Understanding Diabetic Retinopathy: Symptoms, Stages, and Prevention
Diabetic retinopathy is a leading cause of vision loss—learn about its symptoms, stages, treatments, and prevention to protect your eyesight.
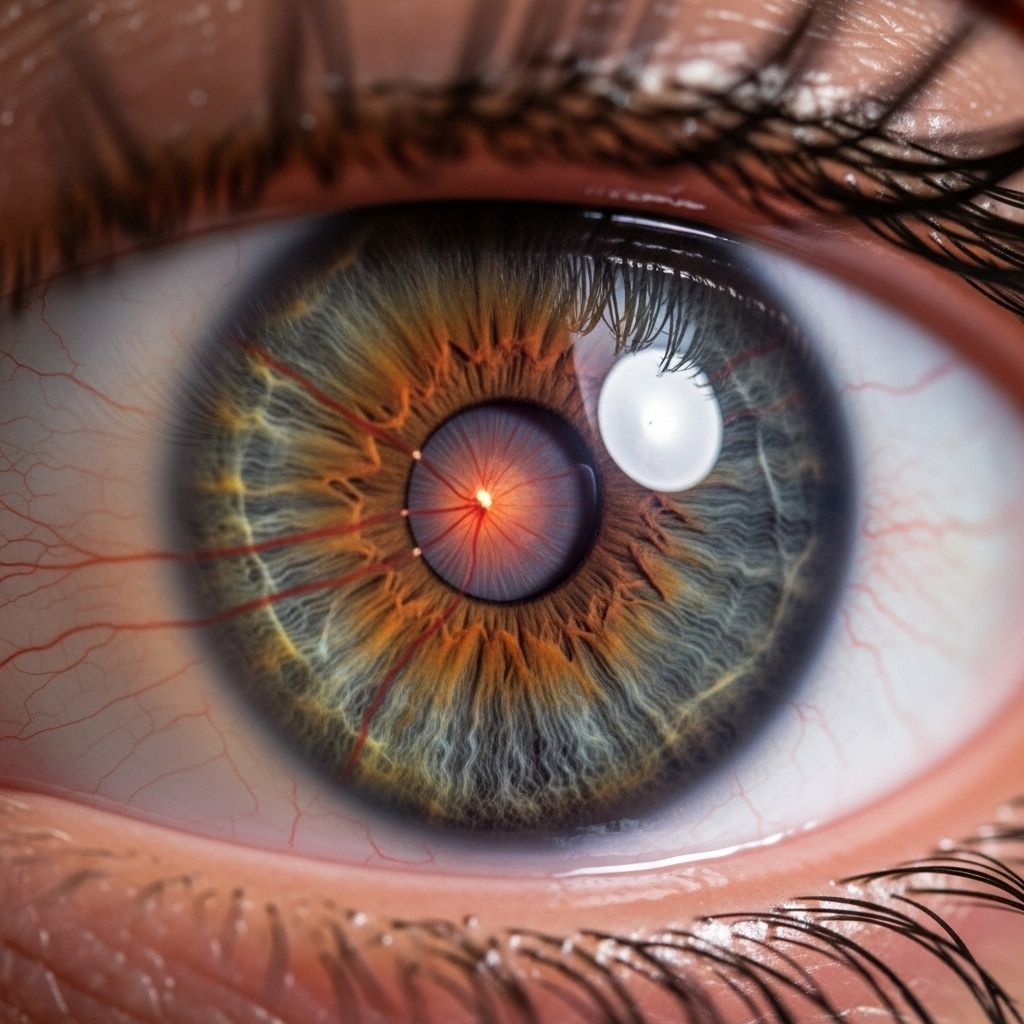
Diabetic retinopathy is a serious and common complication of diabetes that impacts the small blood vessels in the retina—the light-sensitive layer at the back of the eye. As high blood sugar damages these vessels, diabetic retinopathy can progress to vision impairment and even blindness if left undiagnosed or untreated. However, with early detection, effective management, and timely intervention, most vision loss caused by diabetic retinopathy is preventable. This article provides a detailed overview of diabetic retinopathy, covering its risk factors, symptoms, stages, diagnosis, treatments, and prevention strategies.
