Understanding Electrophysiology Procedures: What to Expect and Why They’re Essential
A comprehensive guide to electrophysiology procedures, from purpose and preparation to benefits, risks, and recovery.
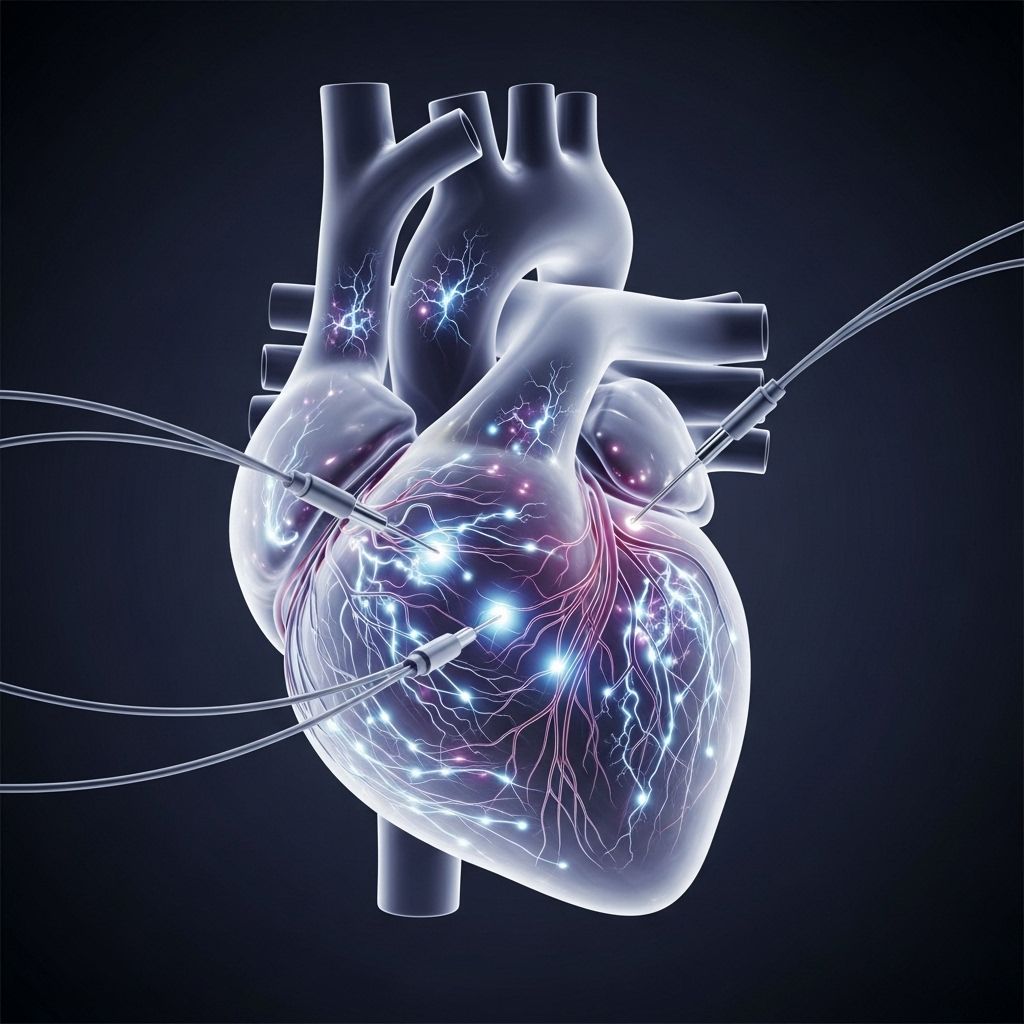
Electrophysiology (EP) procedures are powerful tools that cardiologists rely on to diagnose and treat irregular heart rhythms, also known as arrhythmias. These minimally invasive procedures help specialists evaluate the heart’s internal electrical activity, allowing for both diagnosis and therapeutic interventions. In this guide, you’ll learn what an electrophysiology procedure entails, why your doctor might recommend one, how to prepare, the step-by-step process, potential risks and benefits, and what your recovery may look like.
What Is an Electrophysiology Procedure?
An electrophysiology procedure is a series of tests and interventions that allow doctors to record, analyze, and often correct abnormal heart electrical activity. These procedures are performed by specially trained cardiologists called electrophysiologists. The primary goals are to determine the origin of an abnormal heart rhythm (arrhythmia), offer a precise diagnosis, and sometimes provide immediate therapy such as catheter ablation or device implantation.
- EP procedures use catheters tipped with electrodes to map the heart’s electrical system.
- The procedure can involve: simple electrical recordings, stimulating the heart to reproduce arrhythmias, and delivering treatments through the same catheters.
