Understanding Prion Diseases: Causes, Symptoms, Diagnosis, and Prevention
Explore the origins, types, symptoms, diagnosis, treatment, and prevention of prion diseases for improved awareness and health management.
Prion Diseases: An In-depth Overview
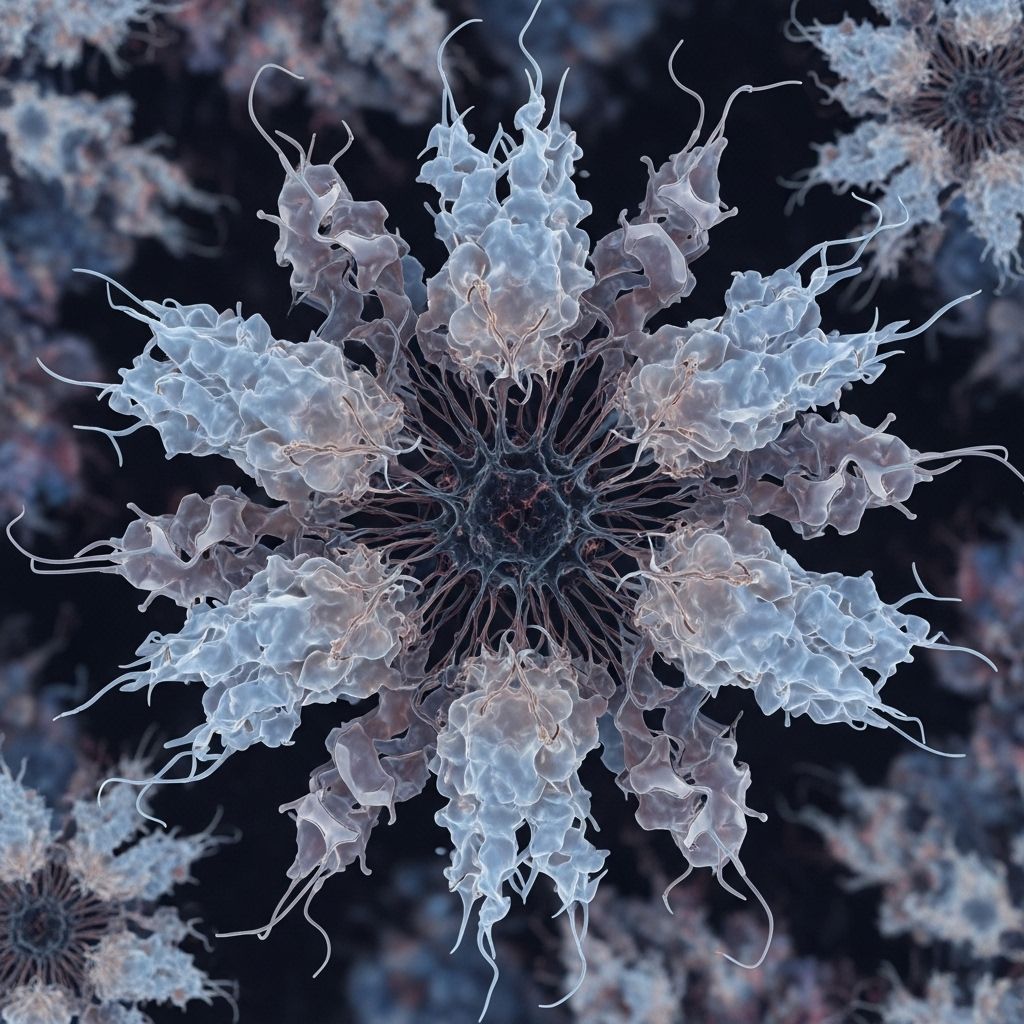
Prion diseases are a group of rare, progressive, and universally fatal disorders affecting the nervous system in both humans and animals. These conditions, also known as transmissible spongiform encephalopathies (TSEs), are caused by prions, which are infectious proteins leading to neurodegeneration and widespread brain damage. This article provides a comprehensive exploration of prion diseases, including their causes, manifestations, diagnostic processes, available treatments, and preventive strategies.
What are Prion Diseases?
Prion diseases are not caused by bacteria, viruses, or fungi, but instead result from prions—abnormally folded versions of the prion protein. These misfolded proteins can induce other normal prion proteins to adopt the abnormal form, resulting in exponential accumulation and damage within the brain and nervous system. Unlike typical infectious agents, prions lack nucleic acids, making them unique in pathogenicity.
