Understanding Heart Disease: Causes and Risk Factors
A comprehensive guide to the genetic, lifestyle, and health-related factors that shape your heart disease risk.
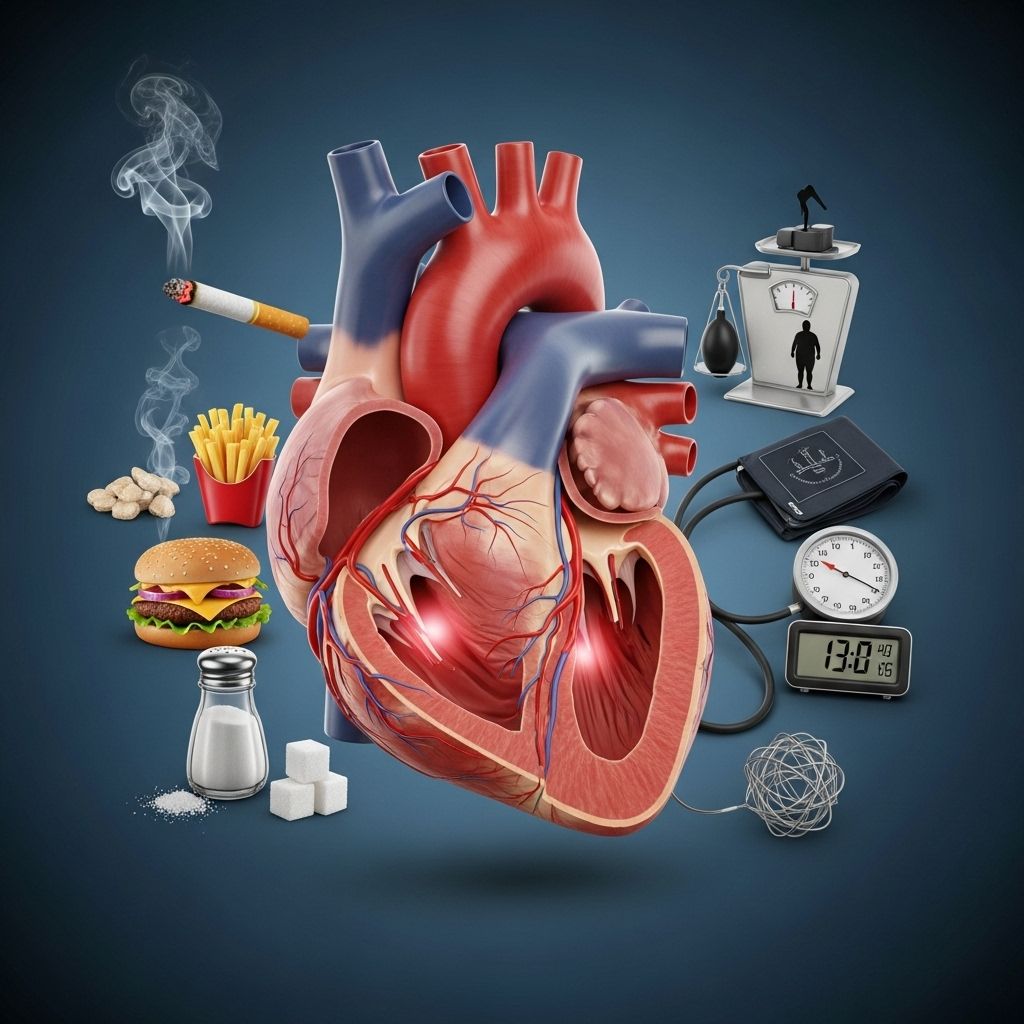
Heart disease remains the leading cause of death among adults around the world. Though commonly known as coronary heart disease (CHD) or cardiovascular disease, the umbrella term ‘heart disease’ covers several conditions affecting the functioning of your heart and blood vessels. The most prevalent form is caused by the build-up of plaque within the arteries, restricting the flow of oxygen-rich blood to this vital organ. But what causes this build-up? Who is at greatest risk? This comprehensive guide unpacks the multiple causes and risk factors involved, so you can take informed steps to safeguard your heart health.
What Is the Main Cause of Heart Disease?
