Understanding Intestinal Obstruction: Causes, Symptoms, and Treatment
Learn the causes, symptoms, diagnosis, and treatments for intestinal obstruction and essential steps for managing this serious condition.
Understanding Intestinal Obstruction
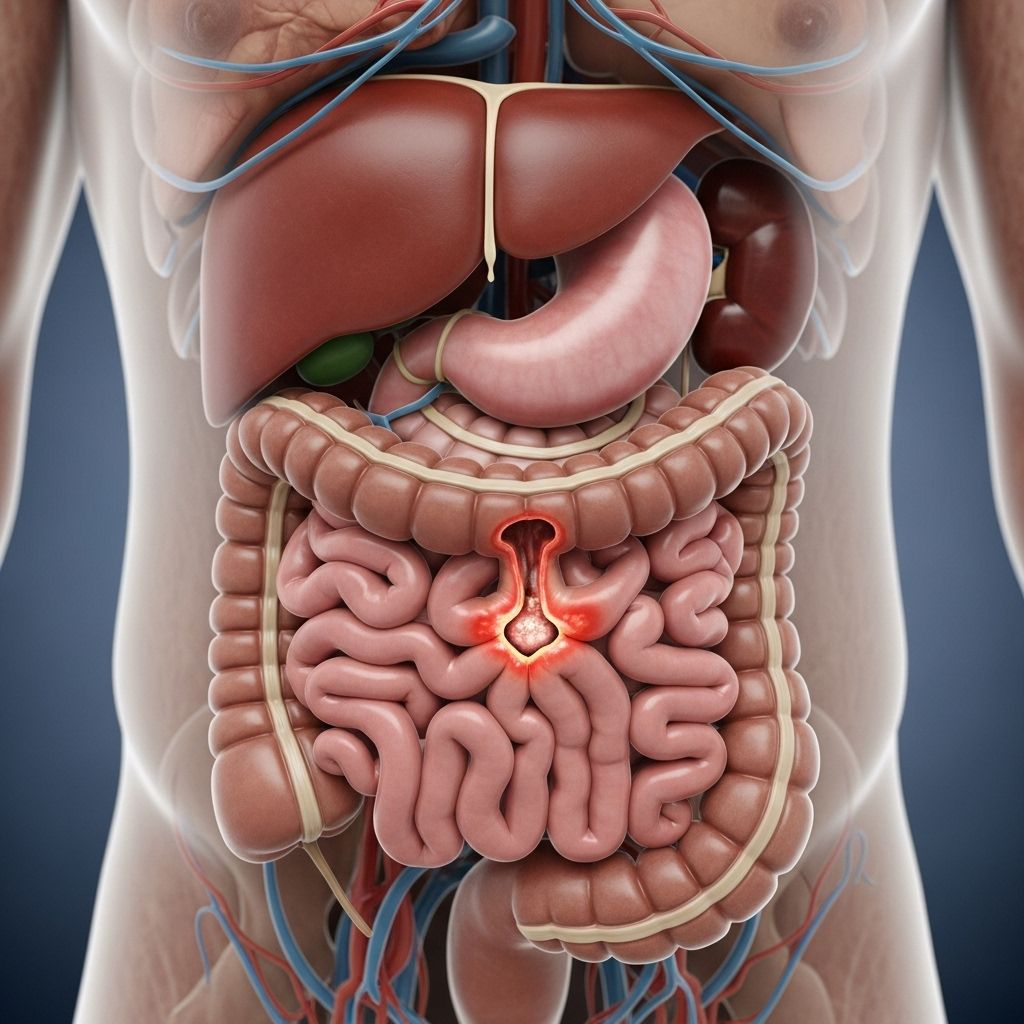
Intestinal obstruction is a serious medical condition characterized by a blockage that prevents the normal movement of food, liquid, and gas through the small or large intestine. This disruption in digestive flow can cause significant health problems and requires prompt medical attention to avoid dangerous complications.
