Understanding Ureteropelvic Junction Obstruction (UPJ Obstruction)
A comprehensive guide to the causes, symptoms, diagnosis, and treatment of ureteropelvic junction obstruction in children and adults.
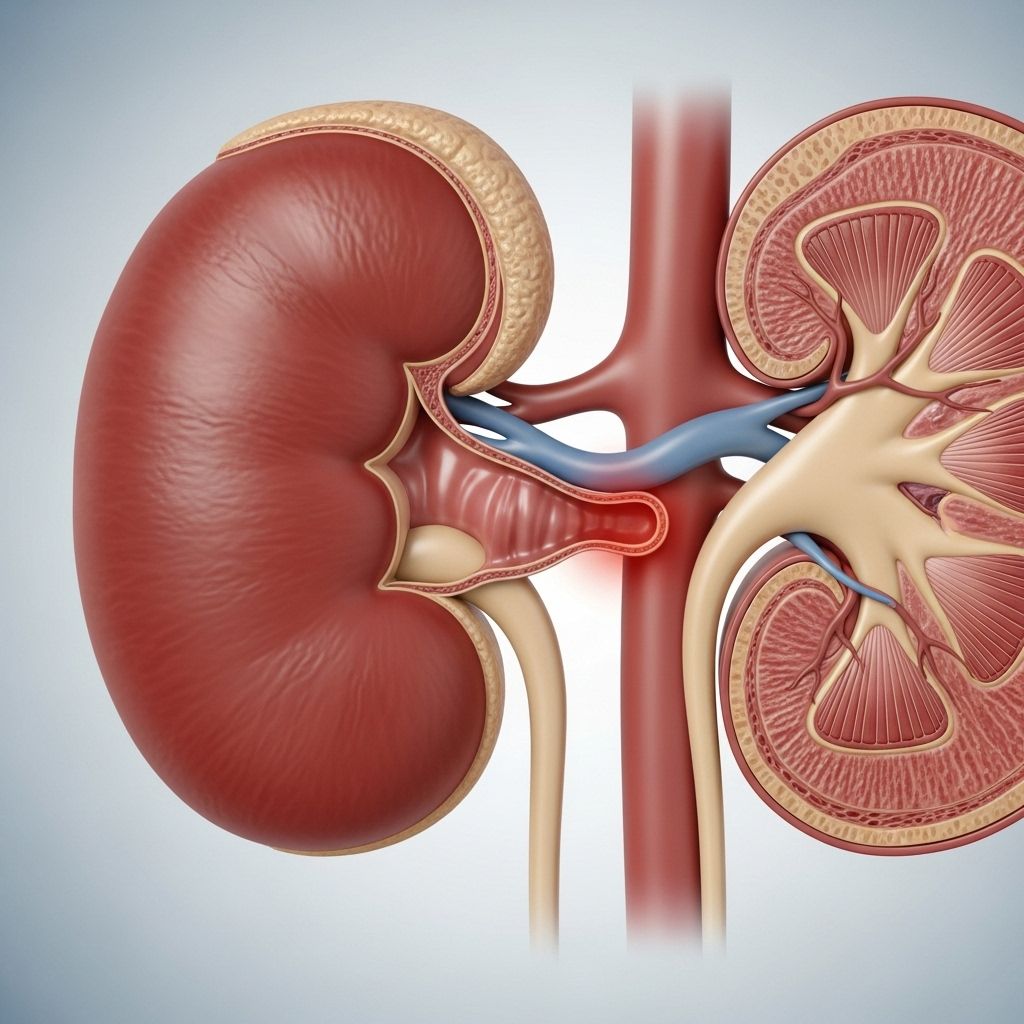
Ureteropelvic junction (UPJ) obstruction is a condition that involves a blockage at the junction where the pelvis of the kidney meets the ureter— the tube which carries urine from the kidney to the bladder. This blockage restricts urine flow, resulting in the swelling of the kidney (hydronephrosis) and potential kidney damage. UPJ obstruction is a significant urological concern, particularly in the pediatric population, though it can also affect older children and adults.
What is Ureteropelvic Junction Obstruction?
The ureteropelvic junction is the anatomical region where the renal pelvis—the funnel-shaped structure in the kidney that collects urine—meets the ureter, the tube that drains urine into the bladder. In UPJ obstruction, this junction becomes blocked or narrowed, impeding the normal outflow of urine. Blocked urine can build up and cause the kidney to dilate, a condition called hydronephrosis.
