Understanding Atherosclerosis: Causes, Risks, Diagnosis, and Management
Learn how atherosclerosis develops, its risk factors, symptoms, diagnosis, prevention, and the latest strategies for management.
Atherosclerosis Overview
Atherosclerosis is a progressive condition affecting the arteries, leading to the buildup of fatty deposits—known as plaques—on the inner walls of these blood vessels. Commonly referred to as “hardening of the arteries,” this disease undermines the flexible, healthy function of arteries and dramatically increases the risk of heart attack, stroke, and peripheral vascular disease.
Over time, plaques can restrict blood flow, reduce oxygen delivery to tissues, and cause serious, sometimes life-threatening complications.
What is Atherosclerosis?
- A chronic condition involving the accumulation of fat, cholesterol, calcium, and other substances (collectively called plaques) inside arteries.
- Plaque buildup stiffens and narrows arteries, impeding blood flow and putting vital organs at risk.
- This process begins subtly and may take decades to produce symptoms.
- Atherosclerosis is a key underlying cause for major cardiovascular events such as heart attacks and strokes.
Alternative Names
- Hardening of the arteries
- Arteriosclerosis
- Plaque buildup – arteries
- Hyperlipidemia – atherosclerosis
- Cholesterol – atherosclerosis
Causes of Atherosclerosis
The development of atherosclerosis is multifactorial, with several contributing systemic and behavioral risk factors influencing onset and progression.
While aging remains a major risk, lifestyle and genetic factors play critical roles.
- High cholesterol levels: Excessive amounts of LDL (‘bad’ cholesterol) encourage plaque formation at younger ages, especially with diets high in saturated and trans fats.
- Diabetes: Poorly controlled blood sugar accelerates damage to blood vessel walls, fostering plaque buildup.
- Family history: Genetic predispositions increase susceptibility, particularly if close relatives have heart disease or strokes.
- High blood pressure: Hypertension damages arterial walls and makes plaque buildup more likely.
- Lack of exercise: Sedentary lifestyles contribute to obesity, insulin resistance, and poor lipid profiles.
- Being overweight or obese: Heightens risk by affecting blood pressure, lipids, and glucose metabolism.
- Smoking: Directly injures the endothelium (arterial lining), precipitating atherosclerosis and multiplying overall cardiovascular risk.
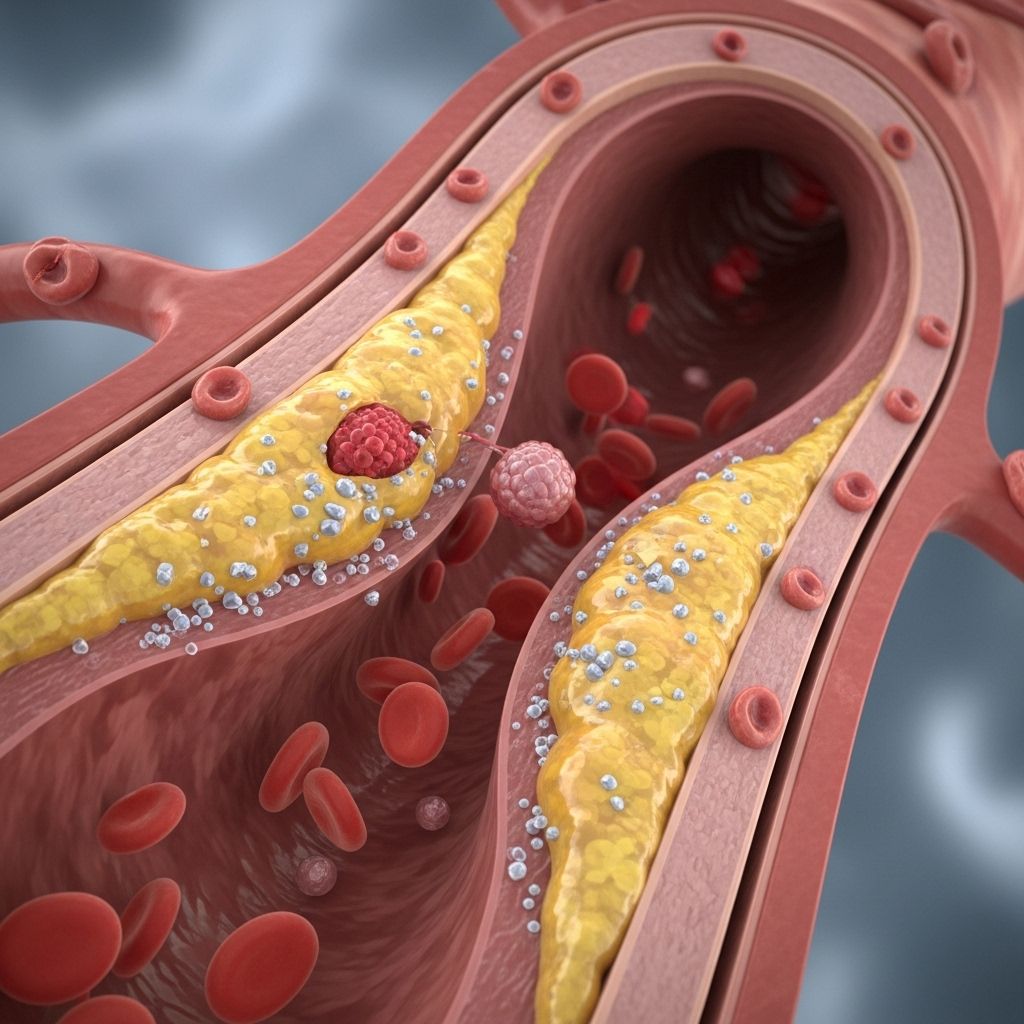
Pathophysiology: How Do Plaques Form?
