Understanding Constipation: Causes, Symptoms, Treatment, and Prevention
Learn about constipation, its symptoms, causes, treatments, and prevention for better digestive health and daily wellness.
Constipation
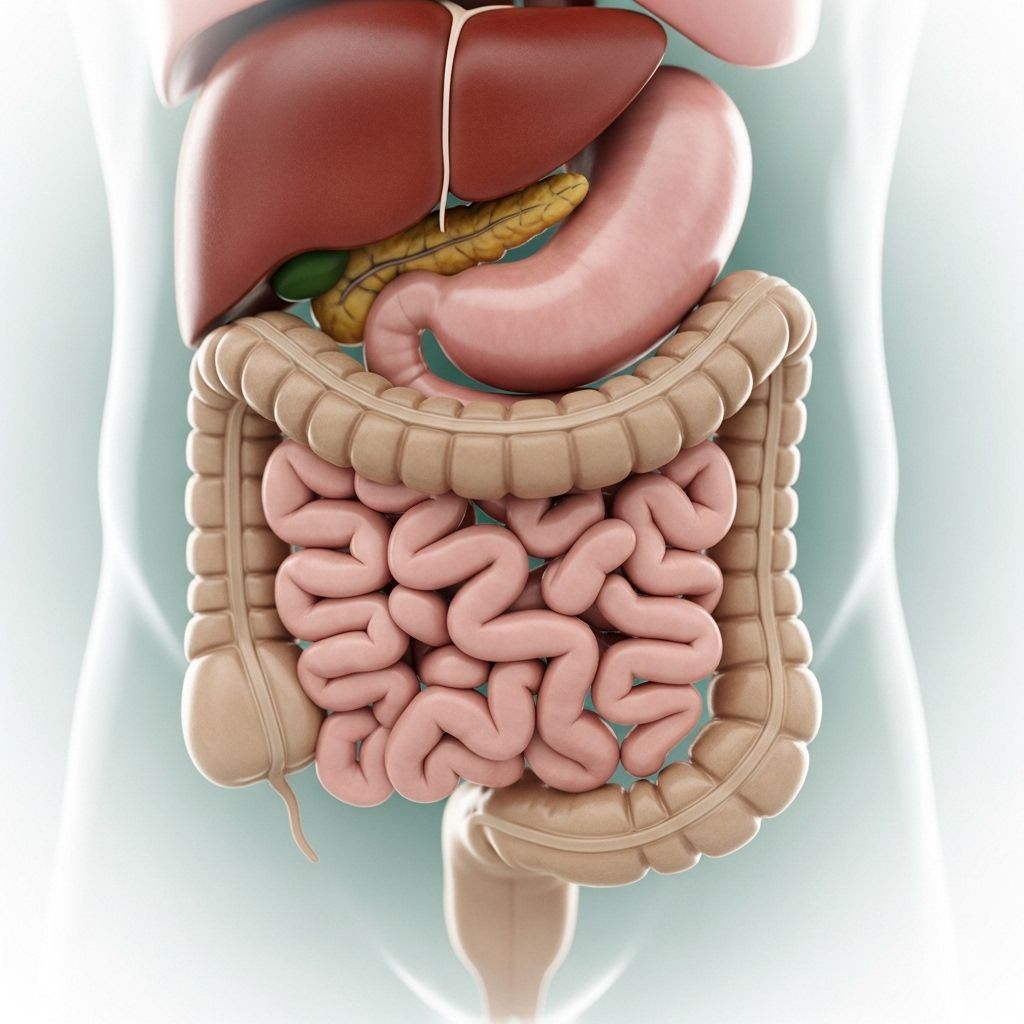
Constipation is a common digestive condition characterized by infrequent, difficult, or painful bowel movements. Affecting millions of people, it impacts quality of life and can be a symptom of underlying health problems. Understanding its causes, symptoms, treatment options, and preventive strategies is vital for maintaining overall digestive health.
What is Constipation?
Constipation refers to fewer than three bowel movements per week, passing dry, hard, or lumpy stools, and feeling that bowel movements are incomplete or require excessive straining. While digestive habits vary, chronic constipation is diagnosed when these symptoms persist for several weeks or longer. Both short-term and chronic constipation can occur, with chronic cases demanding further medical evaluation.
Common Signs and Symptoms
- Fewer than three bowel movements per week
- Hard, dry, or lumpy stools
- Straining during bowel movements
- Sensation of incomplete emptying
- Abdominal bloating or discomfort
- Rectal pain during bowel movements
- Needing manual assistance (such as pressing on the abdomen)
Constipation symptoms may be mild, moderate, or severe and can significantly impact daily activities and overall well-being.