- UPJ obstruction is the most common obstructive urinary tract disease detected prenatally via ultrasound.
- It can be a congenital (present at birth) or acquired condition.
- The obstruction may affect one or both kidneys but is usually unilateral (one-sided).
Causes of UPJ Obstruction
UPJ obstruction can arise due to a variety of intrinsic (within the junction) or extrinsic (outside compression) causes. These etiologies are broadly classified as congenital or acquired.
Congenital Causes
- Ureteral Hypoplasia: Incomplete or abnormal development of the smooth muscle in the proximal ureter leads to poor peristalsis and functional blockage.
- High Insertion of Ureter: If the ureter attaches higher than normal on the renal pelvis, sharp angulation impedes urine drainage and causes obstruction.
- Crossing Blood Vessels: A blood vessel, often from the kidney’s lower pole, may cross the ureter and compress it, causing about 50% of symptomatic pediatric cases needing surgery.
- Kidney Malrotation: Rarely, abnormal kidney rotation may lead to UPJ obstruction.
Acquired Causes
- Extrinsic Compression: Conditions outside the ureter compress the UPJ (e.g., retroperitoneal fibrosis, enlarged lymph nodes due to cancer, tumors, or positional factors of a mobile kidney).
- Intrinsic Factors:
- Chronic Inflammation: Ongoing inflammation from stones, infection, or radiation can cause scarring/narrowing.
- Ureteral Tumors: Such as transitional cell carcinoma.
- Iatrogenic Causes: Scarring or strictures after surgeries or endoscopic interventions for stones or previous UPJ repairs.
It's important to be aware of conditions like struvite stones, which can complicate cases of UPJ obstruction. To learn more about the causes and treatment options for struvite stones, check out our extensive resource on struvite stones: causes, symptoms, treatment, and prevention.
Pathophysiology: How does UPJ Obstruction Affect the Kidney?
The normal flow of urine from the renal pelvis to the ureter is determined by:
- The pressure within the renal pelvis.
- The compliance (flexibility) of the urinary system.
- The diameter of the ureteropelvic junction.
- The peristaltic (wave-like) contractions of the ureter’s muscle wall.
When UPJ obstruction occurs:
- Urine cannot flow freely and backs up in the kidney, leading to hydronephrosis.
- Prolonged obstruction causes increased production of inflammatory peptides, activation of the renin-angiotensin system, and eventual decrease in kidney function (glomerular filtration rate, or GFR).
- If not treated in time, it may lead to irreversible kidney damage.
Who is at Risk?
UPJ obstruction can present during different stages of life depending on the underlying cause:
- Fetuses and Infants: Most commonly identified by prenatal (before birth) ultrasound due to routine screening for urinary tract abnormalities.
- Older Children: May become symptomatic later or be diagnosed due to complications or incidental findings.
- Adults: Less common, may result from acquired causes such as kidney stones, prior surgical procedures, or tumors.
Signs and Symptoms of UPJ Obstruction
Symptoms vary widely and are sometimes absent, especially when detected through prenatal ultrasound. When present, classic symptoms may include:
- Abdominal, back, or flank pain.
- Hematuria: Blood in the urine.
- Abdominal mass/lump: Due to the swollen kidney.
- Recurrent urinary tract infections (UTIs), sometimes accompanied by fever.
- Vomiting or gastrointestinal symptoms.
- Poor growth or failure to thrive in infants.
In babies, most often UPJ obstruction is detected before symptoms appear, thanks to improved prenatal imaging. In older children and adults, symptoms can be more pronounced:
- Back/flank pain (may be intermittent or associated with fluid intake).
- Nausea or vomiting.
- Visible blood in urine or urinary tract infection.
How is UPJ Obstruction Diagnosed?
Diagnosing UPJ obstruction involves a combination of imaging studies and laboratory tests. The goal is to confirm the blockage, assess its severity, and evaluate the impact on kidney function.
- Prenatal Ultrasound: Most common in infants, detects hydronephrosis before birth.
- Postnatal Ultrasound: Confirms continued presence and extent of hydronephrosis after birth.
- Renal Nuclear Medicine Scans (e.g., MAG3, DTPA): Measures kidney function and drainage capacity.
- Voiding Cystourethrogram (VCUG): Rules out other causes of hydronephrosis like vesicoureteral reflux.
