Understanding Celiac Disease: Symptoms, Causes, Diagnosis, and Care
A comprehensive resource exploring the causes, symptoms, diagnosis, treatment, and daily life impact of celiac disease.
Understanding Celiac Disease
Celiac disease is a chronic autoimmune condition triggered by gluten that affects the digestive system, leading to inflammation and damage of the small intestine. With growing awareness of food intolerances and autoimmune disorders, understanding celiac disease is crucial for patients, caregivers, and the general public alike. This article delivers comprehensive information about the causes, symptoms, diagnosis, treatment, and daily management of celiac disease.
What Is Celiac Disease?
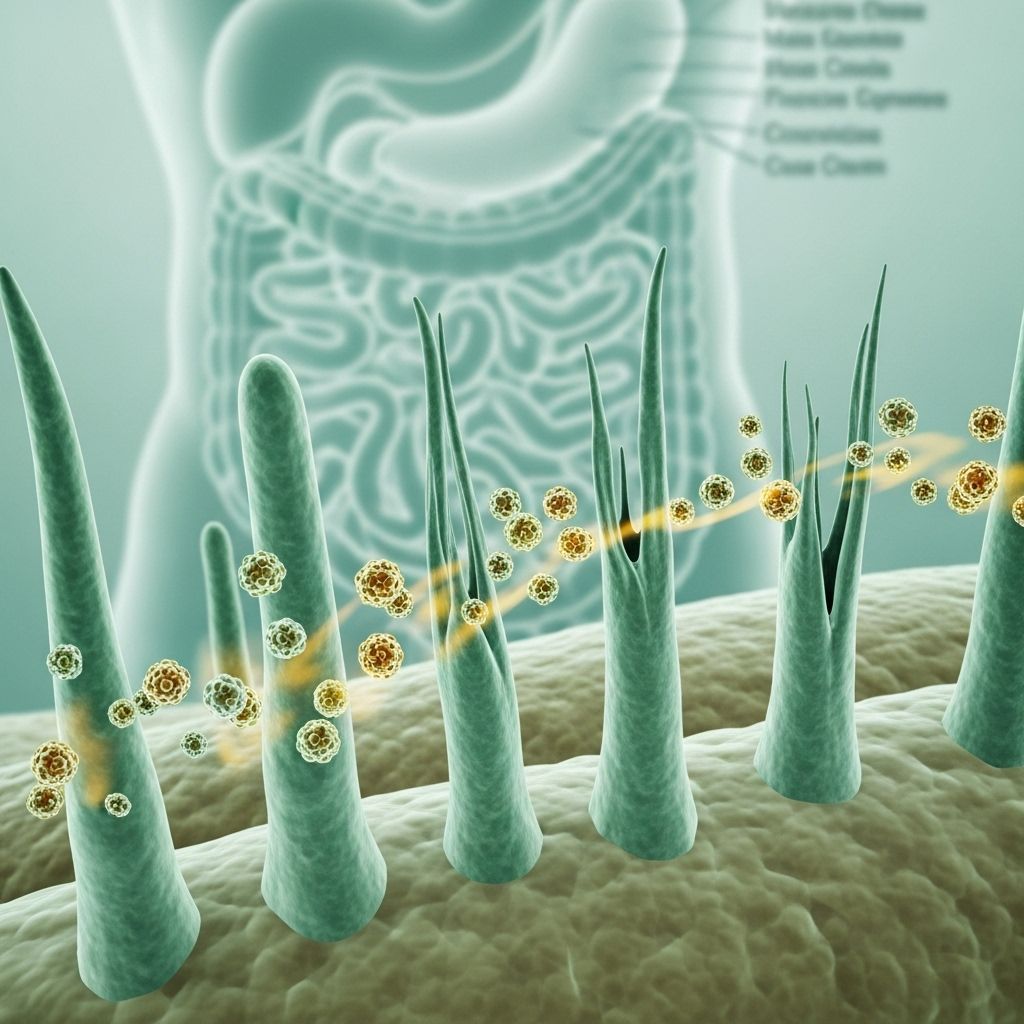
Celiac disease is an autoimmune disorder where the ingestion of gluten, a protein present in wheat, rye, and barley, causes damage to the lining of the small intestine. People with this condition experience an abnormal immune reaction to gluten, resulting in chronic inflammation and the flattening of the villi — tiny, finger-like projections that absorb nutrients from food. This damage impairs nutrient absorption, which can have widespread effects throughout the body.