Causes of Constipation
Constipation can result from a variety of factors. Most cases are functional, meaning no underlying anatomic or biochemical abnormality is found. However, certain medical conditions, medications, or lifestyle choices can contribute to the development or persistence of constipation.
Common Causes
- Inadequate dietary fiber: Not consuming enough fruits, vegetables, and whole grains slows intestinal transit.
- Insufficient fluid intake: Dehydration leads to harder stools and makes them more difficult to pass.
- Physical inactivity: Sedentary lifestyle reduces gut motility, increasing the risk of constipation.
- Ignoring the urge: Regularly delaying bowel movements may desensitize the urge to go.
- Medications: Certain drugs—such as opioid painkillers, antacids with aluminum or calcium, antidepressants, iron supplements, and diuretics—may cause constipation.
- Changes in routine: Travel, pregnancy, aging, or stress can affect bowel habits.
- Medical conditions: Underactive thyroid, diabetes, irritable bowel syndrome (IBS), neurological disorders (e.g., Parkinson’s disease, multiple sclerosis), and structural gastrointestinal problems.
Specific Medical Causes
- Colonic inertia (slow colon transit)
- Pelvic floor dysfunction
- Obstruction (e.g., colorectal cancer, strictures, or hernias)
- Inflammatory bowel disease (though less common)
- Metabolic or endocrine conditions (e.g., hypercalcemia, hypothyroidism)
Constipation and Gut Health
The billions of bacteria residing in the gut play a significant role in bowel movement frequency and consistency. Gut dysbiosis—an imbalance or reduction in beneficial bacterial species—may contribute to sluggish bowel transit and harder stools. Emerging research supports that dietary adjustments and the use of probiotics may improve symptoms for some patients.
Who is at Risk?
Constipation can affect anyone at any age, but certain groups are more susceptible:
- Women (especially during pregnancy and after childbirth)
- Older adults (aging slows digestion and bowel muscle activity)
- Individuals with low-fiber diets
- People with sedentary lifestyles
- Those taking medications known to cause constipation
- People with chronic illnesses affecting nerve or muscle function
Diagnosing Constipation
The diagnosis of constipation involves a detailed medical history, physical examination, and, sometimes, diagnostic tests to rule out underlying causes or complications.
Medical History and Physical Exam
- Review of symptoms, duration, frequency, and stool characteristics
- Assessment of dietary and lifestyle habits
- Medication review
- Physical and rectal examination to check for abnormalities
Diagnostic Tests
- Blood tests (to rule out infections or metabolic disorders)
- Abdominal X-rays or imaging (to check for blockages)
- Colonoscopy or sigmoidoscopy (for structural problems or colorectal cancer screening)
- Anorectal manometry (evaluating rectal muscle strength and coordination)
- Transit studies (measuring how quickly stool moves through the colon)
These tests are typically reserved for severe, chronic, or unexplained cases—especially if there are warning signs such as weight loss, bleeding, or sudden changes in bowel movements.
Complications of Constipation
Untreated or severe constipation can result in complications, most commonly:
- Hemorrhoids: Swollen veins in the rectum due to straining
- Anal fissures: Small tears in the rectal lining
- Fecal impaction: Hard stool lodged in the colon or rectum, sometimes requiring medical removal
- Rectal prolapse: Rectal tissue protrudes from the anus due to repeated straining
- Chronic discomfort and reduced quality of life
How is Constipation Treated?
Treatment depends on the duration and severity of constipation, as well as underlying causes. Most cases are successfully managed with lifestyle changes and, if needed, medications. Chronic or resistant cases may require further evaluation.
Lifestyle and Dietary Changes
- Increase dietary fiber (fruits, vegetables, whole grains, legumes)
- Drink adequate fluids (mainly water; avoid excess caffeine and alcohol)
- Increase physical activity (regular exercise boosts gut motility)
- Establish a regular bathroom routine and respond promptly to the urge to go
- Consider probiotics or fermented foods (yogurt, kefir, kimchi)
Medications and Medical Treatment
- Bulk-forming laxatives: Psyllium, methylcellulose (increase stool volume—must be taken with adequate fluids)
- Osmotic laxatives: Polyethylene glycol, lactulose, magnesium hydroxide (draw water into colon)
- Stool softeners: Docusate (moisten stool for easier passage)
- Stimulant laxatives: Senna, bisacodyl (stimulate bowel contractions; for short-term use when other measures fail)
- Lubricant laxatives: Mineral oil (rarely used; caution for aspiration risk)
- Prescription medications: Prucalopride, lubiprostone, linaclotide, or plecanatide (for chronic or resistant cases)
- Treatment of underlying causes: Adjust or change constipating medications, treat metabolic or neurological conditions
Non-Medication Approaches
- Biofeedback therapy (train pelvic floor muscles for coordinated defecation)
- Behavioral therapy and counseling (especially beneficial for children)
- Surgical intervention (rare and reserved for severe, unresponsive constipation due to structural problems)
Prevention of Constipation
- Eat a balanced diet high in fiber
- Drink enough fluids daily
- Exercise regularly
- Heed your body’s signals—do not ignore the urge to have a bowel movement
- Develop a consistent bathroom routine
- Limit constipating medications when possible (consult with your healthcare provider)
When to Seek Medical Care?
