Understanding Meningioma: Causes, Symptoms, Diagnosis, and Treatment
A comprehensive guide to meningioma—exploring risk factors, diagnosis, treatment options, and supportive care for this common brain tumor.
Understanding Meningioma
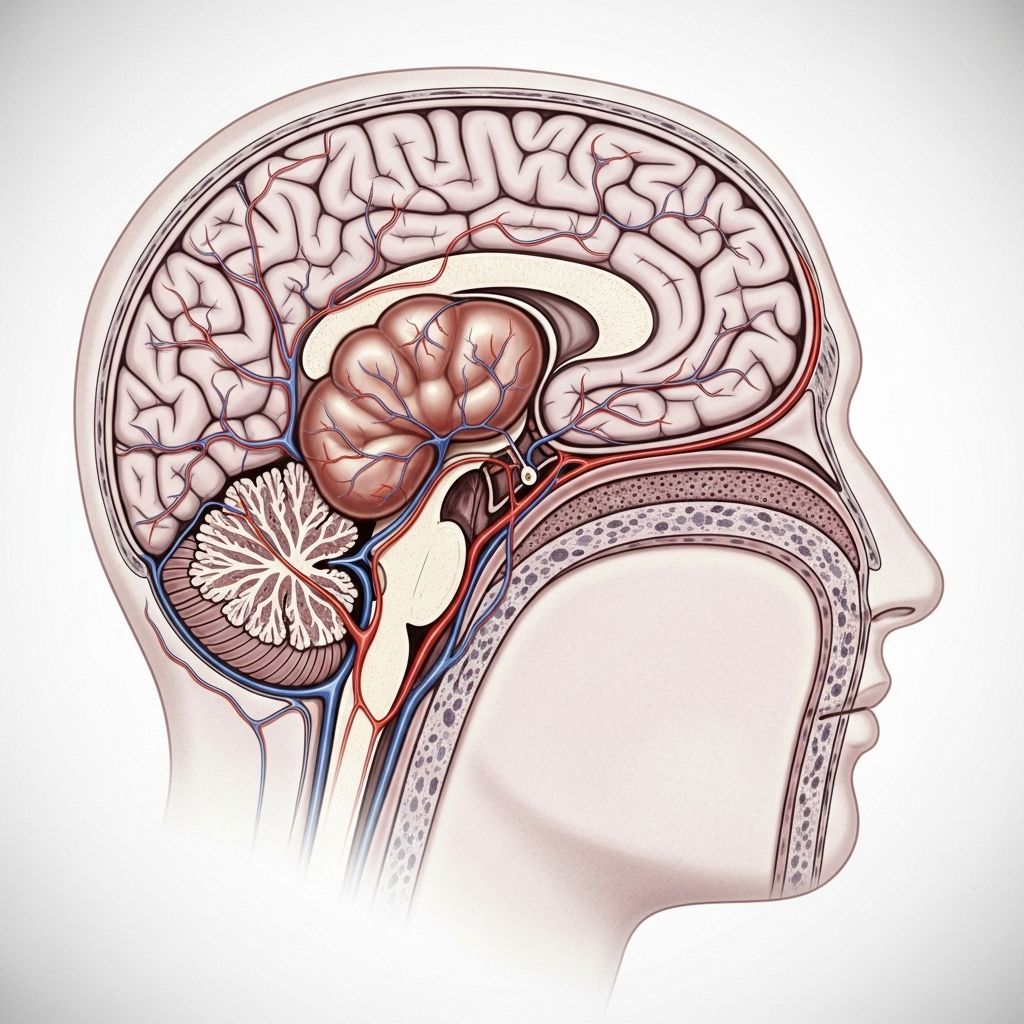
Meningioma is the most common type of primary brain tumor, typically arising from the meninges—the membranes that form the protective layers surrounding the brain and spinal cord. While most meningiomas are slow-growing and benign, their size and location can lead to significant neurological symptoms and require specialized treatment approaches. This article examines the core aspects of meningioma, including risk factors, symptoms, diagnosis, treatment options, and considerations for living with or after a meningioma diagnosis.
What Is a Meningioma?
A meningioma is a tumor that develops from the meninges, specifically the arachnoid cap cells of the dura mater. Meningiomas primarily occur in the brain, but can also develop along the spinal cord. While most meningiomas are benign (noncancerous), a small percentage can be atypical or malignant (cancerous and more aggressive).
