Understanding Lymphadenitis: Causes, Symptoms, Diagnosis, and Treatment
Your comprehensive guide to recognizing, diagnosing, treating, and preventing lymphadenitis and its complications.
Lymphadenitis is a common medical condition that affects thousands of people every year, often manifesting as swollen, painful lymph nodes. This comprehensive guide will help you understand what lymphadenitis is, what causes it, how to recognize its symptoms, which diagnostic tools are available, the various treatment options, prevention techniques, and ways to manage life with this condition.
What is Lymphadenitis?
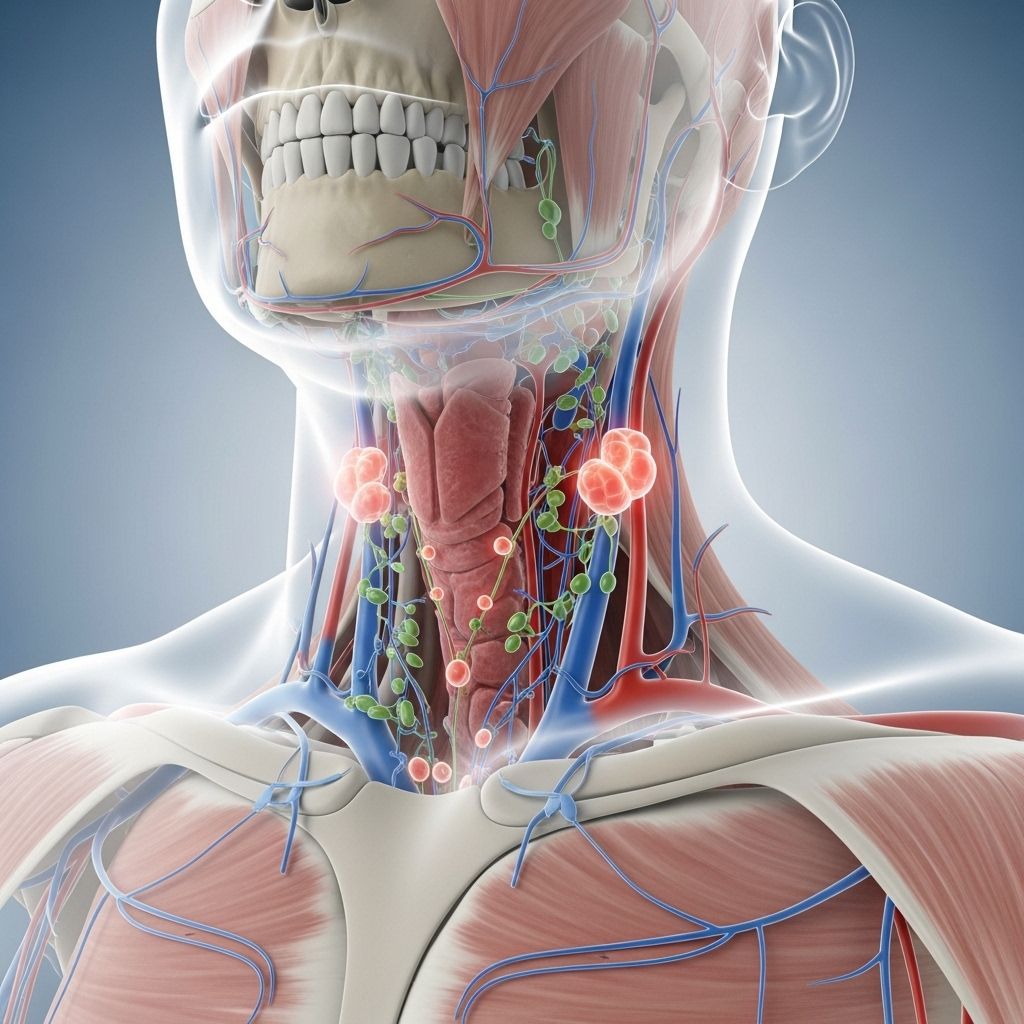
Lymphadenitis refers to the inflammation or infection of the lymph nodes, which are also known as lymph glands. These structures are an essential part of the lymphatic system and support the immune system’s functions by filtering out harmful substances. When lymph nodes become infected, typically by bacteria, viruses, or fungi, they swell, become tender, and may cause significant discomfort.
Alternative Names
- Lymph node infection
- Lymph gland infection
- Localized lymphadenopathy
The Lymphatic System: A Brief Overview
The lymphatic system is a network that includes lymph nodes, ducts, vessels, and organs. It acts as a major component of the immune system, with lymph nodes acting as filters and storage sites for white blood cells that help fight infection and disease. Any part of this system can experience infection or inflammation, but lymphadenitis refers specifically to the nodes.