Category: Digestive Disorders
What Is Intestinal Obstruction?
An intestinal obstruction refers to the partial or complete blockage of the bowel. This blockage halts the passage of digestive contents through the intestines, leading to inflated discomfort, pain, and other gastrointestinal symptoms. Obstructions can occur in either the small intestine or the large intestine (colon), and are classified by their cause as either mechanical or functional (ileus).
Main Types of Intestinal Obstruction
- Mechanical Obstruction: Involves a physical blockage (such as a tumor, scar tissue, or twisted intestine) that impedes passage through the bowel.
- Ileus (Functional Obstruction): The intestine stops moving due to nerve or muscle dysfunction, not a physical barrier.
Anatomy: The Role of the Intestines
The small intestine and colon are vital components of the digestive tract. They absorb nutrients from food and move remaining waste for excretion. Any obstruction disrupts nutrient absorption and waste elimination, leading to an accumulation of intestinal contents and subsequent swelling and pain.
Symptoms of Intestinal Obstruction
Symptoms develop because digestive contents are trapped behind the blockage, leading to a buildup of pressure and inflammation. Key signs and symptoms include:
- Abdominal pain and cramping, often intermittent and severe
- Abdominal swelling (distention)
- Loss of appetite
- Constipation and/or inability to pass gas
- Nausea and vomiting
- Diarrhea (rare, but possible if only partial blockage exists)
- Breath odor due to backup of intestinal contents
Signs to Seek Immediate Medical Care
- Severe abdominal pain
- Persistent vomiting
- Swelling accompanied by constipation and inability to pass gas
- Signs of infection or fever
If you notice any of these symptoms, prompt diagnosis and treatment are essential, as prolonged obstruction can lead to tissue death and life-threatening complications.
Causes of Intestinal Obstructions
Intestinal obstruction can result from a wide range of causes, both mechanical and functional:
- Adhesions (scar tissue from previous surgery)
- Hernias (bowel protrudes into another area)
- Tumors (especially colon cancer)
- Strictures (narrowing due to inflammation, e.g., Crohn’s disease or diverticulitis)
- Foreign bodies (swallowed objects)
- Gallstones (rare)
- Impacted stool
- Intussusception (one bowel segment telescopes into another)
- Volvulus (twisting of the intestine)
- Infections, electrolyte, or mineral imbalances
- Use of narcotic medications
Special Considerations
- Paralytic Ileus commonly seen in infants, children, and following abdominal surgery or infections.
- Cancer can directly block intestines, necessitating special management (e.g., stents, gastrostomy tubes).
How Is Intestinal Obstruction Diagnosed?
Early diagnosis is critical to prevent complications. Diagnostic steps typically include:
- Physical Examination: Detects swelling, tenderness, distention, and sometimes palpable masses or hernias.
- Imaging Tests:
- Abdominal X-ray: Reveals air-fluid levels, dilated bowel loops.
- Abdominal CT Scan: Detailed images to distinguish mechanical from functional obstruction.
- Barium Enema: Contrast study to assess colon blockage.
- Upper GI and Small Bowel Series: Contrast study of the upper digestive tract.
- Laboratory Tests: May detect infection, inflammation, or electrolyte imbalances.
Complications of Untreated Obstruction
- Bowel perforation
- Tissue death (necrosis)
- Serious infections (such as peritonitis or sepsis)
- Organ failure due to infection and electrolyte imbalance
Prompt treatment significantly reduces these risks.
Treatment Options for Intestinal Obstruction
Treatment depends on the type, severity, and cause of the obstruction, but always requires hospitalization for acute symptoms. Common interventions include:
- Nasogastric Tube: Inserted through the nose to drain fluids and relieve pressure, helps manage nausea and vomiting.
- IV Fluids: Restore hydration and electrolytes, especially if vomiting and diarrhea occur.
- Bowel Rest: Halting eating and drinking allows the intestine a chance to clear the obstruction and heal.
