Understanding Viral Gastroenteritis: Causes, Symptoms, and Prevention
Comprehensive guide to viral gastroenteritis, covering causes, symptoms, prevention, treatment, and recovery insights.
Understanding Viral Gastroenteritis
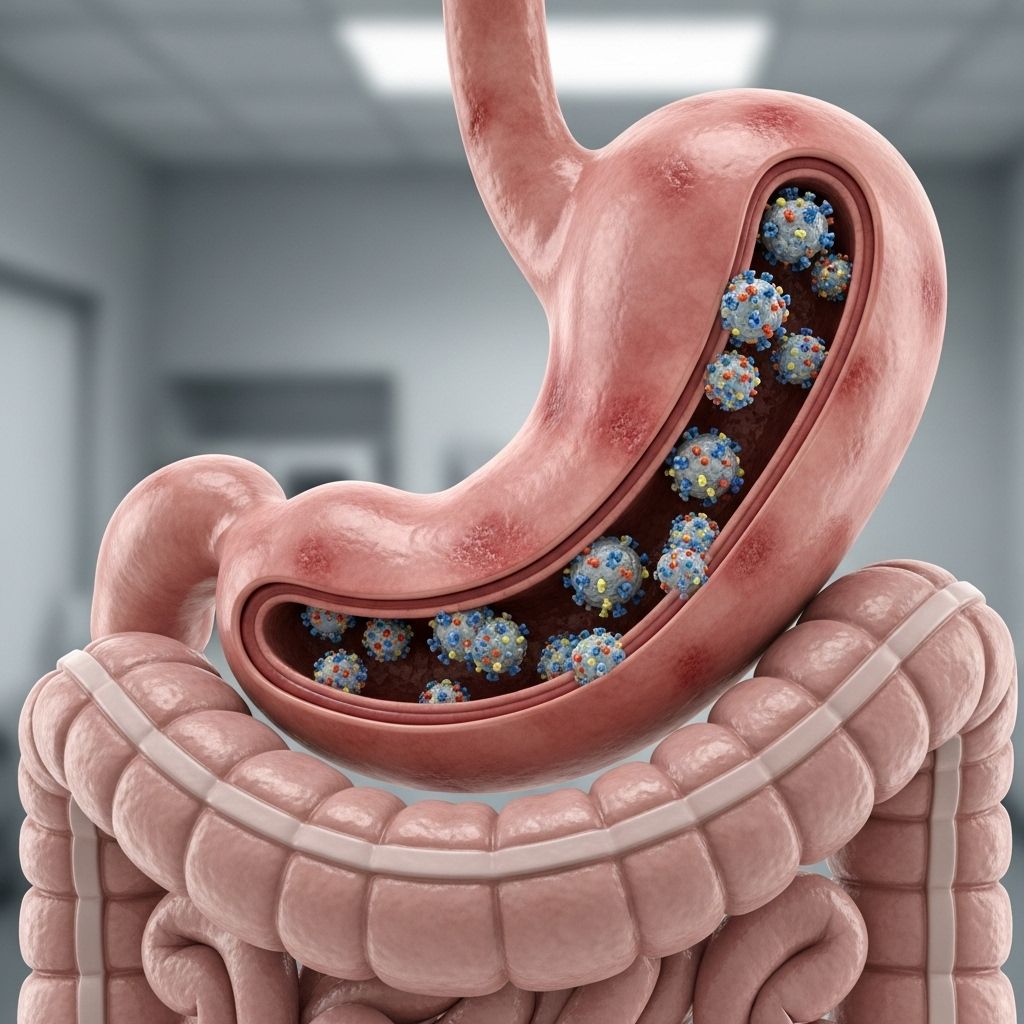
Viral gastroenteritis, often called the “stomach flu,” is a common and highly contagious infection of the stomach and intestines. Characterized by symptoms such as nausea, vomiting, diarrhea, abdominal pain, and sometimes fever, viral gastroenteritis affects millions every year, leading to discomfort and potential health risks—especially for vulnerable populations. Unlike influenza, which attacks the respiratory tract, viral gastroenteritis targets the digestive system. This article explores viral gastroenteritis in detail, including causes, symptoms, transmission, treatment, prevention, and recovery tips, to help you protect yourself and others.
What Is Viral Gastroenteritis?
