Understanding Tracheostomy: Procedure, Care, and Recovery
Essential information on tracheostomy, from reasons and risks to daily care, tube changing, and long-term outcomes.
A tracheostomy is a surgical procedure that creates a direct airway through an opening in the neck into the windpipe (trachea). Tracheostomies are typically performed to help individuals breathe when their usual airway is blocked or impaired, or when long-term respiratory support is required. This guide provides an in-depth look at the reasons, procedures, potential risks, daily care, and life adjustments associated with tracheostomy.
What is a Tracheostomy?
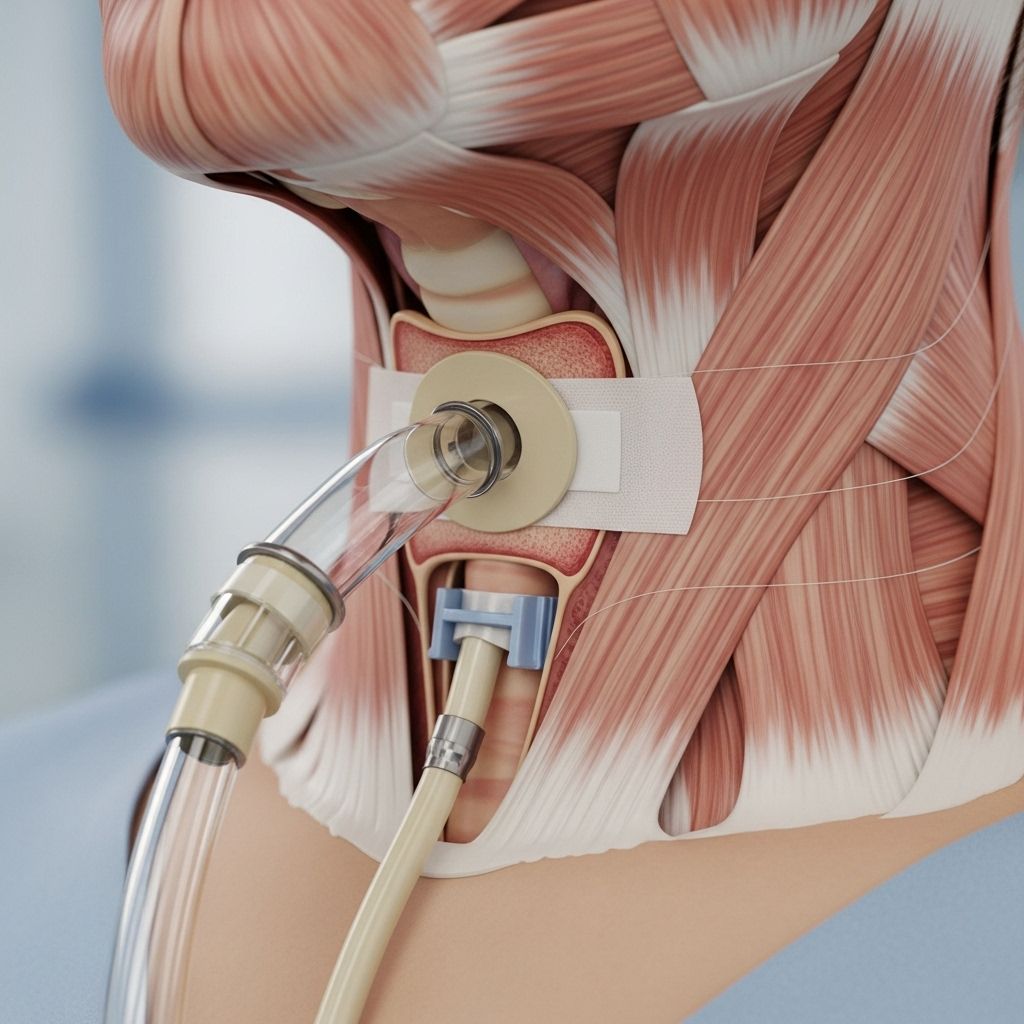
A tracheostomy involves making a small opening (called a stoma) in the anterior (front) aspect of the neck, just below the larynx (voice box), through which a tracheostomy tube is placed directly into the trachea. The tube helps maintain an open airway, facilitates breathing, and can also assist in removing tracheal secretions.
- Tracheostomy tube: A small, curved tube inserted through the stoma into the trachea.
- Stoma: The surgically created hole in the neck and trachea through which the tube passes.
- The tube may be temporary or permanent depending on the underlying condition.
Why is a Tracheostomy Needed?
There are several medical reasons why a person may require a tracheostomy. The most common include:
- Airway obstruction: Blockages due to swelling, injury, tumors, or foreign objects in the upper airway.
- Long-term ventilation: When mechanical ventilation is needed for extended periods, such as in neurological diseases or after major surgery.
