Understanding Craniotomy: Procedure, Risks, and Recovery
Explore what a craniotomy involves, why it is performed, potential risks, and what to expect before, during, and after brain surgery.
Craniotomy
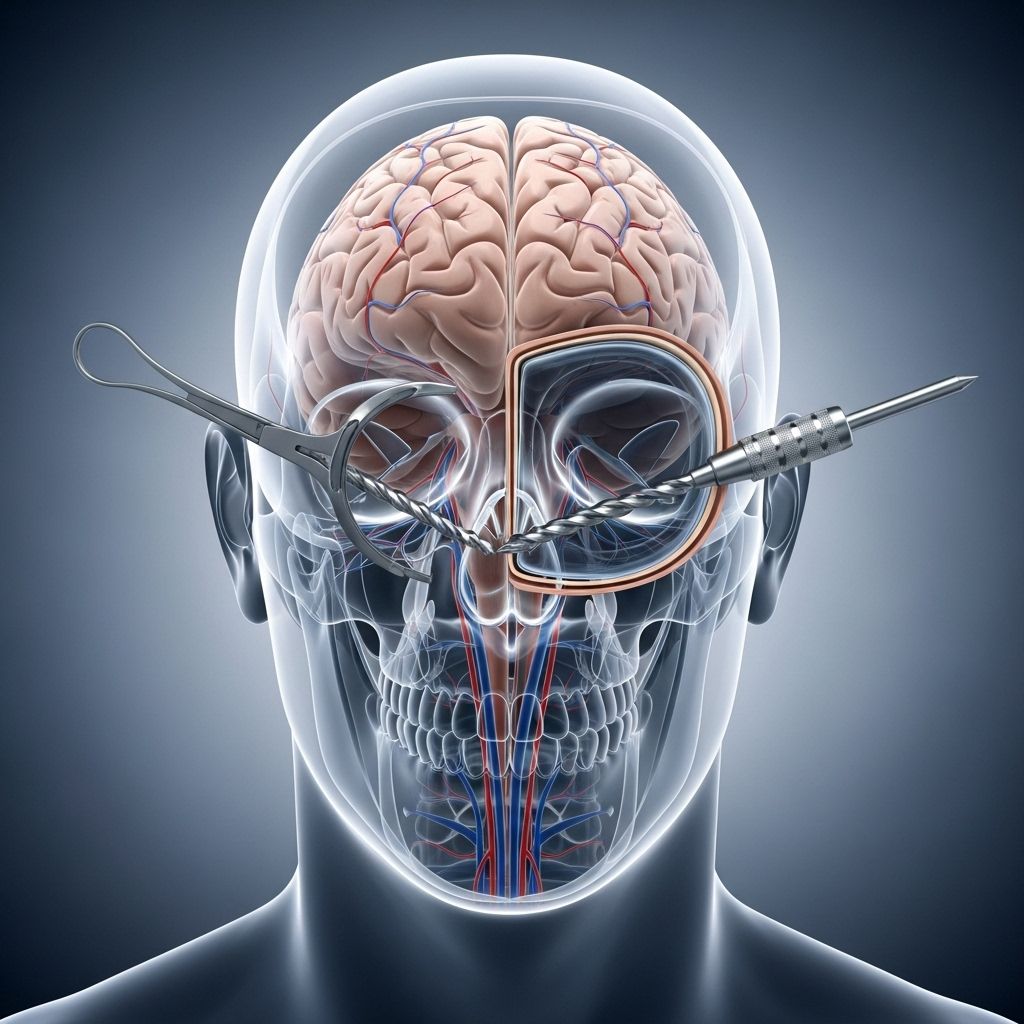
A craniotomy is a surgical procedure in which a section of the skull—called a bone flap—is temporarily removed to access the brain. This critical neurosurgical intervention is performed for various medical reasons, such as removing brain tumors, treating brain injury, or repairing blood vessel abnormalities. The procedure has evolved significantly with advances in imaging, surgical techniques, and precision tools, helping to improve outcomes and reduce risks associated with opening the skull.
What is a Craniotomy?
A craniotomy is a procedure in which a portion of the skull is surgically opened to allow a neurosurgeon direct access to the brain. Once the underlying neurological issue is addressed, the bone flap is secured back in place with specialized plates and screws. Depending on the surgery’s objective, a craniotomy may range from a small keyhole opening to a much larger bone removal. The size and location depend on the area of the brain requiring treatment and the complexity of the procedure.
Reasons for a Craniotomy
Craniotomies are performed for a variety of neurologic and neurosurgical conditions. The most common reasons for a craniotomy include:
- Brain Tumor Removal: To access and remove benign or malignant tumors in the brain tissue.