Atherosclerosis is fundamentally an inflammatory process.
High circulating lipids—like LDL cholesterol—migrate beneath the arterial lining (endothelium), triggering local immune responses.
The following steps outline the general progression:
- Endothelial injury: Risk factors such as hypertension or smoking damage the arterial wall’s inner lining, reducing its protective qualities.
- Lipid infiltration: LDL cholesterol enters the vessel wall, where it is oxidized and attracts immune cells (macrophages and monocytes).
- Foam cell formation: Macrophages absorb oxidized LDL, becoming ‘foam cells.’ These aggregate and form the fatty streaks visible in vessels.
- Plaque maturation: Continued inflammation encourages buildup of smooth muscle cells, connective tissue, and calcium, thickening and hardening the plaque.
- Plaque rupture or thrombosis: Advanced plaques may crack, exposing their inner core. This triggers clot formation, abruptly blocking blood flow and causing heart attacks or strokes.
Symptoms of Atherosclerosis
Most people with atherosclerosis remain unaware until a major artery becomes significantly narrowed or blocked. Symptoms depend on which arteries are affected and how advanced the disease is.
Common Symptom Areas
- Coronary arteries (heart):
- Chest pain (angina)
- Shortness of breath
- Fatigue during exertion
- Heart attack (in severe cases)
- Carotid arteries (brain):
- Sudden weakness/numbness of face, arm, or leg (often on one side)
- Blurred vision
- Difficulty speaking or understanding
- Dizziness, loss of balance
- Stroke symptoms
- Peripheral arteries (legs):
- Pain, cramping, or fatigue in hips, thighs, or calves during walking
- Leg weakness or numbness
- Poor wound healing in feet/toes
- Loss of hair or cool, pale skin on lower extremities
- Renal arteries (kidneys):
- High blood pressure resistant to treatment
- Kidney dysfunction
Clinical Impact and Complications
Atherosclerosis is a system-wide disorder that can compromise any major artery. The most serious complications arise when plaque-related blockages or ruptures occur in arteries serving critical organs.
| Artery Affected | Major Complications |
|---|---|
| Heart (Coronary) | Angina, Myocardial infarction (heart attack), Sudden cardiac death |
| Brain (Carotid/Cerebral) | Transient ischemic attack (TIA), Stroke |
| Legs (Peripheral arteries) | Limb ischemia, Claudication, Potential limb loss |
| Kidneys (Renal arteries) | Kidney failure, Severe hypertension |
| Aorta | Aneurysm formation, Possible rupture (fatal bleeding) |
- Aneurysm formation: Plaques may weaken arterial walls, causing bulges (aneurysms) that risk fatal rupture.
- Thrombosis: Clot formation at a plaque site can completely block blood flow, resulting in tissue death.
- Embolism: Plaque fragments or clots can travel downstream, blocking smaller blood vessels and leading to organ damage.
Risk Factors for Atherosclerosis
A number of modifiable and non-modifiable risk factors make certain individuals more susceptible to developing atherosclerosis. Understanding these risks is crucial to prevention and management.
- Age: Risk increases with age. Plaque buildup is often gradual, starting in childhood and advancing over decades.
- Family history: Genetic predisposition is a notable risk, especially for premature forms (<55 years in men, <65 in women).