Normal heart function relies on a synchronized electrical signal traveling through the heart muscle, allowing it to contract and pump blood efficiently. When these electrical signals are disrupted, it can lead to arrhythmias, which in turn may cause palpitations, dizziness, fainting, chest pain, or even sudden cardiac arrest.
Why Is an Electrophysiology Procedure Performed?
Your doctor may recommend an EP study or related intervention if you have symptoms suggestive of a heart rhythm disorder or if previous tests indicate an electrical disturbance. Common reasons for referring someone for an electrophysiology procedure include:
- Unexplained fainting episodes (syncope)
- Recurrent or persistent palpitations
- Unusual heart rhythms detected on ECG or during monitoring
- Assessment prior to treatment for certain arrhythmias
- Evaluation for potential device implantation (pacemaker or ICD)
- Determining the risk of future arrhythmia in certain heart disease conditions
These procedures can directly guide therapies like ablation, where the problematic heart tissue is destroyed, or guide medication management and device therapies.
Tests and Measurements Performed During an EP Procedure
Electrophysiology procedures are comprehensive, and the exact tests depend on your particular symptoms and heart condition. Common components of an EP procedure include:
- Standard cardiac mapping: Electrodes on your skin and catheters inside your heart record electrical signals to locate where an arrhythmia originates.
- Stimulation or pacing tests: Small electrical impulses may be delivered through catheters to change your heart rate and identify how arrhythmias develop or are sustained.
- Intracardiac electrograms: Highly sensitive measurements inside your heart reveal the timing and route of electrical conduction.
- Medication testing: Sometimes, medications are administered through the catheter to observe their effects on your heart’s electrical system or to help provoke certain arrhythmias under controlled settings.
The results help the electrophysiologist build a detailed map of your heart’s electrical activity, which is essential for diagnosis and for planning treatment during the same session, if appropriate.
How Invasive Is an Electrophysiology Procedure?
An EP procedure is considered minimally invasive but does involve some intervention. The noninvasive component is the surface ECG measurement, but catheter insertion—usually through blood vessels in the groin, wrist, or neck—is a minor surgical procedure. Local anesthetic is typically used at the insertion site to make you comfortable.
- Most people experience minimal discomfort, typically only mild soreness where the catheter(s) were inserted, especially as anesthesia wears off later.
- Occasionally, some people may notice heart rate changes or palpitations during the test as doctors stimulate the heart—these should not hurt, but they can feel unusual.
Who Performs Electrophysiology Procedures?
These procedures are performed by electrophysiologists, who are cardiologists with advanced training in diagnosing and treating arrhythmias. They work within a multidisciplinary team that may include nurses, anesthetists, and specialized technicians.
An electrophysiology laboratory or EP suite is a highly specialized facility within a hospital, equipped with advanced imaging tools, monitoring equipment, and technology for both diagnostic and therapeutic procedures. Your care team will focus on ensuring your safety and comfort throughout the procedure.
Preparing for Your Electrophysiology Procedure
Your healthcare team will provide detailed instructions tailored to your unique health needs, but general preparation often includes:
- Pre-procedure assessments: Blood work, ECGs, and possibly imaging tests will be performed ahead of time.
- Medication adjustments: Inform your doctor about all medications and supplements you take—certain blood thinners or anti-arrhythmic drugs may need to be paused or adjusted.
- Fasting: You may be asked to avoid eating or drinking for at least six hours before the procedure.
- Arrange transportation: Since you’ll receive sedative or anesthesia medications, someone should drive you home after the procedure.
Wear comfortable clothing and leave jewelry or valuables at home. Bring a list of your medications and any necessary paperwork for hospital admission.
What Happens During the Electrophysiology Procedure?
The timeline and details may vary, but here’s a typical sequence for an EP procedure:
- Admission and consent: You’ll be admitted to the hospital’s electrophysiology lab. Your team will review your records, explain the procedure, and answer any last-minute questions. You will be asked to sign a consent form.
- Monitoring and IV placement: Electrodes are placed on your chest to monitor your heart, and a blood pressure cuff may be attached. An intravenous line is started to administer fluids, medications, and sedatives as needed.
- Preparing the insertion site: The area (often the groin, less often the neck or arm) is shaved and sterilized. A local anesthetic is injected to numb the site.
- Catheter insertion: One or more thin, flexible catheters (about the size of spaghetti) are threaded through a small blood vessel, guided by imaging screens into the heart.
- Recording and pacing: The catheters detect and record your heart’s electrical activity, and controlled electrical impulses may pace your heart at different rates.
- Ablation or further intervention: If the source of your arrhythmia is found and ablation is planned, radiofrequency energy or extreme cold may be applied to destroy a tiny area of heart tissue causing the problem.
- Completion: The catheters are removed, and pressure is applied to the insertion site. The area is bandaged and monitored closely for bleeding or other issues.
How Long Does an Electrophysiology Procedure Take?
