Understanding Nonalcoholic Fatty Liver Disease: Symptoms, Causes, Diagnosis, and Treatment
Unravel NAFLD: What it is, why it happens, how it’s diagnosed, and the strategies for effective management.
What is Nonalcoholic Fatty Liver Disease (NAFLD)?
Nonalcoholic fatty liver disease (NAFLD) is a condition in which excess fat builds up in the liver of people who consume little or no alcohol. Unlike other liver diseases associated with alcohol use, NAFLD primarily affects individuals with metabolic risk factors and has become one of the most common causes of chronic liver disease globally. NAFLD may remain silent, showing no clear symptoms, yet it can progress to more serious conditions that threaten overall health.
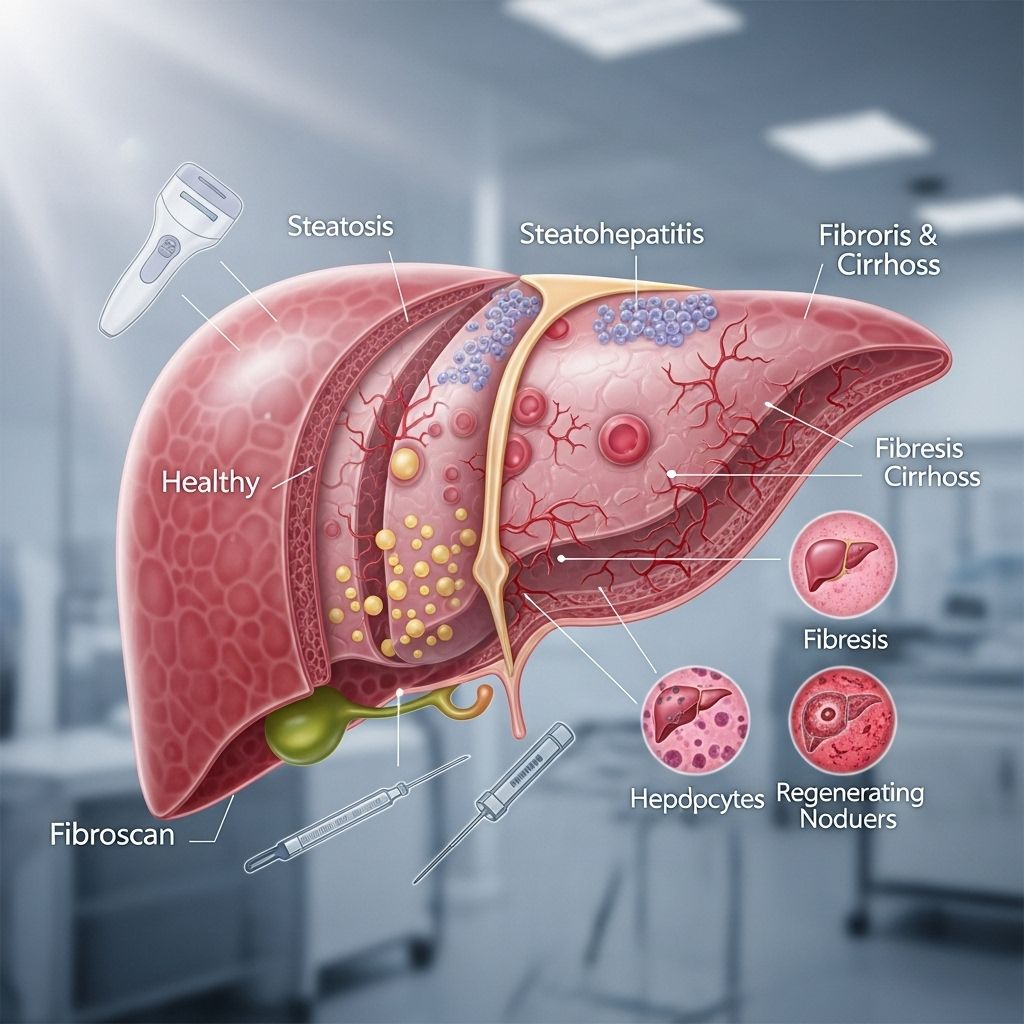
Types and Stages of NAFLD
The spectrum of nonalcoholic fatty liver disease includes two primary types, each representing different levels of severity:
- Nonalcoholic fatty liver (NAFL): This is the simple accumulation of extra fat in the liver without significant inflammation or liver cell damage. NAFL is considered relatively benign and less likely to progress to liver damage.
- Nonalcoholic steatohepatitis (NASH): In this form, fat accumulation is accompanied by liver inflammation and damage to liver cells. NASH can progress to advanced scarring (fibrosis), cirrhosis, liver failure, or in some cases, liver cancer.