- Transmissible spongiform encephalopathies (TSEs): The term covers prion diseases due to the sponge-like degeneration observed in the brains of affected individuals.
- Irreversible neurodegeneration: Prion accumulation leads to widespread neuronal death, ataxia, cognitive decline, and ultimately death.
- Universally fatal: There is no known cure, and all forms eventually lead to death.
How Prion Diseases Occur
Prions originate from a normal cellular prion protein called PrPC, found mainly in nervous tissue. Through a poorly understood trigger, PrPC converts to the abnormal form PrPSc, which has altered folding and properties:
- Abnormal folding: PrPSc is resistant to conventional methods of protein degradation.
- Inducing conversion: Misfolded PrPSc can convert nearby PrPC into PrPSc, propagating the disease process.
- No immune response: Because the primary structure remains unchanged, PrPSc does not provoke an immune reaction.
The rapid spread and neurotoxicity of prions are due to their unique infectious and self-propagating nature, resulting in severe brain damage and distinct clinical symptoms.
Types of Prion Diseases in Humans
Several human disorders are classified as prion diseases, distinguished by their clinical features and patterns of transmission:
- Creutzfeldt-Jakob Disease (CJD): The most common human prion disease. Mainly sporadic, but 10-15% of cases are genetic and some are acquired (iatrogenic or variant forms).
- Variant CJD: Linked historically to consumption of contaminated beef during the bovine spongiform encephalopathy (“mad cow disease”) outbreak.
- Kuru: Historically prevalent in Papua New Guinea, spread by ritual cannibalism.
- Gerstmann-Sträussler-Scheinker Syndrome (GSS): A rare inherited prion disease.
- Fatal Familial Insomnia (FFI): A genetic disorder presenting chiefly with sleep disturbances.
| Disease | Transmission Mode | Key Symptoms | Notes |
|---|---|---|---|
| Creutzfeldt-Jakob Disease (CJD) | Sporadic, genetic, iatrogenic | Rapid dementia, motor dysfunction | Most common prion disease in humans |
| Variant CJD | Consumption (infected beef) | Psychiatric, sensory, motor symptoms | Linked to BSE epidemic |
| Kuru | Consumption (ritual cannibalism) | Ataxia, tremors, neurodegeneration | Eradicated, historical significance |
| GSS | Genetic (PRNP mutations) | Ataxia, dementia | Rare familial disorder |
| FFI | Genetic (PRNP mutations) | Insomnia, dementia | Rare, severe sleep disorder |
Types of Prion Diseases in Animals
Prion diseases are also observed in several animal species, typically with lateral or foodborne transmission:
- Scrapie: Occurs in sheep and goats, causing ataxia and neurodegeneration.
- Bovine Spongiform Encephalopathy (BSE): Affects cattle and is known as “mad cow disease.” Consumption by humans can cause variant CJD.
- Chronic Wasting Disease (CWD): Impacts deer, elk, and moose; recent spread across North America and Europe has caused significant concern.
- Transmissible Mink Encephalopathy (TME): Affects mink, acquired through contaminated feed.
Symptoms and Clinical Presentation
Prion diseases present with rapidly progressive symptoms, typically involving neurological and psychiatric impairment:
- Dementia: Rapid mental decline with memory loss and behavioral changes.
- Motor Symptoms: Incoordination, muscle stiffness, tremors, and ataxia.
- Sensory Disturbances: Visual impairment, pain, abnormal sensations.
- Sleep Disorders: Insomnia or abnormal sleep cycles (especially in FFI).
- Psychiatric Symptoms: Anxiety, depression, hallucinations, personality changes (notable in variant CJD).
In most prion diseases, symptoms progress rapidly within months, leading to profound disability and death.
Diagnosis of Prion Diseases
Diagnostic Challenges
Due to the rarity of prion diseases and the similarity of their symptoms to other neurodegenerative disorders, diagnosis is complex and typically involves a combination of:
- Medical history and neurological examination
- Magnetic resonance imaging (MRI): May show characteristic brain changes
- Electroencephalogram (EEG): Irregular brain wave patterns seen in CJD
- Cerebrospinal fluid (CSF) testing: Identification of biomarkers such as 14-3-3 protein
- Genetic testing: Detection of mutations in the PRNP gene for inherited forms
- Brain biopsy/autopsy: The only definitive method for confirming diagnosis; post-mortem analysis is most reliable
No single test can definitively diagnose prion diseases prior to death, making early detection particularly challenging.