What Is Diabetic Retinopathy?
Diabetic retinopathy is a microvascular complication of diabetes characterized by damage to the blood vessels of the retina. The retina plays a crucial role in vision by converting light into neural signals which the brain interprets as visual images. Any damage to the retina can compromise your ability to see clearly and accurately.
The condition develops gradually and may not cause noticeable symptoms in its early stages. Left unchecked, it can lead to vision loss that may be irreversible. Regular eye examinations and effective diabetes management are essential for early detection and prevention.
Causes and Risk Factors
Diabetic retinopathy is caused primarily by prolonged high blood glucose levels, which damage the delicate blood vessels in the retinal tissue. Over time, persistent high blood sugar can weaken, swell, and disrupt these vessels, leading to leakage, bleeding, and impaired blood flow. In advanced cases, new, abnormal blood vessels may begin to grow in the retina—a response that often exacerbates the problem.
- Duration of diabetes: The longer you have diabetes, the higher your risk.
- Poor blood sugar control: Chronic hyperglycemia accelerates retinal damage.
- High blood pressure: Elevated blood pressure can worsen blood vessel damage in the eyes.
- High cholesterol: Unhealthy cholesterol levels add to the risk for vascular complications.
- Pregnancy: Gestational changes may increase risk in women with diabetes.
- Tobacco use: Smoking is linked to greater risk of diabetic complications, including retinopathy.
Genetics and inherited metabolic abnormalities can also play a role, but these are far less common than the direct impact of chronic high blood sugar.
Stages of Diabetic Retinopathy
Diabetic retinopathy is a progressive disease, developing in well-defined stages. Recognizing these stages is crucial for both patients and healthcare providers.
| Stage | Description | Key Features |
|---|---|---|
| Mild Nonproliferative Retinopathy | The earliest stage. Microaneurysms (tiny bulges) form in the retinal blood vessels. | Occasional leaking of fluid; few, if any, symptoms. |
| Moderate Nonproliferative Retinopathy | Some blood vessels nourishing the retina are blocked. | Early vision changes may appear. |
| Severe Nonproliferative Retinopathy | More vessels are blocked, depriving retinal areas of blood supply. Retina signals the body to grow new blood vessels. | Significantly increased risk for progression to advanced disease. |
| Proliferative Diabetic Retinopathy | The most advanced stage. New, fragile blood vessels grow along the retina and into the vitreous gel. | Prone to bleeding, scarring, retinal detachment, and vision loss. |
Symptoms
Early diabetic retinopathy typically causes no symptoms. As it advances, one or more of the following may develop:
- Blurry or fluctuating vision
- Dark or empty areas in your field of vision
- Impaired color vision
- Difficulty focusing
- Seeing spots or floaters
- Vision loss, which can become sudden and severe in advanced cases with bleeding
Complications
Diabetic retinopathy can give rise to significant complications that threaten eyesight:
- Vitreous hemorrhage: New, abnormal retinal vessels may leak blood into the eye’s center (vitreous), causing spots, streaks, or a complete vision block.
- Retinal detachment: Scar tissue from new vessel growth can pull the retina away from the back of the eye, leading to light flashes, floaters, and severe vision loss.
- Glaucoma: Abnormal blood vessels can block the drainage of fluid from the eye, raising pressure and damaging the optic nerve.
- Permanent vision loss: Without prompt treatment, advanced diabetic retinopathy can result in irreversible blindness.
Diagnosis
Regular eye exams are vital for those with diabetes. Doctors typically detect diabetic retinopathy through a dilated eye examination:
- The doctor uses special eye drops to widen the pupils.
- The inside of the eye and retina are examined for swelling, abnormal blood vessels, bleeding, or fluid leakage.