The length of an EP procedure can vary, depending on its complexity and the number of tests or treatments required:
- Simple diagnostic procedures often last 1–2 hours.
- If catheter ablation or a device implant is needed, the procedure may last 3–6 hours or longer.
You will remain under close supervision throughout, and your healthcare team will keep you informed about what to expect during each stage.
Risks and Potential Complications
EP procedures are generally safe and well-tolerated, but like any medical procedure, they carry some risks. Your doctor will discuss these with you beforehand, and all steps will be taken to minimize them. Potential risks include:
- Bleeding or bruising at the catheter insertion site
- Minor pain or discomfort at the site
- Infection
- Blood clot formation
- Damage to blood vessels or heart structures
- Unexpected or worsened arrhythmia during the study
- Heart attack or stroke (rare)
Special precautions and medications are administered during and following the procedure to help mitigate these risks, including careful monitoring of your heart’s rhythm and blood pressure, as well as support in the event of bleeding or other complications.
Recovery and Aftercare
After your EP procedure, you’ll be monitored in a recovery area—sometimes for several hours—until you’re fully awake and your heart rhythm and blood pressure are stable:
- You must remain lying down and avoid moving the leg or arm used for catheter access until your doctor decides it’s safe.
- The insertion site will be checked for bleeding or swelling, and you may have pressure dressings applied.
- Most people can eat and drink after a few hours, once fully awake.
- Once cleared, you’ll be able to get up and walk around. Some mild soreness or bruising is normal.
Returning home:
- Most patients return home the same day; some may stay overnight depending on the procedure and any underlying conditions.
- You should avoid strenuous activity, heavy lifting, and driving for at least 24 hours or as directed by your healthcare team.
- Monitor the insertion site for signs of infection (redness, swelling, oozing) and call your doctor if you develop a fever, significant discomfort, or new symptoms.
Benefits of Electrophysiology Procedures
EP procedures are crucial for:
- Pinpointing the source of abnormal heart rhythms (arrhythmias)
- Guiding lifesaving therapies, such as ablation or device placement
- Personalizing medication management
- Reducing symptoms and risk of complications associated with untreated arrhythmias
- Improving quality of life and long-term outcomes for many heart rhythm disorders
Commonly Asked Questions (FAQs)
What is the main purpose of an electrophysiology procedure?
EP procedures are performed to diagnose and treat abnormal heart rhythms, identify their source, and determine the best management strategy—which may include medication, ablation, or device therapy.
Will I be awake during the procedure?
Most patients remain awake but relaxed, thanks to sedative medications. You may feel slight pressure or mild discomfort, but pain is unusual. In some cases, general anesthesia may be used for complex procedures.
How soon can I resume normal activities after an electrophysiology procedure?
Most people can return to regular activities the day after their procedure but should avoid strenuous exercise, heavy lifting, and driving for at least 24 hours—follow your specific instructions from the care team.
Are there alternatives to electrophysiology studies?
Alternatives may include external monitors (Holter or event monitors), noninvasive imaging, or blood tests. However, EP procedures provide the most detailed and dynamic assessment of the heart’s electrical system, especially when treatment can be performed at the same time.
What are the signs I should seek medical attention after the procedure?
Contact your doctor if you experience significant bleeding, swelling, or pain at the catheter site; fever; chest pain; shortness of breath; or a rapid or irregular heartbeat.
Summary Table: Key Facts about Electrophysiology Procedures
| Aspect | Details |
|---|---|
| Purpose | Diagnose, monitor, and treat heart rhythm disorders |
| Performed By | Electrophysiologist (specialist cardiologist) |
| Invasiveness | Minimally invasive (catheter-based) |
| Common Risks | Bleeding, bruising, infection, arrhythmia, vascular injury |
| Approximate Duration | 1–6 hours, depending on complexity |
| Average Recovery Time | 1–2 days for most patients |
Conclusion
Electrophysiology procedures are vital diagnostic and therapeutic tools in contemporary cardiology. They empower doctors to precisely identify and treat arrhythmias, reduce symptoms, and improve quality of life for many individuals facing heart rhythm problems. If your healthcare provider recommends an EP study, understanding the process, benefits, risks, and recovery can help you feel confident and well-prepared every step of the way.
References
- https://www.medicalnewstoday.com/articles/what-is-an-electrophysiology-procedure
- https://www.ucsfhealth.org/education/electrophysiology-procedure
- https://www.healthline.com/health/heart/what-is-an-electrophysiology-procedure
- https://www.healthline.com/health/electrophysiologist
- https://www.ncbi.nlm.nih.gov/books/NBK567719/
- https://www.heart.org/en/health-topics/arrhythmia/symptoms-diagnosis–monitoring-of-arrhythmia/electrophysiology-studies
- https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.071542
Read full bio of Sneha Tete