Causes, Risk Factors, and Transmission
- Sporadic mutations: Most cases of CJD arise without a clear cause.
- Genetic inheritance: Mutations in the PRNP gene can cause familial forms of prion disease.
- Acquired (infectious): Disease can result from exposure to prion-contaminated tissues through food (variant CJD), medical procedures (iatrogenic), or historical practices (kuru).
Animal prion diseases, such as BSE, scrapie, and CWD, are generally spread through direct contact with infected animals or ingestion of contaminated feed or tissue. The unpredictable species barriers and distribution of prions in different tissues complicate assessment of transmission risk.
Treatment Options
Currently, there is no cure or disease-modifying treatment available for prion diseases. The primary approach is palliative—focused on relieving symptoms and improving comfort:
- Supportive care: Includes pain management, control of psychiatric symptoms, and prevention of complications such as infections.
- Rehabilitative therapies: Physical, occupational, and speech therapies may assist in maintaining function as long as possible.
- Experimental approaches: Research into molecular mechanisms is ongoing in hopes of identifying potential therapeutic targets, but no effective treatments have yet reached clinical use.
Prevention Strategies
While inherited and sporadic forms of prion disease cannot be prevented, acquired cases may be reduced through careful public health measures and regulations:
- Food safety: Regulations limiting contamination of animal feed and food supply have reduced the risk of BSE-related variant CJD.
- Medical procedure protocols: Strict sterilization and avoidance of reusing surgical instruments on brain tissue minimize risk of iatrogenic transmission.
- Selective breeding and monitoring: Animal herds are monitored for signs of prion disease, and affected animals are culled to prevent spread in agriculture.
Outlook and Research Directions
Active research is dedicated toward developing diagnostic biomarkers, uncovering the molecular mechanisms of prion conversion, and discovering possible treatments. Despite advances in understanding prion biology, effective prevention and management depend heavily on vigilance in healthcare, agriculture, and food safety.
- Therapeutic targets: New research continues to highlight possible intervention points in prion replication and neurotoxicity.
- Global surveillance: Monitoring of both human and animal prion disease outbreaks is essential to control transmission and understand geographic spread.
Frequently Asked Questions (FAQs)
Q: What are prions?
A: Prions are infectious proteins that cause normally folded cellular prion protein (PrPC) to misfold into a disease-causing form (PrPSc), resulting in progressive degeneration of nervous tissue.
Q: Are prion diseases contagious like other infectious diseases?
A: Prion diseases are unusual in their mode of transmission. Most common forms are sporadic or inherited, but they can be acquired by exposure to infected tissue through food or medical procedures. Human-to-human transmission is extremely rare and requires direct exposure to prion-containing tissue.
Q: Can prion diseases be cured?
A: There are currently no cures for prion diseases. Treatment is limited to symptom management and supportive care, while research continues into possible interventions.
Q: Who is at risk for prion diseases?
A: Risk factors include age (incidence increases with age), genetic mutations (in familial forms), exposure to contaminated food or tissues, and, historically, cultural practices such as ritual cannibalism.
Q: How can prion diseases be prevented?
A: Prevention focuses on food safety, screening of medical procedures, and herd management in agriculture. Inherited and sporadic cases cannot be prevented.
Additional Information
- Incidence: Annual incidence of prion diseases in the U.S. is about 1.2 cases per million.
- Host specificity: Different strains of prion disease have unpredictable species barriers, complicating risk assessment.
Prion diseases, although rare, remain pivotal in neurodegenerative research due to their unique pathogenesis and public health implications. Improved awareness, vigilance, and research are crucial in managing their impact and advancing the quest for effective therapies.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9071098/
- https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540451/all/Prion_Diseases
- https://pubmed.ncbi.nlm.nih.gov/16168932/
- https://pure.johnshopkins.edu/en/publications/prion-diseases-13
- https://pure.johnshopkins.edu/en/publications/prion-diseases-11
- https://www.hopkinsguides.com/hopkins/search?catcode=479&st=OSS&search=Prion+Disease
- https://www.unmc.edu/healthsecurity/transmission/2023/12/12/prion-disease-rising-in-the-u-s/
Read full bio of Sneha Tete