NAFLD generally progresses through the following four stages:
| Stage | Description |
|---|---|
| 1. Fatty liver (steatosis) | Simple build-up of fat in the liver; no inflammation or damage. |
| 2. Nonalcoholic steatohepatitis (NASH) | Fat buildup causes inflammation and liver cell damage; risk of fibrosis begins. |
| 3. Fibrosis | The liver shows scar tissue, but still functions reasonably well. |
| 4. Cirrhosis | Severe scarring leads to poor liver function and potentially life-threatening complications. |
NAFLD vs. NASH: What’s the Difference?
While both NAFL and NASH fall under NAFLD, their impact differs:
- NAFL: Generally harmless, though it can progress in certain individuals.
- NASH: Higher risk of progressing to advanced liver disease due to ongoing inflammation and damage.
Most people remain at the simple steatosis stage, but a subset will progress to NASH and beyond.
Who Gets NAFLD?
NAFLD can affect anyone, including children and adults, but certain groups face a greater risk. It is particularly prevalent among individuals with conditions such as:
- Obesity (especially abdominal obesity)
- Type 2 diabetes
- Metabolic syndrome (a cluster of conditions that include high blood pressure, high blood sugar, high cholesterol, and excess abdominal fat)
- High cholesterol or triglycerides
- Insulin resistance or prediabetes
- Polycystic ovary syndrome (PCOS)
NAFLD is not restricted to overweight individuals. It may also occur in people who are not overweight or obese, including some children. Rapid weight loss and certain medications also contribute risk.
Causes and Risk Factors
The exact cause of NAFLD is not fully understood, but researchers believe it results from a combination of factors:
- Obesity: The single strongest risk factor.
- Type 2 diabetes and insulin resistance: Insulin resistance increases fat accumulation in the liver.
- High cholesterol and triglycerides: People with abnormal fat levels in the blood are at higher risk.
- High blood pressure: Often associated with NAFLD and metabolic syndrome.
- Poor diet or rapid weight loss: Crash diets, gastric bypass surgery, and nutritional imbalances may contribute.
- Certain medications: Drugs such as corticosteroids, calcium channel blockers, and some cancer therapies have been linked to NAFLD.
- Other conditions: Bowel diseases, polycystic ovary syndrome, or certain inherited metabolic conditions.
- Genetics: Family history appears to increase risk.
- Lack of exercise: Physical inactivity is a key lifestyle-related risk.
It is important to note that NAFLD can also develop in individuals who do not have any identified risk factors.
Symptoms of NAFLD
NAFLD is often known as a “silent” disease because most individuals experience few or no symptoms, especially in the early stages. When symptoms do occur, they may include:
- Persistent fatigue or general tiredness
- Pain or discomfort in the upper right abdomen (where the liver is located)
As NAFLD advances to NASH and cirrhosis, more noticeable and serious symptoms can develop:
- Weakness
- Loss of appetite
- Nausea
- Yellowing of the skin and eyes (jaundice)
- Itching
- Swelling in the legs and abdomen (edema, ascites)
- Mental confusion or difficulty concentrating (hepatic encephalopathy)
- Gastrointestinal bleeding
If you experience persistent fatigue, unexplained abdominal discomfort, or yellowing of the skin or eyes, seek medical attention for further evaluation.
Diagnosis of NAFLD
NAFLD is often discovered incidentally when liver blood tests are abnormal or during imaging studies for other health conditions. To confirm a diagnosis and evaluate disease severity, healthcare providers may employ several steps:
Medical History and Physical Exam
- Assessment of personal and family health history
- Review of risk factors including obesity, diabetes, and alcohol use
- Physical examination for signs of liver disease (e.g., enlarged liver, jaundice)
Blood Tests
- Liver function tests (ALT, AST): Elevated levels may signal liver inflammation.
- Blood count and clotting factors: May reveal complications in advanced disease.
- Tests for other liver diseases: To rule out viral hepatitis, autoimmune liver disease, and others.
Imaging Tests
- Ultrasound: Primary imaging study to detect liver fat.
- CT scan and MRI: Provide more detailed images.
- Elastography (e.g., FibroScan): Measures liver stiffness, helping to assess fibrosis versus simple fat accumulation.
Liver Biopsy
Occasionally, a liver biopsy may be recommended to precisely stage the disease, distinguishing between NAFL, NASH, and cirrhosis or to clarify the diagnosis when noninvasive tests are inconclusive. Biopsy remains the only definitive way to diagnose NASH and measure the extent of fibrosis.
Treatment and Management
There is currently no singular medical cure for NAFLD, but comprehensive management can prevent progression and sometimes reverse damage. Key elements include:
Lifestyle Changes
- Weight loss: Gradual, sustained weight loss of 7-10% of body weight can reduce fat, inflammation, and fibrosis (not rapid dieting).