- Chronic lung disease: Conditions such as chronic obstructive pulmonary disease (COPD) that result in difficulty clearing secretions.
- Trauma: Severe facial or neck injuries compromising normal breathing pathways.
- Congenital abnormalities: Birth defects that narrow or block airways, especially in infants and children.
- Neuromuscular disorders: Illnesses such as amyotrophic lateral sclerosis (ALS) or spinal cord injury that weaken the muscles needed for breathing.
Types of Tracheostomy Procedures
There are two main types of tracheostomy procedures, each suited for particular needs:
- Surgical tracheostomy: The traditional method, performed in a controlled surgical setting under general anesthesia. This allows the surgeon to see and work directly on the tissues.
- Percutaneous tracheostomy: A less invasive approach typically done in the intensive care unit (ICU) using specialized needles and dilators, guided by imaging and often under local anesthesia and sedation.
- Temporary tracheostomy: Used when airway issues are expected to resolve over time.
- Permanent tracheostomy: Required for ongoing or irreversible airway or breathing problems.
How is a Tracheostomy Performed?
The details of the tracheostomy procedure may vary depending on the patient’s condition and the experience of the surgical team. In most cases, the following steps are involved:
- The patient is positioned on their back, with a rolled towel or pillow under the shoulders to extend the neck.
- Anesthesia is administered: General anesthesia (patient is asleep) is most common, but local anesthesia may be used in emergencies.
- The skin on the lower part of the neck is cleaned with antiseptic solution.
- A horizontal or vertical incision is made just below the Adam’s apple, between the larynx and the top of the chest.
- The surgeon separates muscles and may move or partially divide the thyroid gland to access the trachea (windpipe).
- A small window is cut in the tracheal cartilage, creating an opening into the airway.
- A tracheostomy tube is inserted through the stoma into the trachea following the natural curve of the windpipe.
- The tube is secured using sutures, surgical tape, or a neck strap.
- The skin around the stoma is cleaned, and a dressing is placed as needed.
Some situations require immediate tracheostomy with minimal preparation, especially in severe airway obstruction. In most large hospitals, a team approach includes surgeons, anesthesiologists, nurses, and sometimes respiratory therapists.
What Are the Risks and Possible Complications?
As with any surgical procedure, a tracheostomy carries potential risks. It is important to understand both short-term and long-term complications before undergoing the procedure.
- Bleeding: Most common immediately after the surgery due to injury to blood vessels in the neck or trachea.
- Infection: The tracheostomy stoma or lungs can become infected if care routines are not meticulously followed.
- Damage to the trachea: Incorrect placement or tube management can injure the tracheal wall.
- Tube blockage or displacement: Thick secretions or movement of the tube can obstruct airflow and may be life-threatening if not promptly addressed.
- Air leaks: Escape of air under the skin (subcutaneous emphysema) or into the chest cavity (pneumothorax).
- Difficulty speaking: The airflow bypasses the vocal cords, making normal speech challenging unless special speaking valves are fitted.
Other rare complications can include damage to nearby structures (thyroid gland, esophagus, or major blood vessels), tracheal narrowing (stenosis), and formation of abnormal connections (tracheoesophageal fistula).
Living with a Tracheostomy Tube
The presence of a tracheostomy tube has significant implications for day-to-day activities, but most people are able to adapt to new routines with time and support. Key points to consider include:
- Airway maintenance: Routine suctioning, cleaning, and tube changes are required to prevent infections and blockages.
- Humidification: The lungs normally receive humidified air; with a tracheostomy, added moisture is needed to prevent dryness and keep the tube clear.
- Speech: Talking is difficult initially, but many people can use speaking valves, electrolarynx devices, or learn esophageal speech (especially if the larynx is removed).
- Eating and drinking: Some patients can eat and drink normally, while others may require dietary modifications or tube feeding, especially if swallowing is impaired.
- Physical activity: With guidance, most daily activities are possible, though water sports and dusty environments should be avoided.
Caring for a Tracheostomy at Home
Once at home, proper care of the tracheostomy site and tube is essential to minimize complications. Usually, patients and caregivers are taught these skills by hospital teams before discharge.
Daily Care Steps
- Hand hygiene: Wash hands for 3€“5 minutes before any care procedure.
- Cleaning the stoma: Use sterile water or saline and gauze to clean the skin around the tube daily.
- Changing dressings: Dressings should be changed whenever they are wet or soiled to prevent infection.
- Suctioning: Remove mucus from the trachea using a sterile suction catheter as needed. Suctioning frequency varies by patient.
Changing the Tracheostomy Tube
Tracheostomy tubes may need to be changed regularly, usually every 1 to 4 weeks depending on patient factors, tube type, and healthcare provider recommendations. The process can be performed in a hospital or, with training, at home by caregivers or even the patient.
