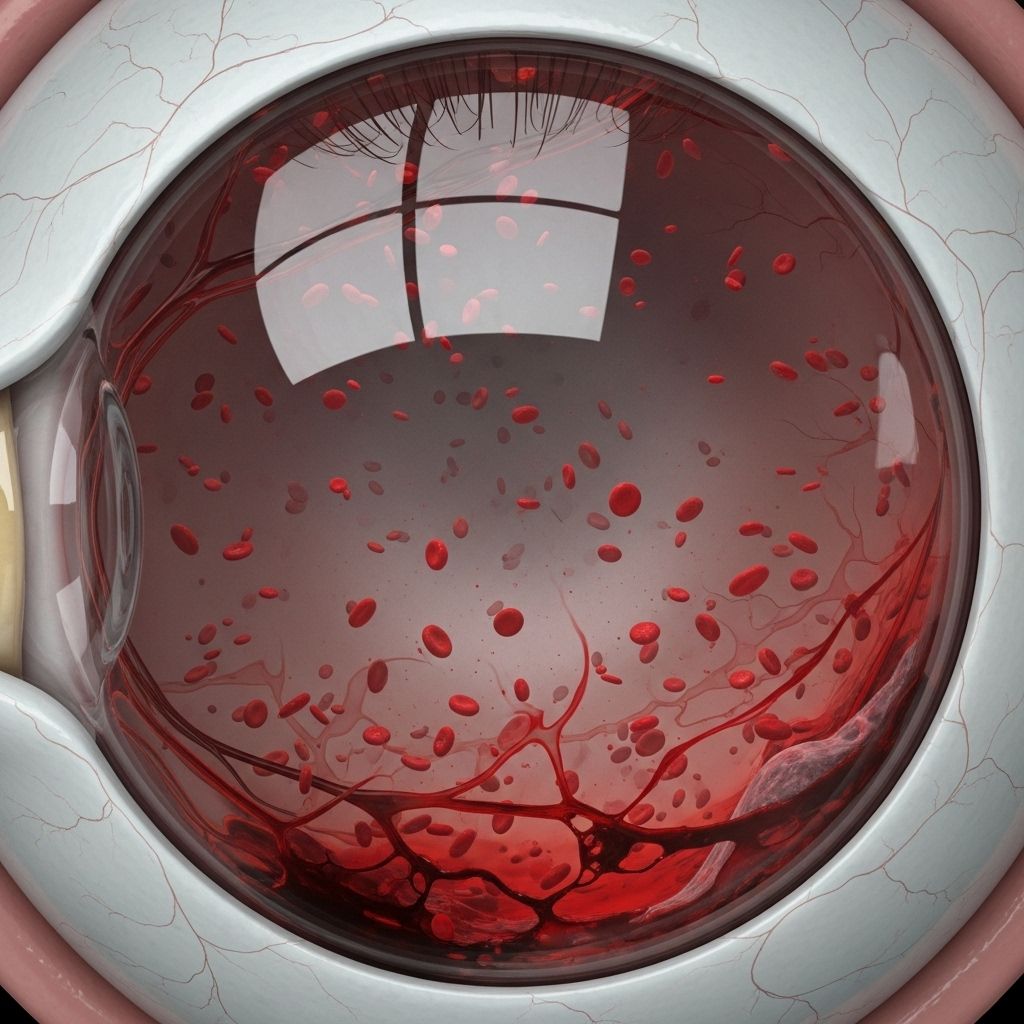
Vitreous hemorrhage is a potentially sight-threatening condition characterized by bleeding within the vitreous chamber of the eye. The vitreous is a clear, gel-like substance that fills most of the eyeball and is crucial for transmitting light to the retina, the light-sensitive tissue at the back of the eye. When blood leaks into this chamber, it interferes with the normal passage of light, leading to visual disturbance or even sudden loss of vision.
What Is Vitreous Hemorrhage?
Vitreous hemorrhage begins when blood enters the vitreous humor—the clear gel occupying the space between the lens and retina. This intrusion can block light from reaching the retina, severely impacting vision. In most cases, the condition presents with sudden, painless vision loss, ranging from mild blurring to total inability to see.
Types of Vitreous Hemorrhage
- Preretinal: Bleeding collects in a boat-shaped pool at the back of your eye, between the retina and the vitreous gel.