- Meningiomas account for about 30% of all primary brain tumors.
- They are more commonly diagnosed in adults aged 40 to 70 years.
- Women are affected more often than men.
- Most meningiomas grow slowly and may remain asymptomatic for years.
Causes and Risk Factors
The precise cause of meningioma is not always clear, but several factors can increase a person’s risk of developing one.
- Age: Risk increases with age; most commonly diagnosed between ages 40 and 70.
- Gender: Women are two to three times more likely than men to develop meningiomas, suggesting hormonal influences.
- Hormonal Factors: Some meningiomas have hormone receptors (such as progesterone, estrogen, and androgen) and may grow during pregnancy or with hormone therapies.
- Genetic Conditions: Individuals with neurofibromatosis type 2 (NF2) have a higher risk due to a genetic mutation.
- Radiation Exposure: Previous radiation therapy to the head, especially during childhood, increases risk.
- Other Factors: Certain rare inherited syndromes and exposure to specific chemicals or toxins may also contribute to risk.
Symptoms of Meningioma
Symptoms depend on the tumor’s size, rate of growth, and location in the brain or spinal cord. Meningiomas can often remain undetected for years because they grow slowly and may not cause symptoms until they reach a significant size.
- Headaches—often persistent and progressively worsening
- Vision changes—such as double vision or loss of vision
- Hearing loss—or ringing in the ears (tinnitus)
- Weakness—in the arms or legs
- Seizures
- Memory problems or personality changes
- Difficulty with balance or coordination
- Numbness or tingling in limbs
- Nausea or vomiting (less common)
In rare cases, a meningioma may be discovered incidentally during brain imaging for an unrelated issue.
How Are Meningiomas Diagnosed?
Early diagnosis and precise characterization are crucial for guiding treatment. The diagnostic process typically includes:
- Medical History and Neurological Examination. Physicians begin with a detailed review of symptoms and a thorough neurological exam to assess changes in function.
- Imaging Tests:
- MRI (Magnetic Resonance Imaging): The gold standard for visualizing meningiomas—provides detail about size, location, and features of the tumor.
- CT Scan (Computed Tomography): Helpful, especially if MRI is unavailable or contraindicated, and better at visualizing calcifications within the tumor.
- Biopsy: In cases that are unclear or atypical, a biopsy may be performed—either via surgery or needle aspiration—to confirm the diagnosis.
Imaging findings characteristic of meningioma include a well-defined mass attached to the dura mater, often with a ‘dural tail’ sign on MRI.
Types and Grades of Meningioma
Meningiomas are classified based on their behavior, appearance under the microscope, and growth potential. The World Health Organization (WHO) has defined several grades:
| Grade | Description | Prevalence |
|---|---|---|
| Grade I (Benign) | Slow-growing, low likelihood of recurrence or aggressive behavior | ~80-85% |
| Grade II (Atypical) | Increased risk of rapid growth or recurrence; more aggressive | ~15-20% |
| Grade III (Anaplastic/Malignant) | Rapidly growing, invasive, higher recurrence rates | <5% |
There are also several subtypes based on pathological features, including meningothelial, fibrous (fibroblastic), transitional, and others. Grade II and III tumors may require more aggressive treatment due to higher recurrence risk and potential for spread.
Treatment Options for Meningioma
Treatment strategies depend on the tumor grade, location, size, growth rate, symptoms, and the patient’s overall health.
Surgery
Surgical removal is typically the first-line treatment for symptomatic or growing meningiomas. The goal is to achieve maximum safe resection—removal of as much of the tumor as possible without harming nearby brain tissue or cranial nerves.
- Complete resection is often possible for many benign meningiomas.
- Some tumors, especially those near critical structures (like the optic nerve or brain stem), require partial removal to avoid complications.
- The neurosurgeon may remove surrounding affected dura and bone to reduce risk of recurrence.
- Postoperative monitoring and follow-up imaging are essential to detect early recurrence.
Radiation Therapy
Radiation therapy is used when:
- The tumor cannot be completely removed surgically.
- The meningioma is recurrent, atypical (Grade II), or malignant (Grade III).
- Surgery is not feasible due to tumor location or patient health factors.
Types of radiation therapy include:
- External beam radiation: Delivers focused radiation from outside the body.