Viral gastroenteritis is an acute inflammation of the stomach and intestines caused by several different viruses. This condition disrupts the normal function of the gastrointestinal tract and typically results in a rapid onset of symptoms. Commonly referred to as the “stomach flu,” viral gastroenteritis is distinct from influenza, which only affects the respiratory system and never the intestines.
- Target Organs: Stomach, small intestine, and large intestine (colon).
- Primary Symptoms: Diarrhea, vomiting, abdominal pain, and low-grade fever.
- Commonality: One of the most frequent causes of illness worldwide, particularly among children, older adults, and those with weakened immune systems.
Understanding Gastroenteritis vs. Influenza
| Feature | Viral Gastroenteritis | Influenza (Flu) |
|---|---|---|
| Affected Area | Stomach & intestines | Nose, throat, lungs |
| Main Symptoms | Vomiting, diarrhea, cramps | Cough, sore throat, fever |
| Common Name | Stomach flu | Flu |
| Cause | Norovirus, rotavirus, adenovirus | Influenza A & B viruses |
Causes of Viral Gastroenteritis
Several viral agents are known to cause gastroenteritis, with variations in prevalence depending on age and exposure:
- Norovirus: The most common cause in adults and outbreaks in institutional settings. Extremely contagious, responsible for many cases in the United States.
- Rotavirus: Primarily affects young children and infants. Vaccines are available and can significantly reduce incidence.
- Adenovirus, astrovirus: Less common causes, can affect both children and adults.
These viruses cause inflammation through direct invasion and destruction of the lining of the stomach and intestines, leading to the characteristic symptoms of vomiting and diarrhea.
How the Infection Spreads
- Person-to-person contact: Shaking hands, sharing utensils, or close proximity with someone infected.
- Contaminated food or water: Consuming food prepared by unwashed hands or water tainted with sewage.
- Surface contact: Touching surfaces contaminated with the virus (door handles, faucets) and then touching the mouth or face.
Symptoms of Viral Gastroenteritis
Symptoms usually develop within 12–48 hours after exposure to the virus and can range from mild to severe, depending on the specific virus, the person’s age, and general health condition.
- Watery, non-bloody diarrhea
- Nausea and/or vomiting
- Stomach cramps and pain
- Low-grade fever
- Headache and muscle aches
- Occasional chills
- Loss of appetite
Symptoms typically last 1–3 days but, in some cases, can extend for up to two weeks as the digestive tract recovers.
Warning Signs: When to Seek Medical Attention
- Diarrhea that lasts more than three days.
- Vomiting that persists for more than 24 hours.
- Fevers above 102°F (39°C).
- Blood in stool or vomit.
- Severe abdominal pain.
- Signs of dehydration: dry mouth, dark urine, sunken eyes, lack of tears, dizziness, or extreme thirst.
Dehydration is the most serious complication and can be life-threatening, especially in infants, older adults, or those with chronic illnesses.
Who Is Most at Risk?
Anyone can contract viral gastroenteritis, but some populations are more vulnerable to severe symptoms or complications:
- Infants and young children
- Elderly adults
- Individuals with weakened immune systems
- Residents in communal living settings (nursing homes, dormitories, daycares, cruise ships)
- Travelers, especially to regions with unsafe water supplies or poor sanitation
How Is Viral Gastroenteritis Diagnosed?
Diagnosis is often based on clinical symptoms and history of recent exposure, since most cases resolve without medical attention and laboratory tests aren’t usually needed. However, a doctor may order stool testing in the following cases:
- Severe or persistent cases
- Immunocompromised individuals
- Outbreak settings, to identify the exact virus
- Unusual presentations (bloody diarrhea, high fever, suspected bacteria or parasites)
Treatment and Self-Care
There is no specific antiviral medication for viral gastroenteritis. The best approach is supportive care, focusing on staying hydrated and managing symptoms while the infection runs its course.
Hydration: The Cornerstone of Treatment
- Fluid Replacement: Drink water, clear broths, oral rehydration solutions, and electrolyte-rich fluids. Avoid caffeine, alcohol, and acidic drinks, which can worsen hydration loss or upset the stomach further.
- For Children: Use pediatric oral rehydration solutions (like Pedialyte); continue breast milk or formula for infants as directed by a healthcare professional.
- For Adults: Sipping clear fluids frequently is better than drinking large amounts at once if experiencing nausea.
- Electrolyte Replacement: Eating saltine crackers or oral solutions helps restore electrolyte balance.