- Intravitreal: Blood disperses directly into the vitreous, often settling due to gravity—with color ranging from bright red to yellowish over time.
Symptoms: How to Recognize Vitreous Hemorrhage
- Sudden blurring or clouded vision: Most people notice a rapid decrease in clarity in one eye.
- Dark spots or floaters: These may appear to swirl, float, or drift in your field of vision.
- General vision loss: If the hemorrhage is severe, sight may drop to just light perception.
- Flashing lights: Occasionally, flashes or streaks may accompany the floaters.
- Painless: The condition typically does not cause discomfort.
Common Causes of Vitreous Hemorrhage
Bleeding inside the vitreous chamber can occur due to several underlying issues, often involving the fragile blood vessels within the eye. Major causes include:
- Diabetic Retinopathy: In diabetes, abnormal new blood vessels form, which break easily. Proliferative diabetic retinopathy is a leading cause.
- Posterior Vitreous Detachment (PVD): Separation of the vitreous from the retina can tear vessels, causing bleeding.
- Retinal Tears or Detachment: Breaks in the retina often lead to vessel damage and hemorrhage.
- Ocular Trauma: Blows to the eye or surgical injuries can rupture vessels and lead to acute bleeding.
- Vascular Occlusion and Vasculitis: Diseases blocking retinal vessels or causing inflammation contribute to hemorrhage.
- Other Causes: Terson’s syndrome (associated with brain hemorrhage), Valsalva retinopathy (from straining), and rare genetic or inflammatory diseases.
Table: Causes and Associated Risk Factors
| Cause | Description | Common Risk Factors |
|---|---|---|
| Diabetic Retinopathy | Growth of abnormal blood vessels prone to rupture | Poorly controlled diabetes, long duration of diabetes |
| Retinal Tear/Detachment | Breaks or separations of retinal tissue tearing vessels | High myopia, aging, prior eye surgery |
| Ocular Trauma | Direct injury to the eye, surgical accidents | Sports injuries, physical assault, accidents |
| Vascular Occlusion | Blockage of small retinal vessels | High blood pressure, heart disease, blood disorders |
Risk Factors
- Diabetes: Increases risk for developing abnormal retinal vessels
- High Blood Pressure: Damages delicate blood vessels
- History of Eye Injury: Prior trauma can weaken vessels
- Advanced Age: Higher likelihood of PVD and vessel fragility
- Blood-thinning Medications: Can exacerbate bleeding
Diagnosis: How Doctors Detect Vitreous Hemorrhage
Diagnosing vitreous hemorrhage involves a combination of clinical history, physical exams, and specialized imaging techniques:
- Ophthalmoscopy: Direct examination with a bright light and lens to visualize the blood within the eye
- Slit Lamp Exam: High-magnification inspection of the front and back structures, helping detect subtle hemorrhage
- Ultrasound (B-scan): Especially helpful if vision is blocked by dense blood—can map the extent and location of bleeding
- Fluorescein Angiography: Imaging technique used to assess retinal circulation and pinpoint abnormal vessel growth
- Optical Coherence Tomography (OCT): Cross-sectional images to evaluate retina and vitreous structure
How Does Vitreous Hemorrhage Affect Vision?
The severity of vision loss depends on how much blood enters the vitreous and where it settles:
- Mild cases: Small floaters or haze may clear with time.
- Dense hemorrhage: May block all sight but light perception, requiring urgent intervention.
- Persistent or recurrent: Chronic blood can trigger inflammation and secondary damage to the retina or other structures.
Complications of Vitreous Hemorrhage
- Ghost cell glaucoma: Pressure rise from degenerated red blood cells blocking drainage
- Hemosiderotic glaucoma: Similar mechanism but related to iron toxicity from blood breakdown
- Proliferative vitreoretinopathy: Scar tissue formation from chronic bleeding
- Hemosiderosis bulbi: Iron deposition from blood breakdown, injuring eye tissues
- Retinal detachment: If bleeding is caused by, or leads to, retinal tears
Natural History and Pathophysiology: How Bleeding Resolves
The vitreous cavity is unique in how it processes and clears blood:
- Rapid clot formation: The molecular structure of the vitreous gel enables swift platelet aggregation and clot stabilization.
- Slow fibrin lysis: Fibrin, key to clot strength, degrades slowly in the eye due to low levels of tissue plasminogen activator.