- Healthy diet: Adopting a balanced diet low in saturated fats and added sugars, such as the Mediterranean diet.
- Physical activity: Aim for at least 150 minutes of moderate exercise per week.
- Alcohol avoidance: Limit or eliminate alcohol as it may worsen liver injury.
Medical Management
- Control of diabetes, high cholesterol, and high blood pressure: Essential for reducing disease progression risk.
- Medications: Although most medicines are not specifically approved for NAFLD, treating associated conditions (such as diabetes and high cholesterol) helps. A new drug, resmetirom (Rezdiffra), has been approved for adults with noncirrhotic NASH with moderate to advanced fibrosis.
- Vaccination: Immunizations for hepatitis A and B are recommended to prevent further liver strain.
- Therapeutic monitoring: Regular follow-up and monitoring for progression or complications.
Additional Steps
- Managing underlying conditions: Maintain control over diabetes, lipid levels, and blood pressure.
- Review all medications: Discuss all supplements, prescription, and over-the-counter medicines with your healthcare provider to avoid liver-toxic agents.
Complications of NAFLD
While many individuals with NAFLD have simple fatty liver and may never experience complications, progression can occur. Risks include:
- Cirrhosis: Extensive scarring leads to impaired liver function.
- Liver failure: Severe cases may result in loss of essential liver function.
- Liver cancer: Particularly hepatocellular carcinoma in cases of advanced NASH.
- Cardiovascular disease: NAFLD is associated with an increased risk of heart disease and stroke.
- Chronic kidney disease: Risk of kidney impairment is also higher among NAFLD patients.
Early identification and intervention are crucial to minimizing these risks.
Prevention of NAFLD
The best strategies to prevent NAFLD and its progression focus on healthy lifestyle habits:
- Maintain a healthy weight through balanced nutrition and regular exercise.
- Limit intake of sugar, refined carbohydrates, and saturated fats.
- Avoid excessive alcohol consumption.
- Monitor and control blood cholesterol, blood pressure, and blood sugar.
- See your healthcare provider regularly, especially if you have risk factors such as obesity or diabetes.
- Be proactive about vaccinations, especially for hepatitis viruses.
These steps not only help lower the risk for NAFLD but also contribute to general cardiovascular and metabolic health.
Frequently Asked Questions (FAQ)
Q: Is nonalcoholic fatty liver disease reversible?
A: In many cases, NAFLD—especially in its early stages—can be improved through weight loss, healthy diet, and increased physical activity. Advanced disease may be harder to reverse but slowing progression is often possible.
Q: Can NAFLD affect people who are not overweight?
A: Yes. Although more common in overweight and obese individuals, NAFLD can occur in people of normal body weight. Genetics, diet, or rapid weight loss may contribute.
Q: What foods are best for liver health if you have NAFLD?
A: A diet emphasizing vegetables, fruits, whole grains, lean proteins, and healthy fats (such as olive oil or nuts) is recommended. Avoid sugary beverages and processed foods high in saturated fat.
Q: Is medication necessary for all patients?
A: Not necessarily. Most cases are managed successfully through lifestyle changes. Specific medications may be considered for those with advanced fibrosis or additional risk factors, such as resmetirom for noncirrhotic NASH with fibrosis.
Q: How often should liver health be checked if you have NAFLD?
A: Regular monitoring as recommended by your healthcare provider is important to track disease progression and manage potential complications.
Resources and Support
- Discuss any concerns or symptoms with your healthcare provider promptly.
- Seek nutritional guidance to create a personalized, sustainable diet plan.
- Explore support groups or patient communities for resources and information.
Summary
Nonalcoholic fatty liver disease (NAFLD) is a growing health concern that can range from simple reversible fat accumulation to serious, potentially life-threatening liver damage. Early recognition, preventive strategies, and positive lifestyle modifications are foundational in managing NAFLD and preserving overall health. If you suspect you are at risk or have concerns about your liver, consult your healthcare provider for comprehensive evaluation and individualized care.
References
- https://medlineplus.gov/ency/article/007657.htm
- https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash
- https://www.pennmedicine.org/conditions/nonalcoholic-fatty-liver-disease
- https://www.nhs.uk/conditions/non-alcoholic-fatty-liver-disease/
- https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/symptoms-causes/syc-20354567
- https://my.clevelandclinic.org/health/diseases/15831-fatty-liver-disease
- https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/diagnosis-treatment/drc-20354573
- https://www.healthdirect.gov.au/fatty-liver
- https://www.aafp.org/pubs/afp/issues/2013/0701/p35.html/1000
Read full bio of medha deb












