Understanding Candidiasis: Causes, Symptoms, Diagnosis & Treatment
Comprehensive guide to symptoms, causes, diagnosis, prevention, and treatment of candidiasis yeast infections across the body.
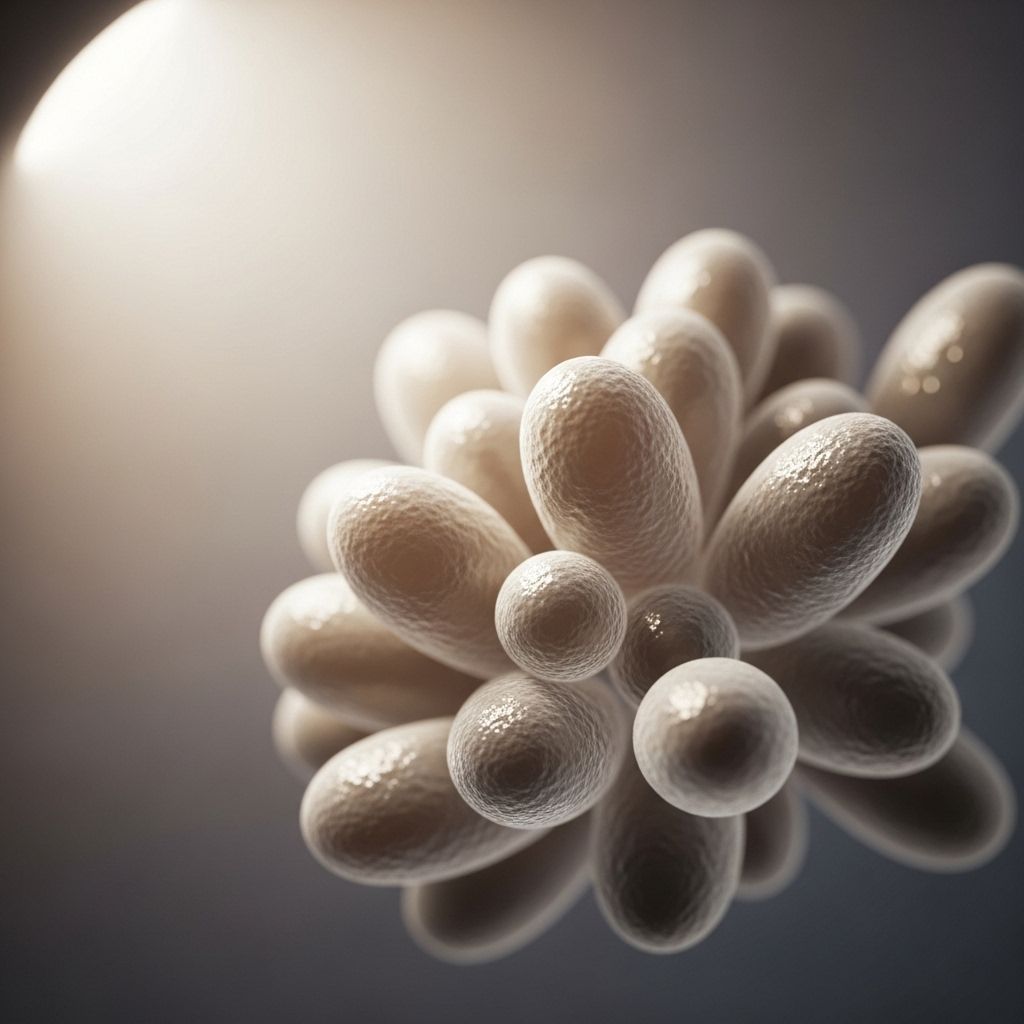
Candidiasis (Yeast Infection) Overview
Candidiasis, also known as a yeast infection, is caused by the overgrowth of Candida species—a type of fungus that naturally inhabits the human body. Under optimal conditions, Candida remains under control through a balance of healthy bacteria and immune defenses. However, disruptions to this balance can enable Candida to multiply, leading to infection in various areas such as the mouth, throat, vagina, skin, and systemic organs in severe cases.
