Understanding Back Pain: Causes, Symptoms, Diagnosis & Treatments
An in-depth overview of back pain including its causes, diagnosis, treatment options, prevention strategies, and tips for living well with this common condition.
Understanding Back Pain
Back pain is a prevalent condition that affects millions of people each year, often interfering with daily activities, work, and overall quality of life. It can range from mild discomfort to severe, disabling pain. Knowing the causes, recognizing symptoms, understanding diagnostic methods, and exploring treatment options can empower individuals to take charge of their back health and seek timely care.
What is Back Pain?
Back pain refers to any ache, discomfort, or stiffness felt along the back, ranging from the upper and middle back down to the lower (lumbar) region. While most people experience lower back pain, any part of the back may be affected. The condition can manifest suddenly (acute) due to injury or strain, or it can persist over a long time (chronic).
Types of Back Pain
- Acute Back Pain: Lasts a few days to weeks, often resulting from sudden injury, muscle strain, or poor posture.
- Chronic Back Pain: Persists for 12 weeks or longer, even after initial injury or underlying cause has been treated.
Symptoms of Back Pain
Back pain symptoms can differ widely from person to person. Some of the most common symptoms include:
- Aching or stiffness along the spine, especially after activity or prolonged sitting.
- Sharp, localized pain in the neck, upper back, or lower back, often after lifting objects or sudden movement.
- Radiating pain that moves down the legs, possibly indicating nerve involvement (such as sciatica).
- Difficulty standing straight or decreased mobility.
- Muscle spasms in the back or hips.
In some cases, back pain may be accompanied by symptoms such as numbness, tingling, or weakness in the legs. These symptoms may suggest nerve irritation or compression and require prompt medical evaluation.
When to Seek Medical Attention
- Severe or worsening pain that does not improve with rest or self-care
- Pain that radiates down the leg, especially below the knee
- Numbness, tingling, or weakness in one or both legs
- Difficulty with bladder or bowel control
- Pain following a traumatic injury (fall, accident)
- Unexplained weight loss, fever, or night sweats associated with back pain
These symptoms could indicate a serious underlying condition such as nerve damage, infection, or cancer requiring immediate medical evaluation.
Causes of Back Pain
There are many different causes of back pain. Understanding the source is essential in selecting an appropriate treatment plan. The three main categories are:
- Mechanical Causes: Involves the muscles, ligaments, and joints
- Spinal Structure Damage: Affects the bones (vertebrae) and discs
- Nerve Involvement: Pain caused by irritation or compression of spinal nerves
| Category | Examples |
|---|---|
| Mechanical | Muscle strains, ligament sprains, posture issues |
| Structural | Herniated discs, osteoarthritis, vertebral fractures, scoliosis |
| Nerve Involvement | Sciatica, spinal stenosis, nerve root compression |
Common Causes of Back Pain
- Muscle or Ligament Strain: Most common cause, often due to heavy lifting, repetitive twisting, or sudden awkward movements.
- Bulging or Ruptured Discs: Discs act as cushions between vertebrae. When they bulge or rupture, they can press on nearby nerves, causing pain.
- Arthritis: Osteoarthritis commonly affects the lower back. In some cases, spinal arthritis can lead to narrowing of the space around the spinal cord (spinal stenosis).
- Osteoporosis: Makes bones brittle and prone to compression fractures.
- Structural Irregularities: Conditions like scoliosis where the spine curves abnormally.
- Degenerative Disc Disease: Discs lose hydration and flexibility, causing pain.
- Infections, cancer, or inflammatory diseases: Less common, but possible causes of persistent back pain.
Risk Factors for Back Pain
Several factors can increase the risk of developing back pain:
- Age—risk increases with age, particularly after 30 or 40
- Lack of exercise—weak, unused muscles in the back and abdomen
- Excess weight—increases strain on the back
- Improper lifting technique—using your back instead of your legs
- Certain diseases or conditions—arthritis, cancer, or spinal problems
- Smoking—impairs blood flow to spinal tissues
- Prolonged sitting or poor posture
- Psychological conditions—anxiety, depression, or stress may contribute
Diagnosis: How is Back Pain Assessed?
Diagnosing back pain begins with a comprehensive medical history and physical exam. Physicians look for clues to pinpoint the origin of the pain and to rule out serious conditions.