- Advanced imaging, such as a fluorescein angiogram, may be employed to better visualize blood vessel changes and leakage.
Eye exams are recommended annually for people with diabetes, but your doctor may advise more frequent checks depending on existing eye health and your diabetes management.
Treatments and Management
The cornerstone of diabetic retinopathy management is optimal blood sugar control. Consistently maintaining blood glucose, blood pressure, and cholesterol at healthy levels is the most effective way to slow progression and reduce risk.
For early-stage retinopathy, improvements in diabetes control may be all that’s necessary, along with monitoring.
Advanced or symptomatic disease may require additional interventions:
- Laser surgery (photocoagulation): Creates small burns in the retina to seal or destroy abnormal vessels and stop leakage.
- Intravitreal injections: Medications (such as steroids or anti-VEGF agents) injected directly into the eye to reduce swelling, suppress growth of abnormal vessels, or control inflammation.
- Vitrectomy: A surgical procedure to remove blood, scar tissue, or fluid that threatens or impedes vision. May also include repairing retinal detachments.
Treatment choice depends on the stage and severity of the condition, as well as overall eye health and medical history. Regular follow-ups are crucial to monitor progress and adapt treatment as needed.
Prevention
Although some people may develop diabetic retinopathy despite good blood sugar control, prevention strategies greatly reduce the risk and severity of eye complications:
- Control blood sugar: Aim for targets set by your diabetes care team (often an A1C of 7% or less).
- Manage blood pressure and cholesterol: Take prescribed medications and make dietary changes as needed.
- Annual eye exams: Regular checkups catch retinopathy early, when treatment is most effective.
- Quit smoking: Smoking worsens vascular damage.
- Adopt a healthy lifestyle: Regular physical activity, balanced nutrition, and consistent use of diabetes medication all play a role in prevention.
Frequently Asked Questions (FAQs)
Q: Can diabetic retinopathy be reversed?
No, the structural changes in the retina caused by diabetic retinopathy cannot be completely reversed. However, early detection and prompt treatment can prevent further progression and reduce or stabilize vision loss.
Q: How often should people with diabetes have an eye exam?
Experts recommend a comprehensive, dilated eye exam at least once a year for anyone with diabetes, or more frequently if advised by an ophthalmologist based on your risk level or findings from prior exams.
Q: Does controlling blood sugar always prevent retinopathy?
While excellent glucose control significantly reduces risk, it does not guarantee prevention. Some people develop retinopathy even with good diabetes management, underscoring the importance of regular eye exams.
Q: Are there any early warning symptoms?
Early diabetic retinopathy often has no noticeable symptoms. Vision changes may indicate advanced disease. Regular checkups are essential for early detection as symptoms may not develop until significant damage has occurred.
Q: Is diabetic retinopathy only a concern for type 1 diabetes?
No. Both type 1 and type 2 diabetes pose a risk for diabetic retinopathy. The risk increases with duration and poor control of the disease in all types.
Key Takeaways
- Diabetic retinopathy is a leading cause of preventable blindness in adults with diabetes.
- Early stages may produce no symptoms, so annual eye exams are essential.
- Control of blood sugar, blood pressure, and cholesterol are the best means of prevention and slowing progression.
- Modern treatments, including laser therapy and injections, can halt or repair some damage if caught early.
- A multidisciplinary approach involving primary care, endocrinologists, and eye specialists is most effective for protecting vision.
References and Resources
- National Eye Institute
- American Diabetes Association
- Beyond Type 1 Diabetes Community
- Mayo Clinic Health Information
References
- https://beyondtype1.org/diabetic-retinopathy/
- https://www.healthline.com/health/diabetes/diabetic-retinopathy-stages
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
- https://www.medicalnewstoday.com/articles/ozempic-semaglutide-may-help-protect-against-diabetes-related-blindness-retinopathy
- https://www.medicalnewstoday.com/articles/323729
- https://www.ccjm.org/content/91/8/503
Read full bio of medha deb