Candidiasis most commonly affects women as vaginal yeast infections, but infections can also occur in men and in people of all ages, impacting different body sites.
Types of Candidiasis
- Vaginal candidiasis (vaginal yeast infection)
- Oral thrush (mouth and throat infection)
- Candidiasis of the skin (cutaneous infection)
- Esophageal candidiasis
- Invasive candidiasis (systemic infection affecting organs or bloodstream)
Causes of Yeast Infections
Candida typically resides on the skin, mouth, gut, and genitals without triggering symptoms. Factors that disrupt this balance can allow the fungus to cause infection by growing too much.
- Antibiotic use – kills beneficial bacteria that keep Candida in check
- Pregnancy – hormonal changes affect vaginal environment
- Uncontrolled diabetes – increased sugar in body fluids can fuel yeast growth
- Immune system deficiency – increases susceptibility, especially in HIV/AIDS or cancer
- High estrogen levels – contraceptives or hormone treatments may raise risk
- Poor hygiene or damp environments – promotes fungal growth on skin folds
- Sexual activity – rarely transmitted sexually, but possible in female partners
- Other medical conditions – autoimmune or chronic illnesses disrupt balance
Symptoms of Candidiasis
The symptoms of candidiasis depend on the location and severity of infection. Some infections may be mild or even asymptomatic, while others cause substantial discomfort or complications.
Common Symptoms by Body Area
| Type | Typical Symptoms |
|---|---|
| Vaginal Candidiasis |
|
| Oral Thrush |
|
| Esophageal Candidiasis |
|
| Skin Candidiasis |
|
| Invasive Candidiasis |
|
Complications & Special Cases
- Recurrent yeast infections (defined as four or more episodes per year) may indicate underlying issues such as diabetes, immune compromise, or non-albicans Candida species.
- Men can also develop candidiasis (balanitis) on the penis, presenting as irritation, redness, and discharge.
- Severe infection can lead to skin fissures, sores, or systemic illness in immunocompromised patients.
Diagnosis of Candidiasis
Diagnosis typically relies on a combination of physical examination, discussion of symptoms, and laboratory testing.
- For vaginal candidiasis: A sample of vaginal discharge may be collected for microscopic examination or culture.
- Oral thrush: Diagnosis can often be made visually by the doctor based on appearance of lesions.
- Other sites or severe cases: Additional lab tests, cultures, or biopsies might be required to confirm the species and extent of Candida infection.
It’s important for healthcare providers to rule out other conditions (such as sexually transmitted infections in the case of vaginal symptoms) since symptoms can be similar.
Treatment Options for Candidiasis
Treatment depends on the site, severity, underlying risk factors, and whether the infection is recurrent or complicated.
Vaginal Yeast Infection Treatment
- Most vaginal yeast infections are effectively treated with antifungal medications, available as:
- Topical creams/ointments (e.g. miconazole, clotrimazole, terconazole)
- Suppositories (placed inside vagina)
- Oral medications (fluconazole, usually in a single dose)
- Prescription antifungals may be needed for severe or recurrent cases.
- Over-the-counter (OTC) treatments are widely available, but proper diagnosis by a healthcare provider is recommended before use.
Oral and Esophageal Candidiasis Treatment
- Oral thrush: Antifungal oral gel, lozenge, or liquid medication, typically used for 7–14 days (e.g. nystatin, clotrimazole, miconazole)
- Severe oral or esophageal infection: Oral or intravenous antifungal medication (fluconazole, amphotericin B)
Invasive Candidiasis Treatment
- Usually requires hospitalization and intravenous antifungal drugs (echinocandin such as caspofungin, micafungin, or anidulafungin)
- Alternatives: fluconazole, amphotericin B
- Length of treatment depends on infection severity, location, and patient’s immune status
Other Considerations
- Treat underlying risk factors if possible, e.g. control blood glucose in diabetes, review antibiotic use, address immune compromise.
- Healthcare providers may adjust treatment if symptoms don’t improve, worsen, or recur after initial therapy (alternate medications, longer courses).
Complicated or Recurrent Infections
- Longer courses or alternate medication may be needed for infections caused by non-albicans Candida strains or due to underlying medical conditions.