Key Steps in Diagnosis
- Medical History: Discussion of when the pain started, its location, intensity, aggravating/alleviating factors, prior treatments, and related symptoms.
- Physical Examination: Assessment of strength, flexibility, reflexes, sensation, and mobility—sometimes involving special maneuvers to reproduce pain or check for nerve function (e.g., straight leg raise test).
Possible Diagnostic Tests
- X-rays: Can reveal bone problems like fractures or arthritis.
- MRI (Magnetic Resonance Imaging) or CT scans: Used to visualize soft tissues, such as discs or nerves, and to assess herniated discs or spinal stenosis.
- Bone scans: Sometimes used to detect infection, fractures, or tumors.
- Electrodiagnostic tests (EMG): Assess nerve function for suspected nerve compression.
Most cases of back pain do not require advanced imaging or testing unless there are “red flag” warning signs, such as severe neurological symptoms, trauma, or suspected systemic illness.
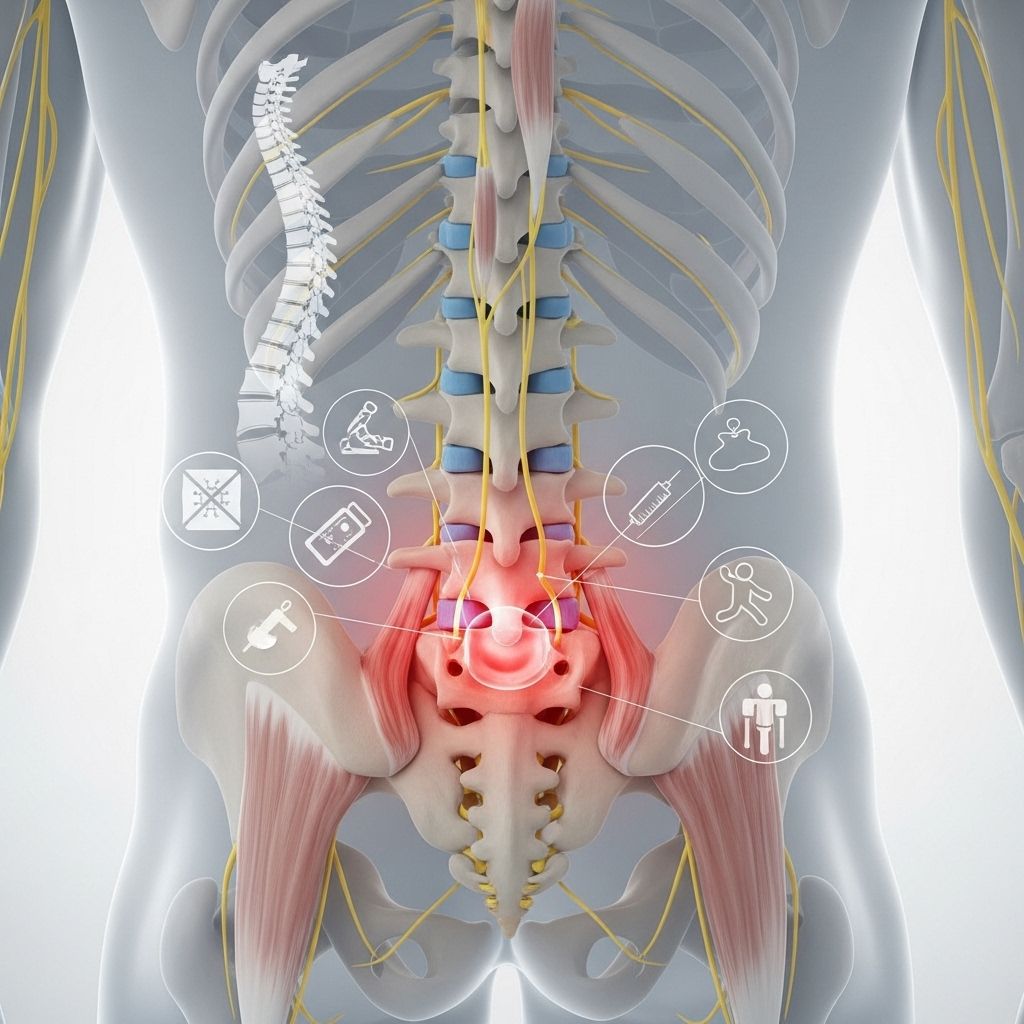
Back Pain Treatments
Treatment plans depend on the severity, underlying cause, and duration of pain. Most people recover with self-care, but persistent or severe pain may require medical intervention.