- Aneurysm Clipping: To repair or clip a brain aneurysm and prevent bleeding.
- Hematoma Evacuation: To remove blood clots from trauma or spontaneous bleeding (e.g., subdural or epidural hematomas).
- Arteriovenous Malformation (AVM) Repair: To correct abnormal tangles of blood vessels in the brain.
- Traumatic Brain Injury Intervention: To relieve pressure, repair fractures, or remove foreign objects after head trauma.
- Epilepsy Surgery: To remove a seizure focus in severe, medication-resistant epilepsy.
- Biopsy: To obtain tissue samples from the brain for diagnostic purposes.
- Infection or Abscess Drainage: To treat severe infections within or around the brain.
Types of Craniotomy
The specific approach and technique for a craniotomy depend on the clinical indication and the location of the affected brain tissue. Major types include:
- Conventional (Standard) Craniotomy: The most common technique, involving a larger bone flap to allow wide exposure.
- Minimally Invasive (Keyhole) Craniotomy: Involves a much smaller opening, designed to reduce trauma to the scalp and skull—for example, minicraniotomy through the eyelid for access to certain brain regions.
- Awake Craniotomy: Performed while the patient is awake but sedated in order to map and preserve critical nerve functions during surgery near important areas like those controlling speech or movement.
- Endoscopic Craniotomy: Uses an endoscope (a camera-tipped instrument) to facilitate less invasive access to deep brain structures.
Preparation for a Craniotomy
Preparation for a craniotomy requires careful planning by an experienced neurosurgical team. Steps generally include:
- Diagnostic Imaging: MRI or CT scans are performed to assess the lesion, guide preoperative planning, and help the surgeon choose the best approach.
- Medical Evaluation: Routine blood tests, electrocardiogram (ECG), and anesthesia evaluation are conducted to assess the patient’s general health.
- Medication Instructions: The team provides instructions regarding medications to stop or continue before surgery, including blood thinners.
- Fiducial Marker Placement: Small sticky markers, called fiducials, may be applied to the scalp to guide surgical navigation much like a GPS system.
- Antiseptic Preparation: The evening before surgery, patients are often asked to use a special antibiotic shampoo to reduce the risk of infection.
- Fasting and Rest: Patients are instructed to refrain from eating or drinking after midnight and to rest well before the procedure.
How is a Craniotomy Performed?
The details of the craniotomy procedure vary by the specific purpose, but generally include the following steps:
- Anesthesia: The patient is usually given general anesthesia to ensure they are unconscious and pain-free. In special cases (e.g., awake craniotomy), local anesthesia is used and the patient stays responsive for neurologic testing.
- Positioning: The patient’s head is secured in a specialized clamp to keep it completely still throughout the operation.
- Scalp Incision: The surgeon makes an incision in the scalp, which may vary in size and location based on the brain area being accessed.
- Bone Flap Removal: A small, high-speed drill is used to create burr holes, followed by a surgical saw to form an outline and lift a portion of the skull (bone flap).
- Dura Mater Opening: The tough membrane (dura) covering the brain is carefully cut and folded back to reveal the underlying tissue.
- Treatment of Brain Condition: The neurosurgeon carries out the necessary procedure—removing a tumor, repairing blood vessels, sampling tissue, or evacuating blood.
- Dura and Skull Closure: The dura is sutured closed, and the bone flap is replaced and secured with plates and screws. Sometimes, the bone flap is not replaced immediately (as in a decompressive craniectomy).
- Scalp Closure: The incision is closed with staples or sutures, often followed by a protective bandage.
Modern craniotomy often incorporates advanced computer-guided navigation and intraoperative imaging to maximize surgical accuracy and minimize the risk of damage to healthy brain tissue.
Innovations in Craniotomy Approaches
Recent years have seen important technical advances, leading to less invasive approaches. For example:
- Transpalpebral Orbitofrontal Craniotomy: Small bone removal via the natural crease of the eyelid provides access to the middle and front parts of the brain. This approach offers less trauma, reduced operating time, and minimal scarring compared to traditional skull-based surgery.
- Endoscopic and Image-Guided Techniques: Using computer-generated brain maps from CT and MRI scans, surgeons can plan more precise, targeted pathways and minimize disturbance to healthy brain areas.
| Aspect | Traditional Craniotomy | Minimally Invasive/Keyhole |
|---|---|---|
| Incision Size | Large (multiple inches) | Small (often under 1 inch) |
| Operating Time | 4-8 hours | ~2 hours |
| Scarring | Visible on scalp | Hidden/in natural creases, often unnoticeable |
| Hospital Stay | Several days | Usually overnight |
| Risks | Higher infection risk, more trauma | Lower infection risk, less trauma |
Risks and Complications of Craniotomy
Like any major surgery, craniotomy carries specific risks that should be carefully discussed with your neurosurgical team. Risks can vary with underlying health conditions, surgical complexity, and brain area affected. Common risks include:
- Infection: Despite sterile techniques, infection of the wound, skull bone, or brain tissue may occur.