Causes of Lymphadenitis
Lymphadenitis occurs when pathogens infiltrate lymph nodes, leading to irritation and inflammation. The most frequent causes are:
- Bacterial infections: Common bacteria such as Staphylococcus aureus and Streptococcus pyogenes are leading culprits, often entering the body through breaks in the skin or other infections nearby.
- Viral infections: Viruses like those causing the common cold, influenza, or other systemic viral illnesses may also trigger lymphadenitis.
- Fungal and parasitic infections: Though rare, certain fungi and parasites can infect lymph nodes and result in inflammation.
- Other causes: Less commonly, lymphadenitis can be secondary to more unusual infections (e.g., tuberculosis, cat scratch disease from Bartonella henselae), or as a reaction to certain immune responses, malignancies, or autoimmune conditions.
Pathway of Infection
An infection often begins somewhere in the body (such as the skin) and travels to the nearest group of lymph nodes, which then swell and become tender as they filter and attempt to destroy the invading microorganisms. Lymphadenitis most frequently occurs near the area of an initial infection. For example, a skin infection on a hand may cause swelling of lymph nodes in the elbow or underarm.
Types of Lymphadenitis
- Localized lymphadenitis: Involves one group or cluster of lymph nodes close to the site of infection.
- Generalized lymphadenitis: Affects lymph nodes in multiple areas, which may suggest a more systemic illness.
Symptoms of Lymphadenitis
The hallmark symptoms of lymphadenitis typically appear near the affected node(s). These include:
- Swollen lymph nodes: A node is considered enlarged if it is about 1/2 inch wide or more.
- Pain or tenderness: Affected nodes are often sore or painful to touch.
- Skin changes: The skin over the lymph node may be red, warm, or tender. In severe cases, cellulitis or red streaks may appear.
- Fever and chills: Especially if the infection is more severe or becomes systemic.
- Nodes may feel rubbery: Especially if an abscess (a collection of pus) forms, the nodes can become firm, soft, or even stuck together (matted).
- Fluid drainage: In advanced cases, pus or other fluid may drain through the skin, indicating an abscess.
- Other symptoms: Depending on the underlying cause, people may also experience fatigue, night sweats, or general malaise.
Diagnosing Lymphadenitis
Diagnosis often begins with a detailed medical history and a physical examination of affected areas. The following steps and tests may be involved:
- Physical examination: Palpating the lymph nodes for size, tenderness, mobility, and evaluating for overlying skin changes.
- History taking: Assessing for recent infections, skin injuries, animal exposures (e.g., cat scratch), travel, or systemic symptoms.
- Blood tests: Such as a complete blood count (CBC) to assess for infection or inflammation markers.
- Cultures: A sample (aspirate) from the lymph node, pus or surrounding tissue may be cultured to identify the causative organism.
- Biopsy: In certain cases, especially when malignancy or unusual processes are suspected, a part of or an entire lymph node may be surgically removed for histologic examination.
- Imaging studies: Techniques like ultrasound or CT scan may be recommended for deeper or difficult-to-access lymph nodes, or if an abscess or malignancy is suspected.
When to Seek Medical Attention
- If swelling, pain, and redness in a lymph node area do not resolve or worsen over a few days.
- If fever is high or persists.
- If you notice pus or fluid draining from under the skin near a swollen gland.
Treatment for Lymphadenitis
Treatment depends heavily on the underlying cause of infection and the severity of the condition. The primary goals are to eliminate the infection, relieve symptoms, and prevent complications.
Medical Treatments
- Antibiotics: The most common treatment for bacterial lymphadenitis. Empirical antibiotics are often started while awaiting culture results and may target common bacteria like Staphylococcus aureus and Streptococcus pyogenes.
- Antivirals or antifungals: Used if the infection is caused by a virus or fungus, respectively. This is less common than bacterial lymphadenitis.
- Pain control: Medicines such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may help with pain and fever.
- Surgical drainage: If an abscess has formed in the lymph node, a surgical procedure might be needed to drain the pus.
- Supportive care: Applying warm, moist compresses may reduce pain and swelling. Elevation of the affected limb and rest are also helpful adjuncts.
Inpatient vs. Outpatient Care
- Outpatient care: Most patients respond well to oral medications at home if the infection is mild and there are no complications.
- Inpatient care: Hospital admission may be needed if the infection is severe, there are multiple abscesses, the patient is immunocompromised, or in children, where intravenous (IV) antibiotics can be administered safely.