- Stereotactic radiosurgery: Uses highly focused, high-dose beams (such as Gamma Knife or CyberKnife) for smaller tumors or those in critical locations.
- Fractionated radiation: Spread over several sessions for larger or more sensitive locations.
Observation (Watchful Waiting)
Some small, slow-growing, and asymptomatic meningiomas may not require immediate treatment. Observation involves:
- Regular MRI or CT scans every few months or years to monitor tumor changes.
- Prompt intervention if the tumor grows or symptoms develop.
- Frequently recommended for older adults with stable, non-problematic lesions.
Medications and Other Therapies
- There are currently no approved medications that can cure meningioma.
- Medications may be used to manage symptoms such as seizures (anticonvulsants), swelling (corticosteroids), or headaches (pain relievers).
- Experimental therapies or clinical trials may be considered for recurrent or aggressive forms.
Deciding on the Right Treatment
Treatment planning is highly individualized. Multidisciplinary teams—including neurologists, neurosurgeons, radiation oncologists, and radiologists—collaborate to develop recommendations tailored to the patient. Considerations include:
- Tumor size, grade, and location
- Symptoms and overall health
- Potential impact on neurological function and quality of life
- Risks and benefits of each treatment option
- Patient preferences and lifestyle factors
In some cases, a ‘second opinion’ may be helpful to ensure a comprehensive review of all potential management strategies.
Prognosis and Life After Meningioma Treatment
Most patients with benign meningiomas experience positive outcomes and can live normal or near-normal lives after treatment. However, prognosis may vary based on:
- Tumor grade and subtype
- Completeness of tumor removal
- Recurrence or spread (especially for atypical or malignant types)
- Location of tumor and effects on neurological function
Some patients may require long-term follow-up, regular imaging, or additional treatments if the tumor recurs or changes over time.
Potential Complications
- Recurrence: Even after treatment, meningiomas can recur—especially atypical or malignant forms.
- Neurological Deficits: Depending on the tumor’s location, some patients may experience permanent or temporary issues such as vision loss, weakness, speech difficulties, or memory problems.
- Side Effects of Treatment: Surgery and radiation may cause swelling, infections, or other complications, though these are often well-managed by the care team.
Support and Coping
A meningioma diagnosis can feel overwhelming. Comprehensive care includes:
- Rehabilitation: Physical, occupational, or speech therapy as needed after surgery or radiation
- Counseling and support groups for emotional well-being
- Educational resources for patients and families to better understand the condition
- Close communication with the medical team for monitoring and management of any new symptoms
Prevention and Reducing Risk
- There is no guaranteed way to prevent meningioma, due to its unclear causes.
- Avoid unnecessary exposure to radiation, especially during childhood.
- Discuss any family history of genetic conditions (such as NF2) with a healthcare provider.
- Report persistent neurological symptoms early for prompt evaluation.
Frequently Asked Questions (FAQs)
Q: Is a meningioma cancerous?
A: The vast majority of meningiomas are benign (noncancerous), though a small percentage are atypical or malignant and may behave more aggressively.
Q: Can meningiomas spread to other parts of the body?
A: Malignant meningiomas can rarely spread (metastasize), but most do not. The risk is highest with WHO Grade III tumors.
Q: Are all meningiomas treated with surgery?
A: Not always. Observation is often appropriate for small, asymptomatic tumors, particularly in older individuals or if the tumor is in a surgically challenging location.
Q: Can meningiomas return after treatment?
A: Yes. Recurrence is more common with atypical and malignant meningiomas, and in cases where the tumor could not be fully removed. Close follow-up is essential.
Q: What is the long-term outlook for someone with a meningioma?
A: Outlook is generally excellent for benign meningiomas, with many patients living healthy lives after treatment. Higher-grade meningiomas require more aggressive follow-up and management.
When to See a Doctor
- Persistent headaches, vision changes, seizures, or neurological symptoms should prompt a medical evaluation.
- Individuals with a known history of neurofibromatosis or prior head radiation should report new neurological symptoms immediately.
- Timely diagnosis and intervention can minimize complications and improve outcomes.
Resources and Support
For more information and support, consider reaching out to specialized brain tumor centers, patient advocacy organizations, or local/neuro-oncology programs. Many hospitals also offer resources for caregivers and family members to help manage the challenges associated with meningioma diagnosis and treatment.
References
Read full bio of medha deb