At its core, heart disease most often results from the gradual accumulation of plaque—a waxy substance composed of cholesterol, fatty molecules, and minerals—on the inner walls of your arteries. This process, known as atherosclerosis, narrows and hardens the arteries over time, eventually restricting or even blocking the supply of blood and essential nutrients to the heart muscle. Common factors that damage your arteries and accelerate plaque formation include high blood pressure, high cholesterol, smoking, and elevated triglyceride levels.
How Do Genetics and Family History Influence Heart Disease Risk?
Your family history and genetic makeup play a major role in your likelihood of developing heart disease, particularly at a younger age. Scientific studies have shown that inheriting certain genetic traits can double or even triple your risk—especially when combined with unhealthy lifestyle habits like poor diet or smoking.
Key points about genetics and heart disease risk:
- If you have a male parent who had heart disease, your risk is slightly higher compared to if only a female parent is affected. Having a sibling with heart disease—especially a twin—further increases risk.
- Specific inherited genes may impact how your body manages cholesterol, inflammation, and blood vessel health.
- Relatives who experienced heart disease at a young age (male before 55, female before 65) signal a particularly strong genetic component.
- When your family history is combined with modifiable lifestyle factors (such as diet, activity, and substance use), the overall risk multiplies.
Demographic Factors: Age, Sex, and Ethnicity
Some risk factors for heart disease cannot be changed. These include:
- Age: Risk increases as you get older, with most cases occurring in people over 65.
- Sex: Men have a higher risk of heart disease at a younger age; however, women’s risk rises and may catch up post-menopause.
- Ethnicity: Non-Hispanic Black, non-Hispanic white, and people of Asian or Pacific Islander heritage generally face a higher risk than Native Alaskan or Native American populations.
While these factors cannot be controlled, knowing your personal risk can help you and your healthcare provider build a better prevention plan.
Common Medical Conditions That Increase Heart Disease Risk
Several health conditions substantially boost your likelihood of developing heart disease. Being aware of these can guide your efforts to minimize risk:
- High Blood Pressure (Hypertension): Often called the “silent killer,” high blood pressure silently damages the artery walls, making plaque build-up and artery narrowing more likely. Even without obvious symptoms, untreated hypertension is a leading risk factor for heart attacks and heart failure.
- High Cholesterol (Especially LDL): An abundance of low-density lipoprotein (LDL, “bad cholesterol”) in the bloodstream encourages plaque formation. In contrast, high-density lipoprotein (HDL, “good cholesterol”) helps clear cholesterol from arteries. Imbalanced levels are closely tied to heart disease development.
- High Triglycerides: These blood fats, commonly elevated with poorly controlled diabetes or unhealthy diets, also increase the risk of atherosclerosis and related complications.
- Diabetes (Especially Type 2): People with diabetes are up to twice as likely to develop heart disease or have a stroke, often at a younger age. Poorly managed blood glucose damages blood vessel linings and accelerates plaque build-up. Insulin resistance—a hallmark of type 2 diabetes—exacerbates the risk, further increasing the likelihood of heart attacks.
- Obesity: Carrying excess body fat is directly related to high blood pressure, diabetes, high cholesterol, and systemic inflammation—all of which make heart disease more probable.
- Depression: Chronic depression or high stress does more than reduce quality of life. It raises blood pressure, increases inflammation (measured by C-reactive protein, or CRP), and may trigger unhealthy behaviors—all combining to heighten the risk of heart disease and poor outcomes following a cardiac event.
Other Health Conditions and Situational Risks
- Sleep apnea and chronic sleep deprivation can increase blood pressure and heart strain.
- Chronic kidney disease, inflammatory conditions, and certain cancers may also add to risk by affecting metabolism, vascular health, and systemic inflammation.
Lifestyle Factors: Choices That Affect Heart Disease Risk
Your daily habits have a huge impact—possibly the largest single influence—on whether you develop heart disease. The following lifestyle factors are among the most significant:
- Poor Diet: Eating foods high in saturated fat, trans fats, refined sugars, and excess salt can lead to high cholesterol, hypertension, and obesity. In contrast, a diet high in fiber, fruits, vegetables, lean protein, and healthy fats helps protect cardiovascular health.
- Lack of Physical Activity: Low levels of exercise or an entirely sedentary lifestyle increase the risk of developing obesity, high blood pressure, high cholesterol, and diabetes. Regular aerobic activity (like brisk walking, jogging, or cycling) helps control many risk factors.