- Blood Tests: Assesses kidney function (measuring creatinine and electrolytes).
| Test Name | Purpose |
|---|---|
| Prenatal Ultrasound | Detects hydronephrosis before birth |
| Postnatal Ultrasound | Assesses severity, size, and persistence of obstruction |
| Renal Nuclear Scan | Evaluates drainage and split kidney function |
| VCUG | Rules out vesicoureteral reflux as a cause |
| Blood Tests | Assesses overall kidney health |
Treatment Options for UPJ Obstruction
The management of UPJ obstruction depends on patient age, severity of obstruction, symptoms, and effect on kidney function. Conservative monitoring and surgical intervention are the main approaches.
Observation and Monitoring
- Mild cases with adequate kidney function and no symptoms are often monitored with regular ultrasounds and occasional nuclear scans.
- Spontaneous improvement is common in infants with mild hydronephrosis.
Surgical Treatment
Indicated when there is progressive obstruction, decline in function, significant symptoms, or recurrent infections.
- Pyeloplasty: The gold standard procedure, involving surgical reconstruction of the UPJ to relieve obstruction. Modern techniques favor minimally invasive, laparoscopic, or robotic-assisted approaches when possible.
- Endoscopic Treatments (Balloon Dilation or Endopyelotomy): Sometimes considered in selected older children or adults, but less favored in young children.
- Temporary Drainage (Stents or Nephrostomy Tubes): Employed in urgent cases to relieve severe blockage or infection before definitive surgery.
Prognosis: When treated appropriately, most children and adults recover full or near-normal kidney function. Delay in intervention, especially with worsening function or infection, can lead to permanent kidney damage.
Living with UPJ Obstruction: Outlook and Long-term Management
Most patients with timely diagnosis and treatment of UPJ obstruction have excellent outcomes. Regular follow-up is necessary to monitor kidney function and ensure the success of the intervention.
- Follow-up ultrasounds and nuclear imaging assess long-term function and detect any recurrence.
- In rare cases, further surgery may be required if re-obstruction occurs.
- Lifelong monitoring may be advised if significant damage occurred before treatment.
Frequently Asked Questions (FAQs)
What causes ureteropelvic junction obstruction in children?
In most cases, the cause is a developmental issue where the connection between the ureter and renal pelvis forms abnormally, leading to narrowing and accumulation of urine. Occasionally, a crossing blood vessel or acquired factors (like infection or scar tissue) may be the cause.
What are the symptoms of UPJ obstruction?
Symptoms can vary. Many newborns show no symptoms and are identified by prenatal ultrasound. When symptoms occur, they often include persistent or intermittent abdominal, back, or side pain, blood in the urine, a palpable abdominal mass, urinary tract infections with fever, and sometimes vomiting or poor growth in infants.
How is UPJ obstruction diagnosed?
Diagnosis commonly involves imaging studies: ultrasound (before and after birth), nuclear scans to determine kidney drainage and function, and—if needed—voiding cystourethrogram to exclude other causes. Blood work may also be performed to assess kidney function.
Do all UPJ obstructions require surgery?
No. Many mild cases are managed conservatively with observation, especially in infants when kidney function is adequate and symptoms are absent. Surgery is indicated when there is evidence of progressive deterioration, significant symptoms, or repeated infections.
What is the outlook for patients with UPJ obstruction?
With proper intervention, most patients do very well, regaining normal or near-normal kidney function. Regular monitoring is important to ensure no recurrence or long-term complications.
Key Takeaways
- UPJ obstruction is a common cause of hydronephrosis, especially in infants and children.
- It results from a blockage at the junction of the kidney and ureter, impairing normal urine drainage.
- Early diagnosis—often via prenatal ultrasound—has significantly improved outcomes.
- Treatment depends on severity and may involve observation or surgery, with a high rate of success following intervention.
References
- https://www.ncbi.nlm.nih.gov/books/NBK560740/
- https://www.chop.edu/conditions-diseases/ureteropelvic-junction-upj-obstruction
- https://www.childrensnational.org/get-care/health-library/congenital-ureteropelvic-junction-obstruction
- https://www.uclahealth.org/medical-services/urology/conditions-treated/adult-conditions/ureteropelvic-junction-obstruction
- https://www.mayoclinic.org/diseases-conditions/ureteral-obstruction/symptoms-causes/syc-20354676
- https://www.urologyhealth.org/urology-a-z/u/ureteropelvic-junction-(upj)-obstruction
- https://dcurology.net/common-problems/ureteropelvic-junction-upj-obstruction.php
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/u/ureteropelvic-junction-upj-obstruction.html
Read full bio of Sneha Tete