- Medical conditions:
- High cholesterol/LDL
- Diabetes
- High blood pressure
- Lifestyle choices:
- Poor diet (high in saturated/trans fats)
- Physical inactivity
- Obesity
- Smoking
Diagnosis of Atherosclerosis
Early detection of atherosclerosis—even before symptoms develop—can greatly reduce risk for major cardiovascular events. Diagnosis typically combines a review of personal risk factors, physical exams, and specialized tests.
Diagnostic Techniques
- Physical examination: Listening for abnormal artery sounds (bruits), checking pulses, and reviewing medical history.
- Blood tests: Assess lipid levels (LDL, HDL, triglycerides), glucose, and markers of inflammation.
- Imaging studies:
- Ultrasound: Checks for arterial narrowing and blood flow disturbances.
- CT scan and MRI: Visualizes artery structure and plaque location.
- Angiography: Dye-injected X-ray identifies blockages.
- Other tests: Exercise stress testing may reveal reduced blood supply to the heart.
Prevention and Lifestyle Strategies
While atherosclerosis cannot be reversed once plaques have formed, its progression can be significantly slowed—even halted—by strategic lifestyle and medical interventions.
Prevention should start early, especially in individuals with family histories or other risk factors.
Core Preventive Measures
- Heart-healthy diet:
- Reduce saturated and trans fats
- Increase fiber and whole grains
- Prioritize fruits and vegetables
- Limit added sugars and processed foods
- Regular physical activity: At least 150 minutes per week of moderate-intensity activity.
- Maintain healthy weight: Achieve and sustain a BMI in the recommended range.
- Control blood pressure and blood sugar: Adhere to medication regimens and dietary guidelines as advised by healthcare providers.
- Quit smoking: Eliminate tobacco use to protect artery lining and overall vascular health.
Treatment and Management
Treatment of atherosclerosis targets both underlying causes and acute symptoms. Interventions are highly individualized and can include lifestyle changes, medication, and sometimes surgical procedures.
Common Treatments
- Lifestyle modification: Central for all patients—diet, exercise, and smoking cessation.
- Medications:
- Statins (lower LDL cholesterol)
- Blood pressure medicines
- Blood sugar control agents (for diabetes)
- Antiplatelet agents (e.g., aspirin) to prevent blood clots
- Surgical procedures (if needed):
- Angioplasty and stent placement to open narrowed vessels
- Coronary artery bypass surgery for severe heart blockages
- Endarterectomy to remove plaques from carotid arteries
Outlook and Prognosis
Atherosclerosis is a lifelong condition. While existing plaque cannot be removed entirely, careful management can prevent progression, reduce complications, and improve long-term wellness.
Individuals who actively adopt preventive measures and adhere to prescribed treatments reduce their risk for heart attack, stroke, kidney failure, and limb loss.
Possible Complications
- Heart attack (myocardial infarction)
- Stroke (cerebrovascular accident)
- Aneurysm (arterial bulge that may rupture)
- Kidney failure
- Limb loss due to critical reduced blood flow
Frequently Asked Questions (FAQs)
Q: Does atherosclerosis only affect older people?
No. Although atherosclerosis is more common with age, it begins early in life, especially in the presence of risk factors such as high cholesterol, diabetes, and hypertension.
Q: Can atherosclerosis be reversed?
Plaques cannot be fully eliminated once established, but disease progression can be slowed or sometimes partially regressed through aggressive lifestyle changes and medical therapy.
Q: Are there warning signs before major events like heart attacks?
Not always. Many individuals have no symptoms until a plaque causes a critical blockage or rupture. Regular screening and risk-factor management are vital for early detection.
Q: Does a healthy diet really make a difference?
Yes. Reducing saturated fat, quitting smoking, and increasing physical activity markedly decrease the risk and slow the progression of atherosclerosis.
Q: What should I do if I have multiple risk factors?
Consult a healthcare provider for a tailored prevention and management plan; medication and structured lifestyle changes are typically needed.
Patient Resources
- American Heart Association: Comprehensive guidance on heart health.
- Centers for Disease Control and Prevention (CDC): Up-to-date statistics and preventive care information.
- Consult your cardiologist or primary physician for individualized risk assessment and monitoring tools.
Key Takeaways
- Atherosclerosis underlies most cardiac and vascular disease, progressing silently over years.
- Lifestyle changes—diet, exercise, quitting smoking—are fundamental to prevention and management.
- Early detection and consistent medical care reduce risks for heart attack, stroke, and other serious complications.
- Every individual’s risk profile is unique; ongoing screening and personalized care are essential.
References
Read full bio of Sneha Tete