- Tobacco Use (Smoking): Cigarette smoking and even secondhand smoke damage blood vessels, raise blood pressure, and promote plaque formation. Smokers are twice as likely to develop heart disease as non-smokers, and the risk drops significantly once you quit.
- Alcohol Use: Drinking beyond recommended limits (one drink per day for women, two for men) raises blood pressure and triglycerides, further increasing risk.
- Chronic Stress: Persistent stress can contribute to depression, disrupt healthy routines (diet, exercise), and has direct effects on blood pressure and inflammation.
Table: Controllable vs. Uncontrollable Heart Disease Risk Factors
| Controllable Factors | Uncontrollable Factors |
|---|---|
|
|
Who Is Most at Risk for Heart Disease?
Anyone can develop heart disease, yet some groups face higher risk than others. Those most at risk:
- Adults with multiple medical conditions (high blood pressure & diabetes combined heighten risk substantially)
- Individuals with a strong family history, especially if relatives developed heart disease young
- Men, or women post-menopause
- People with unhealthy lifestyles: smokers, sedentary individuals, or those with poor diets
- Members of certain ethnic backgrounds (see earlier list)
Understanding your specific risk factors can help motivate tailored prevention strategies, such as regular screenings, medication for blood pressure or cholesterol, and targeted lifestyle changes.
Can Heart Disease Be Prevented?
While some heart disease risk factors aren’t within your control, most people can dramatically lower their risk by:
- Quitting smoking and avoiding secondhand smoke
- Adopting a heart-healthy diet low in saturated fat and sodium, high in fruits, vegetables, and fiber
- Exercising regularly, aiming for at least 150 minutes of moderate activity per week
- Maintaining a healthy weight through diet and activity
- Managing chronic conditions with the help of your healthcare team
- Limiting alcohol intake according to medical guidelines
- Addressing depression and stress through counseling, social support, or medical therapy if needed
Frequently Asked Questions (FAQs)
Q: What are early signs of heart disease?
A: Early signs can be subtle, but may include chest pain, shortness of breath, fatigue, or irregular heartbeat. Often, risk factors like high blood pressure or cholesterol are the first clues and can be detected through regular screening before symptoms develop.
Q: Are there differences in heart disease risk between men and women?
A: Yes, men tend to develop heart disease earlier, but women’s risk rises sharply after menopause, eventually matching or surpassing men’s risk.
Q: How much does quitting smoking reduce my risk?
A: Within one year of quitting, your risk of heart attack drops significantly. After 5–15 years, your risk is nearly the same as someone who never smoked.
Q: Does lowering my cholesterol always lower my heart disease risk?
A: Lowering LDL (bad) cholesterol reduces plaque build-up, while raising HDL (good) cholesterol adds protection. Both medication and lifestyle measures can help.
Q: Is heart disease reversible?
A: While advanced atherosclerosis cannot be entirely reversed, lifestyle changes, medications, and interventions can slow progression and sometimes reduce existing plaque, greatly lowering the risk of heart attack.
The Takeaway
Heart disease is shaped by a complex web of genetic, health, and lifestyle factors. While you can’t change your age, sex, or family history, you have powerful tools at your disposal to lower your risk—by managing chronic conditions, adopting healthy habits, and staying informed. Talk with your healthcare provider about your risk factors and what steps you can take today to protect your heart for years to come.
References
- https://www.healthline.com/health/heart-disease
- https://www.cdc.gov/heart-disease/risk-factors/index.html
- https://www.healthline.com/health/heart-disease/causes-risks
- https://www.medicalnewstoday.com/articles/257484
- https://www.medicalnewstoday.com/articles/237191
- https://lifeprogram.org.au/health-hub/earlysignsofheartdiseaseinmen/
- https://www.chp.gov.hk/en/static/80035.html
- https://www.healthline.com/health/video/how-to-lower-cholesterol
- https://www.uc.edu/news/articles/legacy/healthnews/2007/02/uc-health-line–what-women-need-to-know-about-heart-attacks.html
- https://www.cedars-sinai.org/newsroom/healthline-therapy-vs-antidepressants–which-is-best-for-people-with-heart-disease/
Read full bio of Sneha Tete