When to Use Over-the-Counter Medications
- Loperamide (Imodium) or Bismuth Subsalicylate (Pepto-Bismol): May help reduce diarrhea in adults. Do not give these medications to children unless directed by a physician.
- Avoid these medications if symptoms include high fever or bloody stools, which could point to other infections that require different treatments.
Hospitalization and intravenous fluids may be needed for people who can’t keep fluids down or are severely dehydrated.
What to Eat During Recovery
It was once thought that a restricted “BRAT” diet (bananas, rice, applesauce, toast) was necessary during gastroenteritis. However, research shows there is no need for a restricted diet if you feel ready to eat. Most people can return to their normal diet as symptoms improve. Stick initially to:
- Bland, easy-to-digest foods (crackers, rice, lean meats, bananas)
- Avoid spicy, greasy, or high-fiber foods until fully recovered
- Avoid dairy if it temporarily worsens symptoms
Prevention: Reducing the Spread
Viral gastroenteritis spreads quickly and easily. The following steps are critical for limiting your risk and preventing outbreaks:
- Wash hands thoroughly and frequently with soap and water, especially after using the bathroom, changing diapers, and before eating or preparing food.
- Disinfect surfaces that may have been contaminated by stool or vomit using an appropriate disinfectant (bleach-based solutions are most effective against norovirus).
- Isolate sick individuals—keep children and adults with symptoms home until at least 48 hours after vomiting and diarrhea stop.
- Rinse fruits and vegetables well, and thoroughly cook shellfish.
- Vaccinate children against rotavirus (as recommended by your pediatrician).
- Avoid sharing eating utensils, towels, and bedding during illness and recovery.
When traveling, especially to countries with known water sanitation issues, use bottled or boiled water and avoid raw foods washed in local water.
Complications and Long-Term Effects
The key danger of viral gastroenteritis is dehydration. Severe dehydration can lead to complications such as:
- Kidney failure
- Seizures (particularly in children)
- Loss of consciousness
Most people recover fully after a short time, but bowel habits may take a week or longer to normalize. Persistent or severe symptoms should prompt a medical evaluation.
Frequently Asked Questions (FAQs)
Q: How can I tell the difference between viral gastroenteritis and food poisoning?
A: Symptoms are often similar (vomiting, diarrhea, cramps), but food poisoning is usually caused by bacteria or toxins and may develop more rapidly after consuming a suspect meal. Viral gastroenteritis typically develops 12-48 hours after exposure to the virus.
Q: Is there any way to cure viral gastroenteritis quickly?
A: There is no specific cure; focus on supportive care—rest, hydration, and gradual return to normal diet. Antibiotics are not effective against viruses.
Q: Can you catch viral gastroenteritis from the air?
A: It primarily spreads via the fecal-oral route, but airborne droplets can carry the virus during episodes of vomiting, emphasizing the importance of surface disinfection and isolation.
Q: What is the best drink for rehydration?
A: Oral rehydration solutions (such as Pedialyte or homemade mixtures of water, salt, and sugar) are best for severe cases. For mild dehydration, water, clear broths, and diluted juice are helpful; avoid sugary or caffeinated beverages.
Q: Can pets give me viral gastroenteritis?
A: The viruses that cause gastroenteritis in humans do not typically infect pets and vice versa, so transmission from dogs or cats to humans is not a concern.
Q: How long am I contagious?
A: You may be contagious from the moment symptoms begin and for several days after they resolve, especially with norovirus. Practice careful hygiene even after symptoms disappear.
References
This article synthesizes authoritative information from medical sources, including the National Institute of Diabetes and Digestive and Kidney Diseases, the Mayo Clinic, Harvard Health, and public health resources. For specific health concerns, consult your healthcare provider.
References
- https://publichealth.georgetown.edu/viral-gastroenteritis/
- https://www.niddk.nih.gov/health-information/digestive-diseases/viral-gastroenteritis/treatment
- https://www.mayoclinic.org/diseases-conditions/viral-gastroenteritis/symptoms-causes/syc-20378847
- https://www.health.harvard.edu/diseases-and-conditions/gastroenteritis-in-adults-a-to-z
- https://my.clevelandclinic.org/health/diseases/12418-stomach-flu
- https://healthservices.brown.edu/sites/default/files/handouts/Stomach-Flu-20.pdf
- https://medlineplus.gov/gastroenteritis.html
Read full bio of Sneha Tete