- Bleeding: Hemorrhage during or after surgery can create blood clots, sometimes requiring further surgery.
- Swelling: Edema (swelling) in the brain can increase pressure and may require monitoring and treatment.
- Seizures: The risk of postoperative seizures is higher after brain surgery, and anticonvulsant medications are sometimes used.
- Neurological Deficits: Depending on the brain region, surgery may result in temporary or permanent weakness, changes in speech, vision, memory, or sensation.
- CSF (Cerebrospinal Fluid) Leak: Leaks from the incision can occasionally develop, sometimes needing repair.
- Stroke: Rarely, a stroke or loss of blood flow to the brain may occur.
- Blood Clots: Patients are at risk for clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism).
- Reactions to Anesthesia: Allergies or complications related to anesthesia can occur.
Recovery after a Craniotomy
Recovery from a craniotomy varies greatly depending on the nature of the underlying condition, the brain region involved, the patient’s general health, and the specific surgical approach. Here’s what to expect after brain surgery:
- Hospital Stay: Typically ranges from one night (minimally invasive) up to a week or more (complex cases). Patients are closely monitored in a neurosurgical intensive care unit (ICU) initially.
- Pain Management: Headache and discomfort at the incision site are common and controlled with medication.
- Neurological Checks: Frequent monitoring to assess mental status, speech, muscle strength, sensation, and vision.
- Swelling and Bruising: These are common, especially around the incision, and usually resolve over days to weeks.
- Anticonvulsant Medication: Often prescribed temporarily to reduce the risk of seizures.
- Physical and Occupational Therapy: Rehab may be needed to regain strength, coordination, speech, or cognitive skills if deficits are identified.
- Follow-Up Imaging: Follow-up CT or MRI scans are done to monitor for any complications or recurrence of disease.
- Return to Activity: Light activity is encouraged as tolerated, but heavy lifting and strenuous exercise should be avoided for several weeks.
Prognosis and Long-Term Outlook
The outcome after a craniotomy depends on the condition treated, the patient’s age and overall health, and the location and size of the brain region involved. In many cases, craniotomy significantly improves symptoms or removes life-threatening problems. However, some neurological deficits may persist, and ongoing rehabilitation or therapy could be required for optimal recovery. Most patients gradually return to work and other activities, sometimes with certain restrictions.
Questions to Ask Your Doctor
Before undergoing a craniotomy, it is important to have a thorough discussion with your neurosurgeon and care team. Key questions to consider include:
- What is the specific diagnosis requiring a craniotomy?
- What are the goals and expected outcomes of surgery?
- Are there nonsurgical options or minimally invasive approaches?
- What are the potential risks and benefits unique to my situation?
- What is the likely recovery time and prognosis?
- What rehabilitation or support services will be available after surgery?
- How experienced is my surgical team with this type of procedure?
Frequently Asked Questions (FAQs)
Q: How long does craniotomy surgery normally take?
A: Surgical time ranges widely based on the problem, but standard craniotomies often last 4–8 hours. Minimally invasive approaches can sometimes be completed in about 2 hours.
Q: Will part of my hair be shaved for surgery?
A: Often, only a small area is shaved. Newer techniques increasingly spare hair by working through small openings or natural creases (such as the eyelid).
Q: Will I have a visible scar?
A: Traditional craniotomies leave a scalp scar, but minimally invasive procedures may leave minimal or even unnoticeable scars, particularly when incisions are made in natural skin creases.
Q: When can I return to regular activities?
A: Patients typically resume light activities in several weeks, but strenuous activities are usually postponed for up to two months. Individual timelines vary based on the surgery’s complexity and recovery progress.
Q: What complications should I look out for after surgery?
A: Notify your care team about fever, worsening headache, unusual drowsiness, seizure, leakage from the incision, or new neurological symptoms such as weakness or speech changes.
Summary
Craniotomy is a vital neurosurgical procedure, enabling treatment of many brain conditions that might otherwise be untreatable. Continued advancements in imaging, minimally invasive techniques, and surgical precision have improved patient outcomes and reduced both recovery times and risks. Discuss your concerns thoroughly with your health care team to understand your unique risks, benefits, and the best way forward for your needs.
References
Read full bio of Sneha Tete