- Celiac disease can develop at any age after people begin consuming foods or medicines that contain gluten.
- Once it develops, it persists for life. There is no cure, but proper management can control symptoms and prevent complications.
- It is distinct from wheat allergy and non-celiac gluten sensitivity, both of which involve different immune mechanisms.
Gluten and Its Role in Celiac Disease
Gluten refers to a group of proteins found primarily in wheat, barley, and rye. In people with celiac disease, gluten triggers an immune response that causes the immune system to attack the lining of the small intestine.
- Common sources include bread, pasta, cereals, baked goods, beer, and some processed foods.
- Even tiny amounts of gluten—sometimes hidden in sauces, dressings, or medications—can provoke significant damage in those with celiac disease.
Symptoms of Celiac Disease
The way celiac disease presents can differ significantly between individuals. Some people experience classic digestive symptoms, while others may have subtle or no symptoms at all.
Digestive Symptoms:
- Diarrhea
- Abdominal pain and bloating
- Unexplained weight loss
- Constipation
- Loss of appetite
- Nausea and vomiting
- Fatty, foul-smelling stools (steatorrhea)
Non-Digestive Symptoms:
- Fatigue or feeling tired all the time
- Anemia (especially iron-deficiency anemia)
- Bone or joint pain
- Osteoporosis or osteopenia (bone thinning)
- Itchy skin rash (dermatitis herpetiformis)
- Dental enamel defects
- Headaches or migraines
- Tingling or numbness in hands and feet
- Infertility or miscarriages
- Short stature or delayed growth in children
Some individuals may have silent celiac disease, where there are no clear symptoms but there is still measurable damage to the small intestine.
Causes and Risk Factors
Celiac disease results from a combination of genetic and environmental factors. The key triggers, as well as risk factors, are described below:
- Genetic predisposition: Most people with celiac disease carry one or both of the genes HLA-DQ2 and HLA-DQ8.
- Immune response: The immune system erroneously attacks gluten and, as a result, the small intestine.
- Environmental factors: Infections and changes in gut microbiome may influence disease onset in those genetically susceptible.
Who Is at Higher Risk?
- Immediate family members of people with celiac disease (parent, child, sibling)
- People with other autoimmune conditions (such as type 1 diabetes, autoimmune thyroid disease)
- Individuals with Down syndrome, Turner syndrome, or Williams syndrome
- Caucasians and people of European ancestry, although celiac disease occurs globally
Complications of Untreated Celiac Disease
If left undiagnosed or unmanaged, celiac disease can lead to serious and sometimes irreversible health complications:
- Malnutrition due to chronic nutrient malabsorption
- Anemia (iron, folate, or vitamin B12 deficiency)
- Osteoporosis and bone fractures
- Liver disorders
- Neurological symptoms (peripheral neuropathy, seizures)
- Increased risk of certain cancers, such as intestinal lymphoma
- Problems with fertility and pregnancy
Diagnosis of Celiac Disease
Diagnosing celiac disease begins with a thorough medical history and physical examination, especially when symptoms include unexplained diarrhea, weight loss, and nutritional deficiencies. Accurate diagnosis generally involves a combination of blood tests and small intestine biopsies.
Common Steps in Diagnosis:
- Blood Tests: These include screening for specific antibodies (such as anti-tissue transglutaminase—tTG—and anti-endomysial antibodies).
- Biopsy: If blood tests are positive or highly suspicious, an endoscopic biopsy of the small intestine is performed to look for villous atrophy and confirm the disease.
- Genetic Tests: May be used to look for HLA-DQ2 or HLA-DQ8 genes, especially in ambiguous cases.
Important: Individuals should remain on a normal (gluten-containing) diet during testing, since eliminating gluten in advance may cause misleading (false-negative) results.
Treatment and Management
The only proven treatment for celiac disease is a lifelong, strict gluten-free diet. Adherence to this diet allows the small intestine to heal, symptoms to resolve, and risk of complications to decrease substantially.
The Gluten-Free Diet: Core Principles
- Avoid all foods and beverages containing wheat (including spelt, farro, durum, semolina), barley, rye, and related grains.
- Read food labels carefully for hidden sources of gluten.
- Watch for gluten in processed foods, sauces, salad dressings, soups, and some medications or supplements.
- Opt for naturally gluten-free foods: fruits, vegetables, fresh meats and fish, eggs, beans and legumes, most dairy products, potatoes, rice, corn, quinoa, and certified gluten-free grains and flours.