- Extracellular lysis of RBCs: Red blood cells break down more outside cells than inside due to limited macrophage response within the vitreous.
- Vitreous liquefaction: Long-term presence of iron and other breakdown products can lead to collapse of the gel structure.
- Cholesterol crystal formation: Breakdown of red blood cells may lead to shimmering cholesterol deposits—known as synchysis scintillans.
Treatment Options for Vitreous Hemorrhage
The best treatment depends on the underlying cause, the severity, and whether there is associated retinal damage. Approaches include:
- Observation: Mild cases without retinal tears may resolve naturally as the body absorbs the blood. Vision typically improves over weeks to months.
- Medication: In some cases, intravitreal injections such as anti-vascular endothelial growth factor (VEGF) are administered to help shrink abnormal blood vessels.
- Laser Photocoagulation: Used to seal leaky vessels or prevent further bleeding, particularly in diabetic retinopathy.
- Cryotherapy: Freezing therapy can be used to address bleeding vessels.
- Surgery: Pars plana vitrectomy is the main surgical approach for severe or non-resolving hemorrhage—removing the vitreous and replacing it with a clear saline solution.
When Is Surgery Needed?
Surgery is usually reserved for cases where:
- Vision is severely impaired and not improving
- Retinal tears or detachment are present
- The cause of bleeding cannot be diagnosed via non-invasive methods
In all cases, your ophthalmologist will assess the risk and benefit before recommending surgery.
Recovery and Outlook
- Most cases of mild hemorrhage clear on their own over several weeks or months.
- Severe cases or those with underlying disease may experience permanent vision changes.
- Managing underlying conditions like diabetes and hypertension is crucial to prevent recurrence.
Prevention Tips
- Control blood sugar levels in diabetes to minimize risk of abnormal vessel formation.
- Protect eyes from trauma during sports, activities, and work.
- Regular eye exams for at-risk individuals—those with diabetes, high blood pressure, or high myopia.
Frequently Asked Questions (FAQs)
Q: Is vitreous hemorrhage painful?
A: No. Bleeding inside the vitreous chamber is typically painless, although sudden vision changes can be unsettling.
Q: How long does it take for vision to recover after a vitreous hemorrhage?
A: Mild or moderate hemorrhages often clear within several weeks to months as the blood is gradually absorbed. Severe cases may require months or surgical intervention and carry higher risk of permanent vision changes.
Q: Is surgery always necessary?
A: No. Most minor hemorrhages resolve without intervention. Surgery is reserved for sight-threatening cases, persisting hemorrhage, or when retinal tears are present.
Q: Can vitreous hemorrhage recur?
A: Yes. The risk of recurrence is higher in people with poorly controlled diabetes, chronic retinal disease, or those who experience repeat trauma. Managing underlying conditions is critical.
Q: What other complications can arise from vitreous hemorrhage?
A: Risks include secondary glaucoma, retinal detachment, and scarring inside the eye—all requiring specialized care to prevent permanent vision loss.
Q: What should I do if I suddenly lose vision in one eye?
A: Seek immediate evaluation from an eye care professional. Sudden vision loss is always serious and needs urgent diagnosis and management to prevent further damage or complication.
Key Takeaways
- Vitreous hemorrhage is an important cause of sudden, painless vision loss due to bleeding inside the eye’s vitreous chamber.
- Common causes include diabetic retinopathy, retinal tear, trauma, and vascular abnormalities.
- Symptoms include floaters, hazy vision, and reduced sight; pain is usually absent.
- Diagnosis is made through ophthalmoscopy, slit lamp exams, and ocular ultrasound.
- Treatment depends on severity and cause: observation, medication, laser, or vitrectomy surgery.
- Long-term outcome is variable; preventing recurrence by controlling underlying diseases is essential.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10155538/
- https://my.clevelandclinic.org/health/diseases/vitreous-hemorrhage
- https://www.med.umich.edu/1libr/Ophthalmology/Retina/VitreousHemorrhage.pdf
- https://www.healthline.com/health/eye-health/vitreous-hemorrhage
- https://www.healthline.com/health/eye-health/retinal-bleeding
- https://www.medicalnewstoday.com/articles/retinal-hemorrhage
- https://www.ncbi.nlm.nih.gov/books/NBK559131/
Read full bio of medha deb