Self-Care and Home Remedies
- Short Rest: Brief bedrest (not prolonged) for acute pain may be helpful, but early gradual movement is encouraged.
- Heat/Ice Packs: Applied to the affected area can help relieve pain and reduce inflammation.
- Over-the-Counter Medications: Such as acetaminophen, ibuprofen, or naproxen to relieve pain and reduce inflammation.
- Gentle Movement: Early return to normal activities—as tolerated—promotes faster recovery.
Medical Treatments
- Physical Therapy: Exercise, stretching, strengthening, and postural training tailored to the patient’s needs.
- Prescription Medications: Such as muscle relaxants, anti-inflammatory drugs, or in rare cases, opioids for short-term use.
- Injections: Corticosteroid injections or nerve blocks may provide relief for inflammation or nerve-related pain.
- Manual Manipulation: Chiropractic or osteopathic spinal manipulation in some cases.
- Psychological Counseling: For chronic pain, cognitive-behavioral therapy helps manage pain perception and stress.
Surgical Treatments
Surgery is considered a last resort, usually reserved for structural problems that cause persistent pain, neurological deficits, or when other treatments have failed. Common procedures include:
- Discectomy: Removing part of a herniated disc to relieve nerve pressure.
- Laminectomy: Removing bone to relieve spinal stenosis (narrowed spinal canal).
- Spinal Fusion: Joining two or more vertebrae to increase stability.
Alternative and Complementary Treatments
- Acupuncture
- Massage Therapy
- Yoga and Tai Chi
- Mindfulness and relaxation techniques
While some patients experience benefits from alternative therapies, their effectiveness varies and should be discussed with a healthcare provider to ensure safety and compatibility with other treatments.
Prevention: How to Protect Your Back
Taking steps to prevent back pain can reduce the risk of future injuries and improve overall back health. Essential prevention strategies include:
- Engage in regular low-impact exercise (walking, swimming, or cycling)
- Strengthen your core (abdominal and back muscles) through focused exercises
- Maintain a healthy weight to reduce stress on the back
- Practice proper lifting techniques—lift with your legs, not your back
- Use ergonomically designed chairs and workspaces
- Maintain good posture while sitting and standing
- Take frequent breaks to stretch, especially if sitting for long periods
- Stop smoking to improve blood flow and healing to spinal tissues
Living with Chronic Back Pain
Chronic back pain can significantly affect daily activities, mood, relationships, and overall well-being. People living with ongoing back pain can benefit from:
- Multidisciplinary care involving pain specialists, physical therapists, and mental health professionals
- Adjusting activity levels appropriately—remaining as active as possible
- Building a support system among family, friends, or support groups
- Learning coping strategies for pain, such as mindfulness, deep breathing, and stress management
- Setting realistic goals for managing pain and maintaining function
Frequently Asked Questions (FAQs)
What causes most cases of back pain?
Most cases result from muscle or ligament strain due to heavy lifting, awkward movements, or overuse. Structural problems with discs and joints also contribute, but less often.
When should I see a doctor for back pain?
Seek medical attention if you have severe pain, pain following trauma, numbness, weakness, or difficulty with bladder or bowel control. If back pain lasts longer than a few weeks or worsens, consult a health professional.
Can exercise really help back pain?
Yes, specific exercises can strengthen the muscles supporting the spine and relieve pressure. Physical therapy is highly effective for many types of back pain.
Is surgery necessary for most cases?
No, surgery is typically a last resort for severe cases involving nerve compression or structural instability. Most people recover with conservative treatments.
How can I prevent back pain from returning once it’s gone?
Regular exercise, good posture, maintaining a healthy weight, and avoiding heavy lifting or repetitive strain are key to preventing recurrence.
References
- https://www.youtube.com/watch?v=QRwCzu0T4Q4
- https://www.press.jhu.edu/books/title/10099/get-your-lower-back-pain-under-control-and-get-life
- https://pure.johnshopkins.edu/en/publications/an-update-of-comprehensive-evidence-based-guidelines-for-interven-3
- https://hopkinscme.cloud-cme.com/default.aspx?P=0
- https://publichealth.jhu.edu/2012/healthy-monday-2012/02202012_back-pain
Read full bio of medha deb