Prognosis and Possible Complications
With prompt and appropriate treatment, most cases of lymphadenitis resolve quickly. However, complications can occur if the infection is not adequately treated or if the individual is immunocompromised.
- Abscess Formation: Pockets of pus within lymph nodes may require surgical drainage.
- Sepsis: If the infection spreads to the bloodstream, it can cause systemic illness.
- Chronic lymphadenopathy: Some lymph nodes may remain enlarged or firm long after the infection has resolved.
- Tissue scarring: Especially if abscesses have been present.
Prevention of Lymphadenitis
Reducing the risk of lymphadenitis revolves around infection prevention and early treatment of any illness or injury:
- Good hygiene: Wash hands regularly and thoroughly.
- Immediate care for skin injuries: Cleanse cuts, scrapes, and bites prompted and apply antiseptics when needed.
- Early treatment: Address new infections aggressively, especially those of the skin.
- Animal scratch and bite precautions: Take care when interacting with animals, and properly treat any bites or scratches.
- Immune maintenance: For individuals with weakened immune systems, work with healthcare providers to prevent and monitor infections closely.
Living with Lymphadenitis
Most people recover fully from lymphadenitis with the proper treatment. However, some may experience prolonged swelling or discomfort. Managing the condition at home typically involves:
- Adhering to medication regimens: Take all prescribed antibiotics or other medications exactly as directed.
- Monitoring symptoms: Note any changes in size, color, or pain in lymph nodes and inform your healthcare provider about persistent or worsening symptoms.
- Physical care: Use warm compresses on the affected area to aid with symptom relief; elevate the affected limb to reduce up swelling.
- Regular follow-up: Attend all scheduled medical appointments to monitor your progress and catch any complications early.
- Avoid over-the-counter medications: Do not take new over-the-counter pain or fever medicines without consulting your healthcare provider.
Frequently Asked Questions (FAQs) about Lymphadenitis
What is the difference between lymphadenitis and lymphadenopathy?
Lymphadenitis specifically refers to inflammation of the lymph nodes due to infection, while lymphadenopathy is a broader term encompassing any disease or enlargement of lymph nodes, regardless of cause (infection, malignancy, immune disorders).
Is lymphadenitis contagious?
Lymphadenitis itself is not contagious, but the underlying infection (such as a bacterial or viral illness) may be, depending on its cause.
How long does lymphadenitis last?
With timely treatment, most cases improve within several days to a week. Some lymph nodes may remain slightly enlarged for a longer period, even after the infection clears.
Can lymphadenitis return?
Yes, if the underlying causes persist or are not adequately addressed, lymphadenitis can recur in the same or different lymph node regions.
When should I see a doctor for swollen lymph nodes?
If you notice persistent swelling, increasing pain, redness, fever, or pus draining from a lymph node region, seek medical care. Early intervention leads to a better outcome and less risk of complications.
Summary Table: Lymphadenitis at a Glance
| Aspect | Details |
|---|---|
| Common Causes | Bacterial (Staph, Strep), viral, fungal, and rarely, parasitic infections |
| Most Affected Areas | Neck, underarm, groin, behind ears, under the chin |
| Main Symptoms | Swollen, tender lymph nodes; redness; fever; sometimes pus |
| Diagnostic Tools | Physical exam, blood tests, cultures, biopsy, imaging |
| Treatment | Antibiotics/antivirals/antifungals, drainage of abscesses, pain control |
| Prevention | Good hygiene, quick treatment of infections, proper wound care |
| Potential Complications | Abscess, sepsis, chronic enlargement, scarring |
Key Takeaways
- Lymphadenitis is usually a treatable condition, but it can become serious if not managed promptly.
- Recognizing and treating infections early reduces the risk of lymphadenitis and its complications.
- Practice good hygiene and care of wounds to help prevent this condition.
- Contact your healthcare provider if you experience persistent, painful, or worsening swelling in your lymph nodes.
References
- https://www.merckmanuals.com/professional/dermatologic-disorders/bacterial-skin-infections/lymphadenitis
- https://medlineplus.gov/ency/article/001301.htm
- https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=134&contentid=80
- https://ufhealth.org/conditions-and-treatments/lymphadenitis
- https://www.mayoclinic.org/diseases-conditions/swollen-lymph-nodes/symptoms-causes/syc-20353902
- https://my.clevelandclinic.org/health/diseases/17890-mesenteric-lymphadenitis
- https://www.aafp.org/pubs/afp/issues/2016/1201/p896.html
- https://www.mayoclinic.org/diseases-conditions/swollen-lymph-nodes/diagnosis-treatment/drc-20353906
Read full bio of medha deb