- Assemble all supplies: new tube, water-based lubricant, gloves, ties or tape, scissors (if using traditional ties), and suction equipment.
- Wash hands and put on gloves.
- Remove the old tube gently, following the natural curve of the trachea.
- Clean the stoma and surrounding skin.
- Lubricate and gently insert the new tube.
- Remove the obturator once the tube is in place and secure the tube with new ties or Velcro straps.
- Check for air flow and breathing comfort. Apply supplemental oxygen if prescribed and monitor for signs of breathing difficulty or skin color change.
Immediate help should be sought if:
- The tube becomes blocked and can’t be cleared with suction.
- The tube falls out and can’t be replaced.
- There is severe bleeding or sudden difficulty breathing.
Talking and Eating with a Tracheostomy
With a tracheostomy, airflow no longer passes through the vocal cords in the usual way, making speech difficult. However, several strategies can help:
- Speaking valves: One-way valves (like the Passy-Muir valve) fit over the trach tube and allow patients to speak by redirecting exhaled air through the vocal cords.
- Cuff deflation: Deflating the tracheostomy tube’s cuff (if present) can help air reach the vocal cords for speech, under medical guidance.
- Alternative communication: Writing, lip reading, or electronic devices may be needed initially.
Eating and drinking may also be affected. Speech and swallowing therapists can assess swallowing ability and help develop techniques or recommend diet modifications. Tube feeding may be necessary in some patients, especially immediately after surgery or in those at risk for aspiration (food entering the airway).
Long-Term Outlook and Potential for Decannulation
The long-term prognosis after a tracheostomy depends on the underlying reason for the procedure and overall patient health. For many, the tracheostomy is a temporary measure; for others, it may become a permanent solution.
- Temporary tracheostomy: If breathing or airway issues resolve, the tube can often be removed (decannulation), and the stoma will gradually close.
- Permanent tracheostomy: Needed for irreversible conditions or severe injuries.
- Adaptation: Most patients and their families adapt to living with a tracheostomy, especially when provided education, training, and support from healthcare professionals.
When to Call the Doctor
- Difficulty breathing despite suction or tube changes
- Excessive bleeding or signs of infection (redness, pus, swelling around the stoma)
- Sudden pain, swelling, or change in voice or swallowing ability
- Persistent cough or fever that does not resolve
Frequently Asked Questions (FAQs)
Q: Is a tracheostomy permanent?
A: Not always. Some tracheostomies are temporary and can be closed once the underlying issue resolves. Others become permanent, especially with irreversible airway or neurological conditions.
Q: How do you speak with a trach tube?
A: Special speaking valves can be fitted to redirect air through the vocal cords. Many patients work with speech therapists to learn new ways to communicate.
Q: Does a tracheostomy hurt?
A: The procedure is performed under anesthesia to prevent pain. Some discomfort is normal during recovery, but pain usually decreases as healing progresses.
Q: What supplies are needed for home care?
A: You’ll need cleaning supplies (sterile water, saline, gauze), suction catheters, new tracheostomy tubes, tube ties or Velcro straps, gloves, and sometimes humidifiers.
Q: Can you swim or bathe with a tracheostomy?
A: It is important to avoid swimming or submerging the tracheostomy site in water to prevent accidental aspiration. Ask your healthcare provider about safe bathing techniques.
Q: Does a trach affect smelling or tasting?
A: Because normal airflow through the nose and mouth is reduced, some loss of taste and smell can occur. Many patients recover these senses if the tube is removed and healing is complete.
Summary Table: Key Points About Tracheostomy
| Aspect | Details |
|---|---|
| Definition | Surgical opening through the neck into the trachea to aid breathing |
| Main Reasons | Airway blockage, long-term ventilation, neuromuscular diseases, trauma |
| Risks | Bleeding, infection, tube displacement, pneumonia, airway injury |
| Daily Care | Cleaning, suctioning, tube change, stoma care, humidification |
| Speech | Difficult but possible with speaking valve or alternative communication aids |
| Eating | May require adaptation; some need modified diets or feeding tubes |
| Prognosis | Varies by underlying condition; some can have tube removed, others require life-long care |
Living with a tracheostomy requires adjustment, but with proper care and support, many individuals can return to a fulfilling and active life.
References
- https://www.youtube.com/watch?v=DzROHk_5rV4
- https://www.healthline.com/health/tracheostomy
- https://www.youtube.com/watch?v=u6tma0igkD0
- https://www.webmd.com/lung/lung-tracheostomy
- https://bioethics.jhu.edu/wp-content/uploads/2018/12/MWPH_Tracheostomy-Guide_r1.pdf
- https://www.ncbi.nlm.nih.gov/books/NBK555919/
Read full bio of medha deb