Tips for Safe Gluten-Free Eating
- Cook from scratch when possible to control ingredients.
- Use dedicated kitchen tools and appliances to prevent cross-contact at home.
- When eating out, ask questions about food preparation and request gluten-free menu options.
- Work with a registered dietitian knowledgeable in celiac disease for nutrition guidance.
Medical Follow-Up and Support
- Regular follow-up with healthcare providers is necessary to monitor symptom resolution and nutritional status.
- Blood tests may be repeated to assess antibody levels and check for deficiencies (iron, calcium, vitamin D, vitamin B12, folate).
- Bone density scans may be recommended, especially for adults with initial evidence of bone loss or those at risk.
- Vaccinations (such as pneumococcus and hepatitis B) may be advised if the spleen is affected.
Living with Celiac Disease
Adapting to a gluten-free lifestyle can be challenging, especially at first. However, with the right strategies and support, people with celiac disease can thrive.
Coping Strategies
- Educate yourself and your family about sources of gluten.
- Consult gluten-free recipe books and online resources.
- Explore support groups for shared tips, recipes, and encouragement.
- Plan ahead for travel, special occasions, and social gatherings.
- Communicate with schools, workplaces, and care providers to ensure a safe environment.
Common Challenges
- Social situations involving shared food or uncertainty about ingredients.
- Traveling and eating out safely.
- Hidden sources of gluten in medications or personal care products.
- Costs of gluten-free products, which may be higher than their gluten-containing counterparts.
Special Considerations and Related Conditions
Celiac disease frequently co-occurs with other autoimmune conditions. One notable relationship is with Type 1 diabetes. Both conditions share common genetic markers and can influence one another’s management, particularly regarding diet and nutritional balance. Additional screening for celiac disease is often recommended for people with Type 1 diabetes and vice versa.
Other conditions seen more often in people with celiac disease:
- Autoimmune thyroid diseases (such as Hashimoto’s or Graves’)
- Liver autoimmune diseases
- Selective IgA deficiency
Table: Foods to Avoid and Safe Foods in a Gluten-Free Diet
| Foods to Avoid | Safe Foods |
|---|---|
| Bread, pasta, cereals made from wheat, barley, rye, spelt, and triticale | Rice, corn, quinoa, millet, potato, certified gluten-free oats |
| Baked goods (cakes, cookies, pastries) with wheat flour | Gluten-free bakery items (labeled GF) |
| Beer, malt beverages | Wine, distilled spirits, gluten-free beer |
| Soups, sauces, and salad dressings thickened with wheat | Homemade soups, dressings without gluten-containing ingredients |
| Processed meats (unless labeled gluten-free) | Plain meat, poultry, fish, eggs |
Frequently Asked Questions (FAQs)
Q: What is the difference between celiac disease, wheat allergy, and gluten sensitivity?
A: Celiac disease is an autoimmune reaction to gluten causing small intestine damage, wheat allergy is an allergic response to wheat proteins with rapid-onset symptoms, and non-celiac gluten sensitivity involves symptoms triggered by gluten without intestinal damage or specific antibodies.
Q: Is celiac disease curable?
A: There is currently no cure for celiac disease. Symptoms and intestinal damage can be managed and typically reversed with a strict gluten-free diet.
Q: Is it possible to develop celiac disease later in life?
A: Yes, celiac disease can develop at any age, including adulthood, even in those who previously consumed gluten without apparent issues.
Q: Are oats safe on a gluten-free diet?
A: Pure, uncontaminated oats are naturally gluten-free. However, most commercial oats are contaminated with gluten during processing, so only oats labeled as gluten-free should be consumed.
Q: Can children “outgrow” celiac disease?
A: No, celiac disease is lifelong. Even if symptoms appear to resolve, returning to a gluten-containing diet will cause intestinal damage to resume.
When to Consult a Doctor
See a healthcare professional if you experience ongoing digestive problems, persistent fatigue, unexplained weight loss, anemia, or have a close family member with celiac disease. Early diagnosis and strict gluten avoidance can dramatically improve health and quality of life.
Resources and Support
- Registered dietitian specializing in celiac disease
- Celiac disease support groups (local or online)
- National organizations such as the Celiac Disease Foundation and National Celiac Association
- Educational resources and gluten-free product guides
Effective management, regular checkups, and reliable information can help people with celiac disease enjoy healthy, active, and fulfilling lives. Staying informed and vigilant is the best protection against the challenges posed by this lifelong condition.
References
Read full bio of Sneha Tete