- Constipation does not improve with diet and lifestyle changes
- Symptoms persist for three weeks or more
- There is unexplained weight loss or loss of appetite
- Stools are thin, pencil-like, or you see blood
- Severe abdominal pain, nausea, or vomiting
- Family history of colorectal cancer or inflammatory bowel disease
Prompt evaluation ensures that underlying or serious conditions (such as colorectal cancer, metabolic or neurologic disorders) are not missed.
Living with Chronic Constipation
Chronic constipation may require long-term lifestyle and dietary changes, periodic medical evaluation, and sometimes ongoing medication. Many find relief through multidisciplinary approaches involving gastroenterologists, dietitians, and behavioral therapists. Support and education can reduce frustration and help patients regain control over daily life.
Tips for Relieving and Preventing Constipation
- Establish regular mealtimes to stimulate natural digestive rhythms
- Create a bathroom routine, preferably after meals
- Do not ignore bowel movement urges
- Use a footstool to elevate feet while sitting on the toilet—this can help align the colon and make passage easier
- Stay active: even light walking increases gut motility
- Talk to your doctor if current medications might be contributing
Table: Common Medications That Can Cause Constipation
| Medication Class | Examples |
|---|---|
| Opioids | Morphine, codeine, oxycodone |
| Antacids (aluminum or calcium-based) | Calcium carbonate, aluminum hydroxide |
| Iron supplements | Ferrous sulfate, ferrous gluconate |
| Antidepressants | Tricyclics (amitriptyline, nortriptyline) |
| Antihistamines | Diphenhydramine, loratadine |
| Diuretics | Thiazides, furosemide |
Frequently Asked Questions (FAQs)
Q: When is constipation considered a medical emergency?
A: Seek immediate medical attention if constipation is accompanied by severe pain, vomiting, inability to pass gas or stool, blood in the stool, or sudden significant changes in bowel habits.
Q: What dietary changes are most effective for relieving constipation?
A: Gradually increase fiber intake with fruits, vegetables, whole grains, and drink more fluids. A daily goal of 20-35 grams of dietary fiber is recommended for most adults.
Q: How important is exercise in preventing constipation?
A: Exercise stimulates natural contractions of intestinal muscles, making regular physical activity a cornerstone of prevention and remedy for constipation.
Q: Can stress cause constipation?
A: Yes, psychological stress and anxiety may alter gut motility through the gut-brain axis, leading to or worsening constipation in some people.
Q: Are over-the-counter laxatives safe?
A: Laxatives can be helpful for short-term use but should not be relied on long-term without medical supervision, as overuse can lead to dependency or worsen certain conditions.
Q: How does aging affect bowel habits?
A: Aging often slows digestion, weakens gut muscles, and increases the likelihood of chronic conditions or medications that can cause constipation. Proactive management is especially important in older populations.
Q: What is fecal impaction and how is it treated?
A: Fecal impaction is a severe form of constipation where stool becomes hard and stuck in the bowel. Treatment may involve manual removal, enemas, and long-term adjustments in diet and lifestyle.
Summary
Constipation is a common yet manageable condition affecting people of all ages. Most cases resolve with healthy dietary and lifestyle changes. For persistent or severe symptoms, seek medical evaluation to ensure a tailored approach, minimize complications, and retain quality of life.
References
- https://wisemindnutrition.com/blog/constipation-gut-health
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5373459/
- https://pure.johnshopkins.edu/en/publications/outcomes-of-combined-medical-and-behavioral-treatments-for-consti
- https://cdhf.ca/en/constipation-and-the-brain-gut-axis/
- https://pure.johnshopkins.edu/en/publications/the-health-related-quality-of-life-and-economic-burden-of-constip-3
- https://www.consultant360.com/articles/constipation-older-adult
- https://dbhds.virginia.gov/wp-content/uploads/2025/04/April-2025-Pt-2-Constipation.pdf
Read full bio of Sneha Tete