- Patients may receive nutrition via intravenous routes during this period.
- Stent Placement: Mesh tube inserted into the intestine to temporarily open blocked segments, often used in cancer-related blockages.
- Medications:
- Antibiotics if infection is present.
- Antinausea and pain medicines.
- Surgery: Required for complete obstruction, tissue death, or failure of conservative treatments. Surgery removes or bypasses the blockage, repairs damage, and may include removal of tumors or scar tissue.
- Gastrostomy Tube: Direct tube from the abdomen into the stomach for drainage, mainly used in cancer-related obstructions.
Treatment by Cause Table
| Cause | Most Common Treatment Approach |
|---|---|
| Adhesions | Nasogastric tube, surgery if persistent |
| Cancer/Tumors | Stent, surgery, gastrostomy tube |
| Hernias | Surgery |
| Intussusception | Barium enema (children), surgery (adults) |
| Volvulus | Tube via rectum, surgery |
| Ileus | Bowel rest, IV fluids, treat underlying condition |
Recovery and Prognosis
- Many obstructions resolve successfully after treatment.
- Outcome depends on the cause—the prognosis is better for partial, short-duration, and non-cancer cases.
- Prompt recognition and intervention improve survival and reduce complications.
Preventing Intestinal Obstruction
- Maintain a healthy diet with adequate fiber to avoid impacted stool.
- Regular physical activity encourages bowel motility.
- Careful management of chronic conditions, such as Crohn’s disease, can reduce risk.
- Follow medical instructions after abdominal surgery to minimize scar formation.
While prevention is not always possible for all causes, these steps may reduce risk for some individuals.
Frequently Asked Questions (FAQs)
Q: How do I know if I have an intestinal obstruction?
Symptoms such as severe abdominal pain, distention, inability to pass gas, vomiting, and constipation may suggest an obstruction. Contact a healthcare provider for diagnosis if you suspect symptoms.
Q: Are all obstructions treated with surgery?
No. Many partial obstructions are managed with nonsurgical interventions such as nasogastric tube, IV fluids, and bowel rest. Surgery is reserved for complete, persistent, or complicated cases.
Q: What should I expect during diagnosis?
Diagnosis typically involves a physical exam, imaging studies (x-ray, CT scan, or barium studies), and blood tests to assess complications.
Q: Can intestinal obstruction be fatal?
If left untreated, obstruction can cause bowel tissue death, perforation, infection, and even death. Timely medical attention is crucial.
Q: Will I need a stoma or permanent bag after surgery?
Rarely, if the damage is severe or extensive portions of bowel are removed, a temporary or permanent stoma may be needed. This is decided based on operative findings and your condition.
Key Takeaways
- Intestinal obstruction is a medical emergency requiring prompt evaluation and intervention.
- Common symptoms include pain, swelling, nausea, vomiting, and inability to pass stool or gas.
- Treatment may be nonsurgical or surgical, depending on the cause and severity.
- Mechanical and functional types differ in management and risk.
- Prevention strategies involve healthy lifestyle choices and condition management.
References
- Information adapted from authoritative clinical resources, including Mayo Clinic, MedlinePlus, WebMD, and the National Cancer Institute.
References
- https://www.mayoclinic.org/diseases-conditions/intestinal-obstruction/symptoms-causes/syc-20351460
- https://medlineplus.gov/ency/article/000260.htm
- https://www.webmd.com/digestive-disorders/what-is-bowel-obstruction
- https://www.cancer.gov/about-cancer/treatment/side-effects/bowel-obstruction
- https://www.mayoclinic.org/diseases-conditions/intestinal-obstruction/diagnosis-treatment/drc-20351465
- https://my.clevelandclinic.org/health/diseases/bowel-obstruction
- https://www.nyp.org/digestive/bowel-obstruction
- https://www.merckmanuals.com/home/digestive-disorders/gastrointestinal-emergencies/intestinal-obstruction
Read full bio of Sneha Tete