- Consultation with a healthcare provider is crucial for cases not responding to standard treatments.
Prevention of Candidiasis
Practice healthy habits to reduce your risk:
- Maintain good hygiene—keep skin folds, genital area, and mouth clean and dry.
- Limit unnecessary use of antibiotics unless prescribed by your healthcare provider.
- Control blood sugar if you have diabetes.
- Wear loose, breathable clothing and underwear (cotton is best).
- Avoid prolonged damp environments, including wet bathing suits and sweaty gym clothes.
- If prone to vaginal infections, consider avoiding scented feminine hygiene products and douching.
- Follow prescribed treatments for immune conditions closely.
Frequently Asked Questions (FAQs)
Q: Is candidiasis contagious?
A: Most types of candidiasis are not considered contagious, but in rare cases, vaginal yeast infections may be transmitted to a female partner. Transmission to male partners is uncommon.
Q: Can yeast infections recur?
A: Yes. Up to half of women experience more than one vaginal yeast infection in their lifetime, and some suffer recurrent episodes (four or more per year), especially with underlying risk factors such as diabetes, immune disorders, or chronic medical conditions.
Q: What increases my risk for candidiasis?
A: Key risk factors include antibiotic use, pregnancy, uncontrolled diabetes, chronic illness, immune system compromise, hormonal changes, and damp environments. Poor hygiene and certain medications (like corticosteroids) can also raise risk.
Q: How is a yeast infection diagnosed?
A: Diagnosis is usually based on patient history, physical examination of affected area, and laboratory tests (microscopy, culture, or molecular tests) to determine Candida species and rule out other conditions.
Q: Can I treat a yeast infection with over-the-counter medicine?
A: OTC antifungals can treat mild infections, especially vaginal yeast infections. If symptoms are unclear, severe, or recurrent, see a healthcare provider for confirmation and targeted therapy.
Q: When should I see a doctor?
A: Seek medical attention if you experience:
- Severe pain, redness, swelling, or fever
- Frequent or recurrent infections
- No improvement after standard treatment
- Unusual symptoms or immune compromise
Summary Table: Candida Infection Sites & Treatments
| Body Area | Symptoms | Treatment |
|---|---|---|
| Vagina | Itching, burning, thick discharge | OTC/topical antifungals, oral fluconazole |
| Mouth (Oral Thrush) | White plaques, soreness | Antifungal oral gel or lozenges |
| Skin | Red, itchy rash in folds | Topical antifungals, keep skin dry |
| Esophagus | Painful swallowing | Oral or IV fluconazole |
| Bloodstream/Organs (Invasive) | Fever, systemic symptoms | IV echinocandin, fluconazole, amphotericin B |
Living With & Managing Candidiasis
While most cases are mild and treated effectively, candidiasis can disrupt daily life due to discomfort and emotional stress. Follow these general guidelines to manage the condition:
- Take all prescribed medications as directed, and complete the full course.
- Monitor your symptoms; inform your healthcare provider if symptoms persist or worsen.
- Practice preventive hygiene, make healthy lifestyle choices, and control relevant medical conditions.
- Discuss with your provider about maintenance or suppressive therapy for recurrent infections.
Speak to a medical professional for personalized recommendations based on your unique circumstances.
Additional Resources
- Centers for Disease Control and Prevention (CDC): Candidiasis Information
- Cleveland Clinic: Yeast Infection and Candidiasis Care Guides
- Medical News Today: Yeast Infection Causes, Symptoms & Treatment Insights
References
- https://my.clevelandclinic.org/health/diseases/5019-vaginal-yeast-infection
- https://my.clevelandclinic.org/health/diseases/23198-candidiasis
- https://www.medicalnewstoday.com/articles/151172
- https://www.cdc.gov/candidiasis/treatment/index.html
- https://www.mayoclinic.org/diseases-conditions/yeast-infection/symptoms-causes/syc-20378999
- https://www.healthline.com/nutrition/candida-symptoms-treatment
- https://www.uchealth.org/diseases-conditions/yeast-infection/
- https://www.ncbi.nlm.nih.gov/books/NBK560624/
Read full bio of medha deb












